1. Background
Multiple sclerosis (MS), is a chronic inflammatory neurodegenerative disorder in which the insulating coats of nerve cells in the brain and spinal cord are damaged [1]. MS is 2 - 3 times more common in women than in men [2]. The disorder is most commonly diagnosed between ages 20 and 50, with a peak occurring at 30 years of age, but it can be seen at any age [3]. MS is the most common disabling neurological disease of young adults [4].
The disease affects up to 2 million people and the number of people with MS has increased. It is not clear if this increase is due to better diagnosis and reporting, or due to other causes [5]. Previously, Iran was considered as a low-risk region for MS, with a prevalence of < 5/100,000. Recent studies report an increase in the incidence and prevalence of MS in Iran, particularly in Isfahan province of Iran (with a prevalence of 73.3/100,000). This rapid change is mainly thought to be due to the change in lifestyle and vitamin D deficiency [6, 7].
MS involves an immune-mediated process in which an abnormal response of the body’s immune system is directed against the central nervous system and attacks myelin. The damaged myelin forms scar tissue (sclerosis), which gives the disease its name. This damage disrupts the ability of parts of the nervous system to communicate, resulting in a wide range of signs and symptoms, including weakness, fatigue, ataxia, bladder complaints, bowel problems, Motor symptoms, Cognitive changes, Paroxysmal symptoms(sensory or motor), sensory effects and visual impairment [8-10].
Pathologically, MS is characterized by demyelination, multifocal inflammation, reactive gliosis, oligodendrocyte and axonal loss [11, 12]. The clinical studies described four type of MS: relapsing-remitting MS (RRMS), primary-progressive MS (PPMS), secondary-progressive MS (SPMS), and progressive-relapsing MS (PRMS) [13]. Each of these disease courses might be mild, moderate or severe. The most common subtype is RRMS (more than 80% of cases) [14].
MS is a heterogenic and multifactorial disease, and a combination of genetic and environmental factors are involved [15]. In other words, MS triggered by environmental factors in genetically susceptible individuals [16]. Several potential risk factors for MS have been studied but the precise etiology of MS is not yet known [17]. Most important environmental risk factors are Epstein-Barr virus (EBV), smoking, and latitude/hypovitaminosis D. Other risk factors that are commonly studied include vaccinations, stress, and timing of birth, occupation, climate and diet [17-22].
Familial, twin and adoption studies support contribution of genetic factors to the disease [23, 24]. Among all candidate genes the major histocompatibility complex (MHC) region is unambiguously associated with MS [24]. Also, more than 50 non- MHC genetic risk factors has discovered which associated with MS [25]. However, a large proportion of MS heritability still remains unexplained [26]. The human leukocyte antigen (HLA) is the human version of MHC and the strongest susceptibility locus for MS [27]. The dense cluster of genes resides on chromosome 6 (6P21.3) and is responsible for regulation of the immune system in humans [28]. HLA genes have three groups: class I, class II, and class III. The present of antigens from outside of the cell to T-lymphocytes is the function of HLAs class II and it contains the classical alpha and beta chain genes including DP, DM, DOA, DOB, DQ, and DR. As Class II molecules can bind and present certain self-peptides, several studies indicated that HLAs class II have been associated to several autoimmune or immune mediated disorders, including MS [29]. An estimated 10-60% of the MS genetic risk appears to be conferred by the DR15 haplotype (DQB1*0602, DQA1*0102, DRB1*1501, DRB5*0101) [30]. Although several studies have been carried out on the association of HLA DRB5*01 with MS in various populations [31-34], there is no data about this issue in Khuzestan province in Iran.
We performed a case-control study to investigate the possible associations of HLA DRB5*01 locus in Iranian patients from Khuzestan province with MS. This included the investigation of any possible associations between HLA DRB5*01 locus and sex, initial symptoms, expanded disability status scale (EDSS) and course of disease.
2. Methods
The present case-control study focused on HLA DRB5*01 association in 202 MS patients from Khuzestan. Blood samples were obtained from 202 patients from Khuzestan province (that registered in the Khuzestan MS community). The McDonald criteria were used for MS diagnosis [35]. One hundred eighty seven healthy individuals as control were selected from the same geographic region and didn’t have any inflammatory or other autoimmune diseases. Healthy controls were matched on age and sex with MS patients. The study was approved by the ethics committee at Khuzestan MS community. Informed consent was obtained from all individuals.
Genomic DNA was extracted from peripheral blood leukocytes by the salting-out method. Nanodrop and electrophoresis methods were performed to determine the quality and quantity of the extracted genomes.
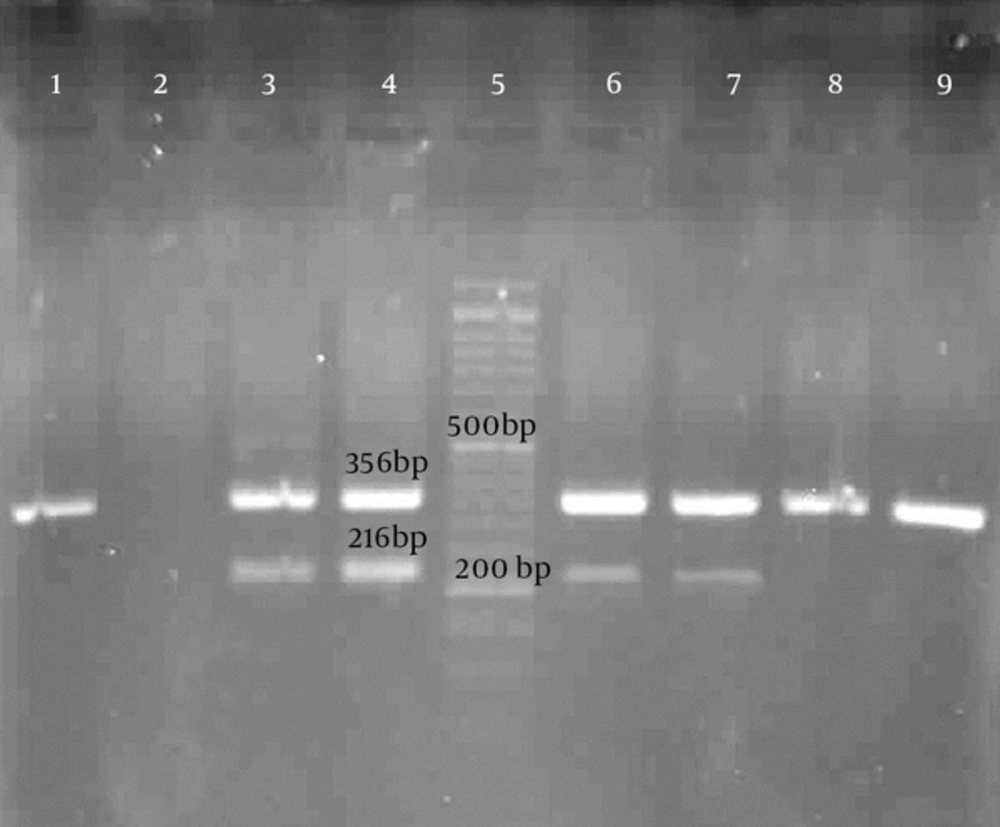
Typing of HLA-DRB5*01 on MS patients was investigated by polymerase chain reaction (PCR) amplification method on the extracted genome with sequence-specific primers (PCR-SSP). PCR amplification of the HLA-DRB5*01 was performed using two oligonucleotide primers (forward primer 5' TTCTTGCAGCAGGATAAGTAT 3'; and reverse primer 5' GTAGTTGTCCACCGCGGCG 3') [36]. The length of the products was 216 base pair. Myelin oligodendrocyte glycoprotein (MOG) gene was used as internal positive control. Primer sequences for amplification of the MOG were as follow: forward primer 5′-GGG ACC AAT TCT GTG TCA CC -3′; and reverse primer 5′-TGA ACC CAG AAG TCA CTC ACA -3′. In ideal PCR condition, 356 base pair bonds of MOG gene were visualized.
The PCR program was described as follows: 95°C for 4 minutes; 30 cycles of 95°C for 30 seconds, 62°C for 45 seconds, 72°C for 30 seconds; and then 72°C for 7 minutes. Finally, several samples were randomly sequenced to validate the results.
The frequency of the HLA-DRB5*01was calculated as percentage. SPSS 21 statistical software and chi square test were used to evaluate the significance of association between frequencies in the MS population compared with the control populations. Statistical significance was defined by a P value of less than 0.05.
3. Results
PCR amplification of the HLA-DRB5*01 and MOG were performed and visualized by gel electrophoresis (Figure 1).
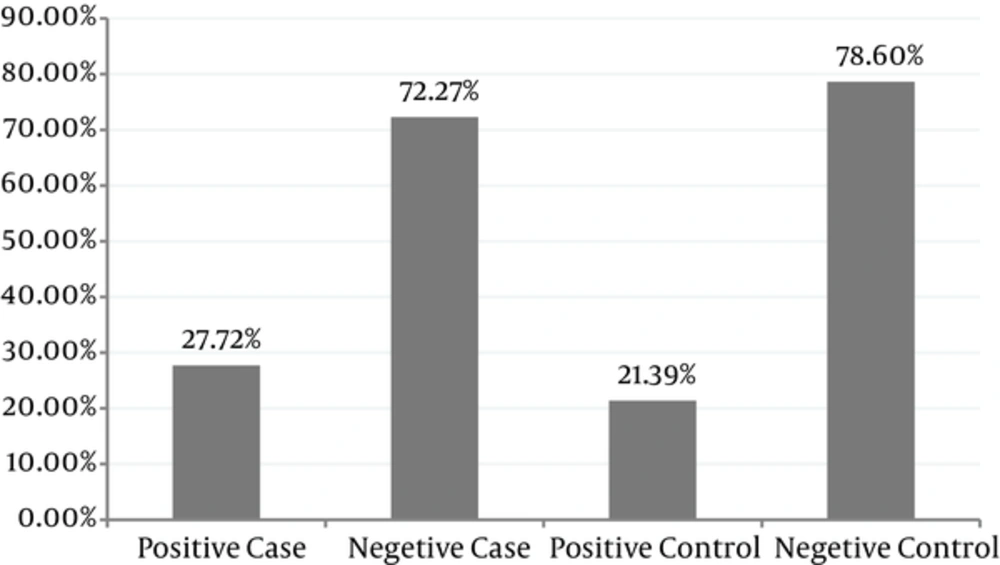
Two hundred and two MS patients were investigated in this study. Data was collected by a questionnaire. The frequency of HLA DRB5*01 in patients was 27.72% and in comparison with control groups (21.39%) no significant association was found with DRB5*01 and MS patients (P = 0.148) (Table 1 and Figure 2).
| Group | HLA DRB5*01 Positive | P Value | OR | CI |
|---|---|---|---|---|
| Case | 56 (27.72%) | 0.148 | 1.41 | 0.885 - 2.246 |
| Control | 40 (21.39%) |
The female to male ratio of 4:1 in MS patients was correlated with controls. The mean age of patients was 32.78 ± 8.37 (range of 16 - 56 years), and mean EDSS was 1.93 ±1.52 (range of 0 - 7.5). Most of the patients had EDSS less than 3. One hundred and fifty patients were characterized as RRMS, two as PPMS, five as SPMS, and two patients as PRMS. Table 2 shows the clinical features of the MS patients.
| Clinical Information | MS Patients | Controls |
|---|---|---|
| Total individuals with MS | 202 | 187 |
| Male | 42 (20.8) | 41 (21.9) |
| Female | 160 (79.2) | 146 (78.1) |
| Mean age of patients | 32.78 ± 8.37 | 56 ± 5.8 |
| Symptom | ||
| Visual disturbance | 82 (71.3) | |
| Sensory problems | 75 (64.1) | |
| Urinary symptoms | 41 (59.42) | |
| Bowel difficulties | 45 (64.28) | |
| Disease course | ||
| RRMS | 150 (74.25) | |
| PPMS | 2 (0.99) | |
| SPMS | 5 (2.47) | |
| PRMS | 2 (0.99) | |
| Mean EDSS | 1.93 ± 1.52 (range of 0 - 7.5) | |
| 0 | 26 | |
| 1 - 3 | 116 | |
| 3.5 - 5 | 18 | |
| 5 < | 8 |
aValues are expressed as mean ± SD or No. (%).
With respect to the presenting symptoms of the disease, higher frequencies were calculated for visual, sensory, bowel and bladder difficulties, respectively.
4. Discussion
Multiple sclerosis is a potentially disabling disease of the brain and spinal cord (central nervous system) and is the most common disabling neurological disease of young adults. Despite all the studies done in recent years, the precise etiology of MS is not yet known.
The earliest association between genes and MS was found in the human leucocyte antigen (HLA) region in 1972 [37, 38], but only in recent years this association has been clarified.
The closest association between the HLA-DR15 haplotype and MS was found in Caucasian MS patients [39]. The HLA-DR15 haplotype is comprised of two DR beta chain genes, HLA-DRB1*15:01 and HLA-DRB5*01:01. This region is in very strong linkage disequilibrium (LD). DR alpha chain and the two beta chains creates the two functional surface heterodimers, DR2b (DRA*0101, DRB1*1501) and DR2a (DRA*0101, DRB5*0101) [30]. Whether both or only one of the two alleles and resulting DR molecules contribute to MS etiopathogenesis are one of the most important questions in MS researches. Some studies show that DR2a is an etiologic risk factor of MS [39, 40]. Recent work in humanized mice indicates that functional epistatic interactions whereby DRB5*0101 directly modulates the severity of the ensuing disease through activation induced cell death (AICD) of encephalitogenic T cells which are restricted by DRB1*1501 [41].
In this study, we attempted to find out the possible association of HLA DRB5*01 locus in Iranian patients from Khuzestan province with MS. According to the results, the average age of patients was 32.78 ± 8.37 (range of 16 - 56 years). Habibi et al. in Mazandaran found that the mean age was 34.3 ± 4.9 [42]. In the study of divani and et al. the mean age of patients in Iran was 30.9 ± 8.9 [43].
In our study the female to male ratio was 4:1, which confirm that MS is more common in women than in men. In a review in 2013 from Iran, this ratio was reported from 1.8 to 3.8 in different studies [44]. This study has shown that 74.25% of MS patients affected with relapsing remitting type. In Kalanie et al. study (2003) RRMS frequency was 88% and Sahraian et al. (2013) in Qom found that more than 80% of patients had RRMS [45, 46].
In this study most of patients had EDSS 1-3 and the frequency of patients with EDSS > 5 were low. It was in line with other studies. As mentioned above mean EDSS was 1.93 ± 1.52 (range of 0 - 7.5) that was fewer than previous studies.
Our study shows that there is no significant association with HLA DRB5*01 among MS patients compared with control group (27.72% vs. 21.39%). Fogdell et al. in sweden showed the association of HLA class П haplotype includes the DRB5*0101 allele with MS [31]. Caillier et al. in 2008 found that there is a significant association between HLA DRB5 alleles and African American MS patients [32], also Donadi et al. in 2010 reported a positive association with DRB5 locus among Brazilian MS patients [33]. However, in a study performed in Japan, no association between DRB5*0101 and western type MS patients was found [34]. These differences may be due to variable ethnic backgrounds of various populations.
This is the first study that investigate HLA DRB5*01association with multiple sclerosis patients in Khuzestan. No significant correlation was observed between HLA DRB5*01 with sex, initial symptoms, type of MS disease and EDSS in Iranian patients from the province. We can conclude that HLA DRB5*01 cannot be considered as a genetic risk factor for MS in Khuzestan population. It is recommended to evaluate this allele in MS population in the other provinces of Iran for more documented results.