1. Introduction
Pancreatitis is inflammation in the pancreas. The pancreas is a long flat gland that is located in the upper abdomen. It produces enzymes and hormones that help digestion and regulate the glucose processes.
Acute pancreatitis can be divided to two broad categories based on Atlanta classification (1).
-Interstitial edematous acute pancreatitis is characterized by acute inflammation of the pancreatic parenchyma and per pancreatic tissues without recognizable tissue necrosis.
Acute pancreatitis according to severity is divided to the following:
-Mild acute pancreatitis, which is characterized by the absence of organ failure or transient organ failure (lesser than 48 hours) and/or local complications.
-Sever acute pancreatitis, which is characterized by persistent organ failure (greater than 48 hours) that may involve one or multiple organs.
At initial evaluation, the severity of acute pancreatitis should be assessed by clinical examination to assess for early fluid losses, organ failure (particularly cardiovascular, respiratory or renal compromise) measurement of the APACHE2 score, and systematic inflammatory response syndrome (SIRS) score (1, 2). Physical findings vary depending upon the severity of acute pancreatitis. In patients with mild acute pancreatitis, the epigastrium may be minimally painful in palpation. In contrast, in patients with severe pancreatitis, there may be significant tenderness to palpation in the epigastrium.
Patients may have abdominal distention and hypoactive bowel sounds (BS) due to an ileus secondary to inflammation. Patients with severe pancreatitis may have hypoxemia, fever, tachypnea, and hypotension.
In three percent of patients with acute pancreatitis, ecchymosis may be in the periumbilicus (Cullen sign) or the flank (grey turner sign). Patients with severe acute pancreatitis may have dyspnea due to diaphragmatic inflammation secondary to pancreatitis, pleural effusions, or adult respiratory distress syndrome.
Approximately five to ten percent of patients with acute severe pancreatitis may have painless disease and have unexplained hypotension (e.g. dialysis and organophosphate poisoning). Although measurement of lipase and amylase is useful for diagnosis of pancreatitis, serial measurements in patients with acute pancreatic are not useful to predict disease prognosis and severity or for changing the management. Serum amylase rises within 6 to 12 hours of the onset of acute pancreatitis. Amylase has a short half-life of approximately 10 hours and in uncomplicated attacks returns to normal within three to five days. Serum amylase elevation of greater than three times the upper limit of normal has a sensitivity for the diagnosis of acute pancreatitis of 67 to 83 percent and a specificity of 85 to 98 percent. Serum lipase has a sensitivity and specificity for acute pancreatitis ranging from 82 to 100 percent. Serum lipase rises within four to eight hours of the onset of symptoms, peaks at 24 hours, and returns to normal within 8 to 14 days. Lipase elevations occur earlier and last longer as compared with elevations in amylase and are therefore especially useful in patients, who present greater than 24 hours after the onset of pain. Serum lipase is also more sensitive as compared with amylase in patients with pancreatic secondary to alcohol, after the onset of acute pancreatitis (3).
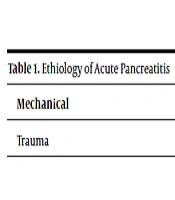
Overall acute pancreatitis is rare in pregnancy, occurring most commonly in the third trimester, and gallstones are the most common cause. When laparoscopic cholecystectomy is not feasible and a common bile duct stone is highly suspected on imaging, endoscopic sphincterotomy or stenting may help prevent recurrence and postpone cholecystectomy until after delivery (Table 1).
| Mechanical | Toxic | Metabolic | Drugs | Infection |
|---|---|---|---|---|
| Trauma | Congenital | Vascular | Miscellaneous | Genetic |
Ethiology of Acute Pancreatitis
2. Case Presentation
In this case report, a 29-year-old pregnant female G3P2 (Gravida 3, Para 2) with gestational age of 31 weeks and three days referred to the maternal ward. Symptoms of this patient were epigastrium pain, RUQ pain, nausea, and vomiting without any delivery (labor pain, PROM, vaginal bleeding) or others sever signs. The vital signs were normal, fetal heart rate was 155 beat per minute and fundal height was normal. The patient did not utilize alcohol or cigarette.
Past medical history (PMH) of the patient showed hyper-lipidemia and gestational diabetic mellitus; she was on a diet for GDM. In her drug history, cholestyramine was prescribed from three days before admission due to rising TG. After admission, the author ordered NPO, N/serum, NGtube, echocardiography, and surgery consultation. Blood Analysis (LFT, Amylase, Lipase, Bun, Cr, CBC, CRP, lipid profile, BS, Na, K, U/A) and abdominal-pregnancy ultrasound was requested
The initial blood analysis showed Amylase = 131, CRP = 96, total cholesterol = 1078, TG = 6036, LFT = Normal, Cr, Bun = NL, CBC (WBC = 14500, HB = 10, PLT = 214000) BS = 177, Cr = 0.9, Na = 13, K = 4, ALT = 14, AST = 17, LDH = 207, Albumin = 3.8, total bitt = 2.5, direct bill = 1.4 and viral marker was normal. Echocardiography showed Nl EF and PAP.
The ultrasound showed multi-locolar collection in pancreas with normal gall bladder and liver. Her pregnancy was 31 - 32 weeks of gestational age, posterior placenta, BPP = 6/8 (Activity = 0).
For this patient, jugular catheter (shaldon) was prepared on the next day and she was undergone plasmapheresis (40 cc/kg) as well as gemfibrozil 600 mg BID, Insulin, and Heparin 5000 IU TDS.
After her first plasmapheresis, TG and total cholesterol showed 2626 and 500, respectively, and, then plasmapheresis was done for the patient six times in total and TG and total cholesterol were decreasing. During this time, pregnancy ultrasound, BPP, and AFI were normal and the fetus was monitored closely many times. The patient was discharged after 21 days at 34 weeks of gestational age and with normal blood analysis (Hb = 11.1, HCT = 33.7, MCV = 94.3, MCH = 29.6, PLT = 27000, PT = 10.5, Cr = 0.6, Na = 136, K = 4.4, total cholesterol = 191, TG < 500, BS = 89, TSH = 1.41, Amylase and lipase = NL). The patient moved to her city in Kerman province (Bam city) and finally delivered at 37 weeks after 21 days of hospitalization. She is completely healthy at present.
3. Discussion
Acute gestational pancreatitis is rarely associated, yet can be caused by important factors, such as maternal mortality and fetal loss. It is generally believed that APIP is associated with several factors (1); gallstone disease or hypertriglyceridemia are the most frequent, and gallstones are amongst top reasons (2). Other reasons, such as Hyperthyroidism (Hyper parathyroidism), connective tissue diseases, infections, and trauma are not the most common causes of acute gestational pancreatitis (3). Acute pancreatitis is explained after medical abortion (4).
Although gallstones are more common causes than hypertriglyceridemia in acute pancreatitis in pregnancy, yet it tends to the severe type in the third trimester (5). Physiological changes in pregnancy, such as overweightness, raised triglycerides, and elevated level of estrogen can increase the incidence of acute pancreatitis in pregnancy (6).
Diagnosis of acute gestational pancreatitis is very difficult, particularly in the first trimester towards the third trimester (6).
Ruptured corpus luteal cyst and ectopic pregnancy are part of differential diagnoses (6). Associations of APIP with HELLP syndrome, preeclampsia, and diabetes mellitus type 2 are important points and can lead to preterm delivery and increase fetal mortality and mobility (7).
Finally, some clinical presentations, namely pain and tenderness in the epigastrium, nausea, vomiting, and abdominal distention led the researchers to characterize pancreatitis; serum amylase and/or lipase were the blood marker for diagnosis. Amylase has severe rise in the first 24 hours and falls down to baseline in three to five days.
Instead, serum lipase remained in the upper normal limit steadily for two weeks. However, there are no differences in both of them for diagnosis (8, 9). However, amylase level is not associated with severity (7). The second step is imaging for discovery of the etiology. Abdominal ultrasound and endoscopic ultrasound are useful for diagnosis of APIP with no more additive rise because of X-ray radiation (9). Computed tomography, magnetic resonance cholangiopancreatography (MRCP), and endoscopic retrograde cholangiopancreatography (ERCP) are not routine, and should carefully be used case by case (9). Ultimately, the type of pancreatitis should be determined in mild acute pancreatitis (MAP) does not have organ failure and systemic complications recover before long yet in severe acute pancreatitis (SAP), it is presented by permanent organ failure (10).
For APIP, collective bargaining is an expected therapy except in pancreatic abscess or infected effusion or gastrointestinal perforation or the condition deteriorates after active treatment. The best time for surgical intervention is the second trimester that is associated with the least complications (10). Another indication of surgery during pregnancy is the presence of cholangitis (11) that has been identified cholecystectomy during the second trimester, which has no additive risk for the mother and the fetus.
For the current patient after primary study, the researchers understood that amylase = 131, cholesterol = 1078, TG = 6036 and the ultrasound showed normal gallbladder and liver. As a consequence, the researchers decided to try conservative treatment. Therefore, plasmapheresis (40 cc/kg) was done six times in total and then TG and cholesterol were decreased. Meanwhile, gemfibrozil 600 mg BID, insulin, and Heparin 5000 IU TDS were ordered. With sever acute pancreatitis diagnosis, the researchers started Total Parental Nutrition (TPN) and hospitalized the patient NPO for 21 days. Many studies have shown that in mild acute pancreatitis (MAP), nutritional support is not recommenced and low fat diet can be used in the first week (12).
Advising antibiotics in sever acute pancreatitis is controversial and the researchers did not use it in this case. There is no more evidence for using antibiotics in mild acute pancreatitis (13).
For the current patient, two other similar cases were reported before by hypertriglyceridemia-induced AP. It is recommended to treat her by plasmapheresis and she was discharged after 21 days from hospitalization in 34 weeks of gestational age and ultimately she delivered at 37 weeks.