1. Background
Tuberculosis is an ancient infection disease made happened by the gram positive bacillus Mycobacterium tuberculosis. Tuberculosis causes a wide range of clinical infections. In general, this bacterium usually attack to lungs, however spine, kidney and brain are the other exposed organs. Tuberculosis infection must be treated correctly because they can lead to fatal [1-3]. Tuberculosis is still located among top ten causes of death in worldwide and known as an important global health problem. About 10.4 million people afflicted with tuberculosis disease which 5.9 million among men (56%), 3.5 million among women (34%) and 1.0 million (10%) among children. In 2015, 1.8 million people died because of tuberculosis that 300,000 death increased from the previous year [4-6]. Tuberculosis can spread from person to person through the air. M. tuberculosis would spread into the air by aerosol particles when a person with tuberculosis disease coughs, sneezes or speak. The bacterium is alive in the air for a long period, depends on the environmental circumstances. Breathing is the opportunity to contaminate non-immunized persons. Another form of tuberculosis from M. bovis can be transferred by using unpasteurized milk products [7]. The general symptoms of tuberculosis disease include feelings weakness, swollen lymph glands, night sweats, weight loss, fever, and lack of appetite. However, cough (for 3 weeks or longer) is the most common symptom. The patients often are complained from chest pain, and coughing with blood, sputum or mucus from the lungs. The signs of tuberculosis disease in other parts of the body such as kidneys, lymph nodes and bones are depend on the area affected, immune system of body and attack severity [8]. The pulmonary tuberculosis is observed more than other tuberculosis types [9]. Prevalence and incidence of tuberculosis is associated with many risk factors such as HIV infections, age, gender, asthma, smoking habits, and family history about contact with tuberculosis patients. The lateral criteria’s such as poverty, homelessness, war, immigration, malnutrition, diabetes, renal insufficiency, alcoholism and social disorders play important roles to increase the tuberculosis statistics [6] which they can reduce immune defense of body. Over the past two decades many challenges such as civil war have been occurred in south west of Asia which affects directly on people life conditions. The incidence and prevalence of tuberculosis have been increased because of poverty, immigration and unemployment. Also, the population of multidrug resistance of tuberculosis is growing as well as HIV cases which they are serious health risk which needs more attention for their control.
2. Objectives
Tuberculosis infection is a major health problem especially among developing countries. The prevalence of drug resistant mycobacterium with HIV cases are alarm for health community. This paper provides a short overview of sources of data to evaluate the epidemiology status of tuberculosis as a burden disease in Iran and neighboring countries.
3. Methods
This study as a descriptive- analytical research is conducted cross- sectional among Iran and neighboring countries since 1990. The information is obtained from exact and valid informative data from web of sciences, Scopus during 1990 - 2016. Some data were collected from related organization for control and prevention of tuberculosis such as WHO and CDC in different countries. The prevalence and incidence of tuberculosis and related factors were studied in each area and SPSS 22 and Excel 2013 are used for data analyzing. The possible causes for increasing or developing of tuberculosis are considered in each country.
4. Results
4.1. Tuberculosis in High Burden Countries
The world health organization (WHO) was reported 8.8 million incident cases of tuberculosis in 2010 that equivalent to 128 cases per 100,000 population globally. The five countries had the largest population of tuberculosis cases included India (2 - 2.5 million), China (0.9 - 1.2 million), South Africa (0.4 - 0.59 million), Indonesia (0.37 - 0.54 million) and Pakistan (0.33 - 0.48 million) [10]. These countries as well as Nigeria accounted 60% of new cases of tuberculosis in 2016 [4]. The rate of tuberculosis incidence was declined only 1.5% from 2014 to 2015 that revealed epidemic tuberculosis is more extensive than previously estimated and controlling is so difficult.
4.2. Tuberculosis in Iran
Based on the WHO report in 2015 the incidence rate of tuberculosis was 16 cases per 100000 populations in Iran [1, 11]. Tuberculosis affects about 16,000 Iranian people and killed about 2000 people each year [10]. The afghan immigrant had significant effect on tuberculosis transmission in Iran. The high incidence of tuberculosis among Afghan immigrants (63.5 per 100,000 in population) was reported from Fars province in 2009 [12]. The studies done by Moradi et al (2008) in Kerman province and Tabrizi et al (2014) in Hormozgan province show, the most new cases of tuberculosis were determined among immigrants that comes from Afghanistan, Pakistan, Bangladesh and India which are endemic area of tuberculosis [3, 5, 10].
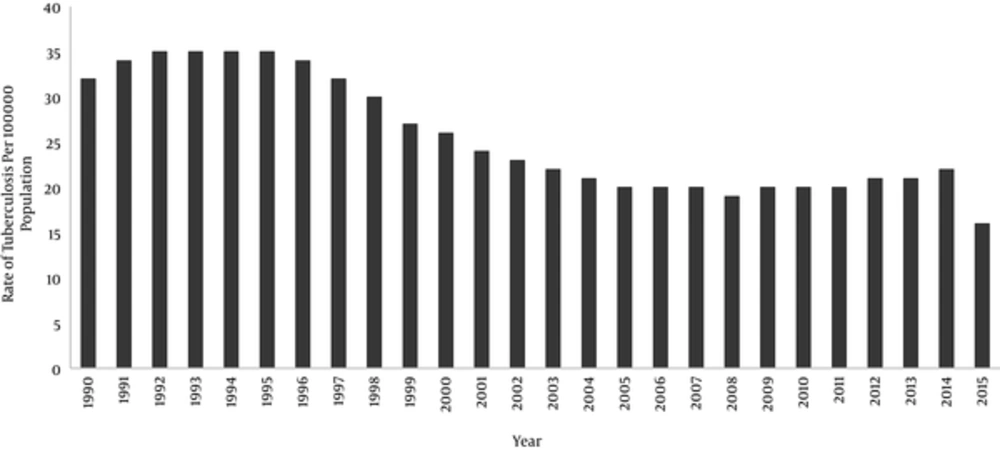
A brief history of tuberculosis in Iran show that the incidence of tuberculosis has been decreased from 142 per 100,000 population in 1965 to 16 per 100,000 population in 2015 [9, 13]. The rate of tuberculosis have reduced more than ten times during a half of century. The estimated incidence of tuberculosis per 100,000 population in Iran from 1990 to 2014 is shown in Figure 1. The highest rate of incidence was during 1992 - 1995 and then the incidence rate decreased gradually.
The highest and lowest rates of the tuberculosis incidence among Iranian provinces in 1997 were 73.5 and 32 per 100,000 populations in Sistan-Baluchistan and Semnan Provinces, respectively [10, 13]. From 9000 tuberculosis cases that were reported in 2001, Sistan-Baluchistan province especially in the Zabol city and Golestan province had the first and second positions. The incidence of tuberculosis was higher in old persons (> 50 years old) than young patients and the tuberculosis infection was occurred among woman higher than men [9, 10]. However, based on WHO’s report in 2013, the male to female ratio for tuberculosis was 1.1 in Iran [5].
During 2005, the prevalence of tuberculosis was 44 cases in Sistan-Baluchistan province, 38 cases in Golestan Province, and 25 cases per 100,000 population in Khorasan Province while the prevalence was low in the central parts of Iran such as Isfahan and Fars provinces [12, 14]. The incidence of tuberculosis was 10485 cases which 2.2% were HIV positive in 2010 [13].
4.3. Tuberculosis in Neighboring Countries of Iran
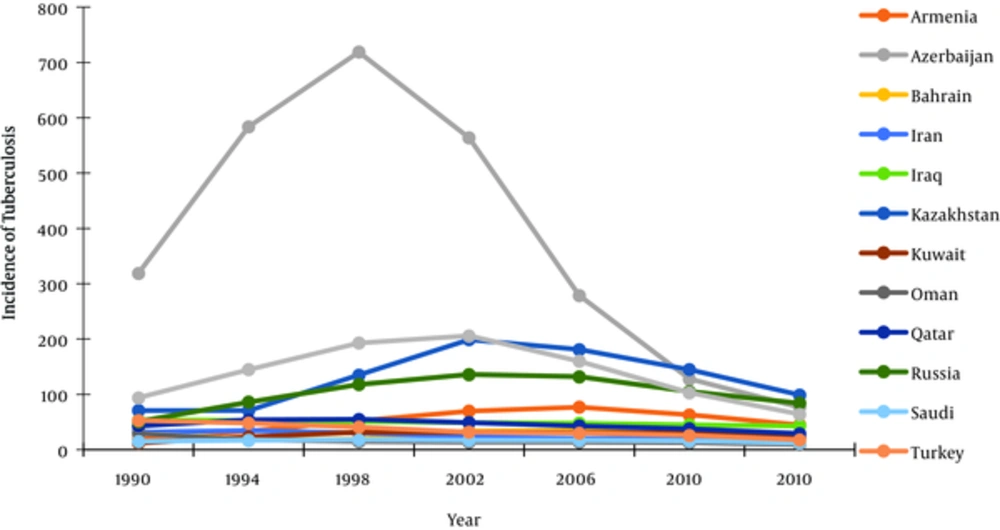
The distribution of tuberculosis in Iran is related with tuberculosis condition in Iran neighboring countries. The incidence of tuberculosis in Iran and neighboring countries during 24 years from 1990 to 2014 are shown in Figure 2 but the statics data from Afghanistan and Pakistan were not reported correctly and they don’t shown in Figure 2.
a) Azerbaijan
Azerbaijan is a north neighboring of Iran as a high tuberculosis priority countries with estimated 10,000 per 100,000 incident tuberculosis cases in each year. The incidence of tuberculosis in this country was significantly higher than other neighbor countries from 1992 - 2006 because of politic and economic problems which occurred since 1992. The incidence of tuberculosis in Azerbaijan was 77 in 2014 that decreased to 69 per 100,000 population in 2015 [4]. The highest rate of tuberculosis was determined between 15 - 34 years among men. The number of total registered tuberculosis cases was 14,274 people in 2000 that was reduced to 9,757 in 2014 [15]. The rate of tuberculosis infections reduced after 2011 because the governmental budgets for tuberculosis control and treatment had increased. This country is a member of high Multi drug resistant tuberculosis (MDR-TB) burden countries [15, 16].
b) Russia Federation
Russia is the biggest country in northern borders of Iran that the prevalence of tuberculosis is a major problem in some regions. The incidence of tuberculosis was 83 per 100,000 population in 2014 that declined slightly to 80 in 2015 [4]. The tuberculosis incidence was higher among men between 25 - 44 years. The prevalence of tuberculosis was higher in the eastern parts in borders of Russia about ten times more than Moscow. The control and treatment programs for tuberculosis have been recovered in recent years that resulted, the tuberculosis incidence statistics is decreased [17].
c) Kazakhstan
Kazakhstan located in the north of Iran, the rate of tuberculosis incidence in 1995 was 135 case per 100000 population that increased to 196 case in 2000 and the incidence rate grown to 233 per 100,000 population in 2004 and then reduced slightly to 139 in 2013 [1]. In the end of 2015, the incidence rate of tuberculosis has declined to 89 per 100,000 population (11.9%) because many programs executed to reduce the population of patient. In spite of many plans, growing of MDR-TB cases is a serious challenge to control tuberculosis distribution. About forty percent of tuberculosis cases and 14% of all newly diagnosed tuberculosis patients in Kazakhstan are MDR-TB. The population of MDR-TB was increased two times from 5.8 to 10.5 per 100,000 cases during three years (2007 to 2010) and now this country is listed among 20 top countries with MDR-TB cases. In addition, 45% of retreatment cases are identified as MDR-TB. Positive HIV cases is an important risk factor that related to increasing MDR-TB transmission rates [18].
d) Turkmenistan
Tuberculosis is also known as an important public health problem in Turkmenistan. The tuberculosis incidence has been increased 50% from 1991 to 1998 and then some programs started for tuberculosis control in new independent countries in north of Iran that resulted the incidence rate of tuberculosis decreased slightly (6%) from 84 to 79 cases per 100,000 from 1999 to 2001 [1, 19]. The rate of tuberculosis incidence was 64 cases per 100,000 people in 2014 but it increased to 70 cases in 2016 [4, 20]
e) Armenia
In the Republic of Armenia, tuberculosis is a serious public health that needs to more attention. The incidence of tuberculosis was 77 cases per 100,000 population in 2002 that show the highest number of patients in the age group 15 - 24 years. The official Armenian statistics reported a significant decline in the population of active cases of tuberculosis from 6,455 cases in 2005 to 3,707 cases in 2010. The incidence rate tuberculosis is decreased to 44 per 100,000 population in 2015 [1]. However, MDR-TB in Armenia is a big challenge for health organizations because the prevalence of MDR-TB are 12% and 57% in new and previously treated patients, respectively. The new strategies for re-emergence of tuberculosis infection after 1995 that supported from WHO is successful for control of tuberculosis in this country [21]. But the rate of MDR-TB cases show the control of tuberculosis is very difficult [22].
f) Afghanistan
The east neighboring of Iran, Pakistan and Afghanistan are important sources for tuberculosis distribution in area. For a long periods Afghanistan was listed among the high burden countries which suffer from high prevalence of tuberculosis but the tuberculosis controlling programs could be reduced the tuberculosis infection rate now. In each year, 53,000 tuberculosis cases reported which %66 are women and %10 are children. Almost 13,000 Afghans die because of tuberculosis annually [1]. The notified cases of tuberculosis was increased from 9668 in 2001 to 28,167 case in 2011 [23]. The high incidence of tuberculosis was 325 per 100,000 in 2001 that increased to 333 in 2006, and then decreased to 189 per 100,000 population during 2014 but still tuberculosis incidence is more than six times than tuberculosis incidence in Iran [1, 23]. Only in 2014, 58000 new tuberculosis patients were identified in Afghanistan, out of which 56% were diagnosed and provided a six-month treatment course others and as well as 25,000 patients were missed out by the health systems.
g) Pakistan
Pakistan is another member of 22 high-tuberculosis burden countries which have border line with Iran. The tuberculosis incidence rate was 270 case per 100,000 annually that more than 510,000 patients were reported in 2015 which the most of them were in range 15 - 34 years [1].
Pakistan currently ranks 5th among countries with highest burden of tuberculosis alongside the 4th highest burden of drug resistant tuberculosis and it has ranking 4th in terms of tuberculosis mortality rates (34 deaths per 100,000 population) [24]. Approximately 420,000 new cases of tuberculosis reported in Pakistan every year. In 2009, approximately 60,000 cases are died because of tuberculosis infection. The prevalence of tuberculosis was 350 cases per 100,000 population in 2010. The incidence was 231 per 100,000 population in 2012 that only 64% of new cases were determined and unknown number of patients were missed out. The incidence of tuberculosis in 2013 was 275 in 100,000 population [25, 26].
h) Iraq
Iraq is among seven tuberculosis contaminated in the eastern Mediterranean countries and occupied rank 108 globally with a high burden of tuberculosis because of long internal wars. There is an estimated 20,000 tuberculosis patients in Iraq and added 15,000 new cases that resulted 4000 deaths because of tuberculosis infection in each year [2]. In 2011 and 2014, the incidence of tuberculosis were 45 and 43 per 100,000 population, respectively which included about 8268 new and relapse cases in each year. A large percentage of tuberculosis cases (about 40%) were not diagnosed and treated for tuberculosis. In Iraq the incidence of drug resistance tuberculosis is very low rate (1.1%) compare with Iran north neighboring countries [2, 27].
4.4. Effective factors for tuberculosis infection
Prevent and treatment of tuberculosis are known earlier but still it is a major problem for health societies. Tuberculosis is depending on many socio-economic factors. Some factors such as civil war, poverty and malnourishment are effective on tuberculosis infection. Immigration is an undeniable topic that contributing to tuberculosis distribution. In United States in 2014 about 13000 new cases of active disease have been reported which over half cases determined in person was born outside of the country [1].
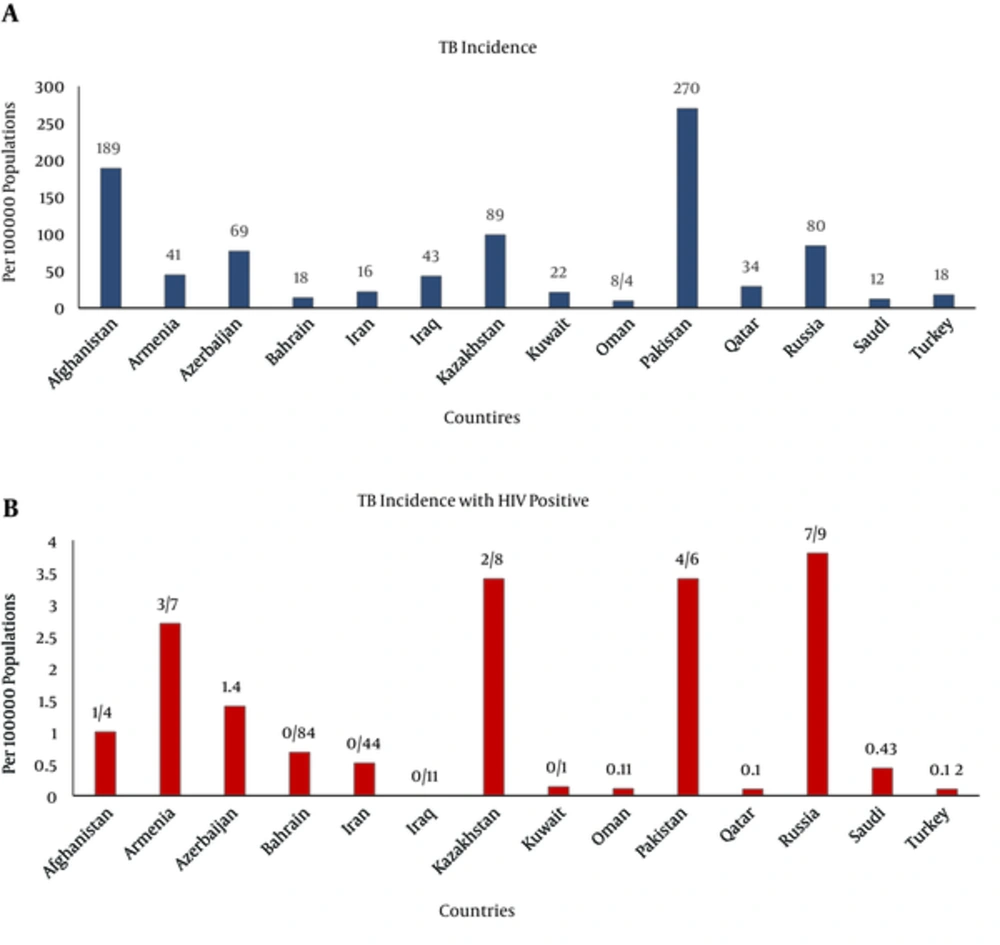
The Human Immunodeficiency Virus (HIV) is another cause to increase tuberculosis chance in Africa and some part of Asia [3]. Tuberculosis and HIV are associated closely because the people infected with HIV are very sensitive for infections by M. tuberculosis [5]. In 2008, from 1.8 million people died because of tuberculosis, half of them associated with HIV. The rate of TB/HIV co-infection has been reported 2.4% in 2012 [28]. In 2014 from 9.6 million people suffering from tuberculosis disease, 1.2 million (12%) were HIV-positive which the African region had accounted two-thirds parts of cases [1, 9, 29]. HIV-associated tuberculosis deaths accounted for 25% of all tuberculosis deaths in 2014. Only in 2015, more than 400,000 new cases with tuberculosis and HIV were added [4]. The risk of tuberculosis progression with HIV positive cases was 30% but this rate was 5% - 10% in HIV-negative cases [6, 9]. The prevalence of HIV for tuberculosis patients was 2.2% that half of the HIV-positive cases were die [1, 6]. The prevalence of HIV/AIDS in Iran has been increased during recent years (8%) and the estimated number of infected people with HIV was 13000 cases that reported in 2015 [1]. The incidence of tuberculosis is shown in Figure 3A and the incidence of tuberculosis associated with HIV is identified in Iran and its neighboring countries in Figure 3B. The data analysis confirmed that the patient population with tuberculosis and HIV are significantly low (< 1%) in some countries such as Afghanistan than Russia Federation [22].
Delay in diagnosis or treatment of tuberculosis is caused to further transmission and higher costs for treatment [30]. In 2006, the delay time between symptom appearances to treatment was 127 days in Iran which declined to 56 days recently [6, 14]. Nine million people are contracted with tuberculosis annually that three million of them are not diagnosed for quality-assured tuberculosis treatment that two of three million from untreated population die each year [14, 31]. In some case delay in diagnosis is because of latent form of tuberculosis [32]. If the therapy for tuberculosis is not adequate resulted to drug-resistant strain of M. tuberculosis.
Drug-resistant tuberculosis is another concern caused irregular or inadequate therapy [1, 32]. The resistance to at least two most potent first-line drugs for tuberculosis treatment (including Isoniazid and Rifampin) known as multidrug-resistant tuberculosis (MDR-TB). Since 1990, the outbreaks of multidrug-resistant strains of tuberculosis were reported with HIV co-infection. In more than 100 countries, 5% of all tuberculosis cases were reported MDR-TB in 2009. The MDR-TB cases were determined in 3.3% of new cases and 20% of previously cases that treated for tuberculosis though the data was variable in each region. In 2014, 12% of new cases and 58% of treated patient were MDR-TB cases that caused 190,000 deaths. From 580,000 new cases of MDR-TB, three countries including India, China and Russia Federation accounted for 45% of cases in 2015. The cost needed for each patient be treated for MDR-TB is typically 10 timers more than drug susceptible tuberculosis patient [1]. Of the 26 countries with high MDR-TB, eight countries are neighbors by Iran such as Kazakhstan, Azerbaijan, Russia Federation and Pakistan [4]. Extensively drug resistant tuberculosis (XDR-TB) is a rare but catastrophic condition than MDR-TB that recently identified as a serious issue for treatment of tuberculosis cases. XDR-TB cases are resistant to many drugs such as Isoniazid and Rifampin as well as, second line of antibiotics such as Fluorquinolone. The new finding including about 9.7% of MDR-TB cases are XDR-TB which the population increased rapidly [14]. Masjedi and associated (2010) reported 6.7% of MDR-TB cases were XDR-TB in Iran [31]. Based on WHO report 0.32 per 100,000 of cases were MDR-TB during 2015 [4] which was low but needs to more attention for tuberculosis patients.
5. Discussion
Iran is located in a middle area of tuberculosis distribution map in Eastern Mediterranean. Two countries with a high prevalence of tuberculosis (Pakistan and Afghanistan) have long borders in the east of Iran and Iraq in the west of Iran which their health community organizations have been severely destroyed because of civil and internal wars. In north neighboring countries of Iran such as Russia Federation, MDR-TB is known as a serious problem. The extended borders among Iran with high-tuberculosis burden countries (Afghanistan and Pakistan) and the immigration from these countries changed the tuberculosis rate and distribution in Iran [3, 11]. The high prevalence of tuberculosis in some area of Iran including Sistan-Baluchistan and Khorasan provinces were predictable because they located near Afghanistan and Pakistan [12]. In Iran BCG vaccination program correctly down that results included the tuberculosis incidence was low for age < 14 years. However, the MDR-TB cases must be control especially in border Provinces of Iran.
In north of Iran, Azerbaijan is a challenge for tuberculosis transmission in the area. After the former Soviet Union (FSU) collapse in 1992, access to anti-tuberculosis chemotherapy became destroyed, lead to the many failure in diagnosis and tuberculosis treatments. Consequently, the insufficient attention caused for spreading of tuberculosis and then increased MDR-TB cases among infected population in new countries such as Russia [17]. Human migration can transmit tuberculosis to recipient countries such as Iran. The result of study by Asgharzadeh and associated (2015) shown the prevalence of tuberculosis in the north west of Iran was affected with the prevalence of tuberculosis in Republic of Azerbaijan. Transmission of tuberculosis to Iranian from Republic of Azerbaijan people is considerable. Besides the treatment of tuberculosis is free in Iran so some patients come from Azerbaijan to Iran for treatment subsequently the chance of tuberculosis transmission will be increased. The similar culture between two areas increased the people exposure [5, 16]. In view of that, the management of patients travel from Azerbaijan to Iran should be considered. In Russia Federation, economic problems, poverty, unemployment and increase in crime rate made the population poorer so the prevalence of tuberculosis increased. Migration into the country also contributed to the tuberculosis spread. In some countries such as Russia and Armenia multidrug resistance is a serious concerns which must be controlled. The Afghans population has encounter with a lot of problems. Many of them are at risk for contracting tuberculosis include women and children, poor and elderly, or malnourished people. In Afghanistan, women significantly are at risk of tuberculosis that two-thirds of tuberculosis cases determined in woman [1]. The high burden of tuberculosis in this country be influenced by living conditions, poverty, traditional beliefs, lack of awareness about tuberculosis, war, lack of access to proper medications and health facilities for diagnosis of the disease. In Pakistan also, non-governmental organizations, lack of public awareness coupled with limited engagement of communities have been identified as challenges impeding tuberculosis control [24]. Both countries, Afghanistan and Pakistan have great population that infected with tuberculosis but the facility and budget is not enough for their prevention or treatment. Many of public health organization try to increase the tuberculosis knowledge and prepare the capacity for further education as well as tuberculosis vaccination. In Iraq the tuberculosis infection has been increased because of internal war and their problems.
In Iran many programs were down for a few years but any challenge in Iran neighbor’s had directly affected to tuberculosis incidence in Iran. Traveling especially to religious cities, grouping and illegal immigration could be increased the rate of tuberculosis in Iran. In this paper some neighboring countries were shown high tuberculosis infection in contrast some neighboring countries such as Turkey or Saudi Arabia have similar or lower tuberculosis incidence then Iran.
5.1. Conclusions
During recent years many efforts in Iran and neighboring countries were carried to control the tuberculosis infection. However, it should be considered that short and long programs with powerful supports for limitation or eradication of tuberculosis are needed. According to the objective of policy making by the Ministry of health in Iran, by the year 2025, the detection rate of pulmonary tuberculosis is increasing to more than 85% and the rate of treatment increased to more than 90%. During recent years some countries such as Afghanistan and Armenia were successful in tuberculosis controlling programs. Improving case detection and treatment adherence, reducing stigma, discrimination and increasing the people knowledge about tuberculosis, decreased the various risk factors of tuberculosis, immunization and prophylaxis for tuberculosis and empowering tuberculosis patients are important steps for reducing of tuberculosis cases. According to the objectives of Health Millennium goals (MDGs), it is expected that the global active tuberculosis incidence in 2050 would be less than one case per million population per year. This aim obtained with accurate epidemiological information of tuberculosis. Plan and prevention control strategies such as vaccination and prophylaxis for tuberculosis should be improved to reduce the treatment costs. The HIV positive cases with tuberculosis or MDR-TB are serious health problems that their treatment are so difficult and more expensive than other tuberculosis cases therefore, the development of better and more rapid prevention and diagnostic methods and continuous monitoring of them are urgent priorities for the control of tuberculosis cases.