1. Background
Multiple Sclerosis (MS) is one of the most common neurological diseases, which is a chronic progressive degenerative disease (1) resulting in psychological changes that can affect the lives of patients. At present, many researchers believe that the importance of diagnosis and treatment of complications such as depression, anxiety, and stress in patients with MS should not be neglected. In fact, these symptoms can lead to a significant reduction in the quality of life. Depression, anxiety, and stress can limit the patients’ participation in their workplace, reduce their general health, make them susceptible to relapses, aggravate symptoms such as fatigue, and increase dissatisfaction with their family and social lives. Furthermore, some psychological symptoms (such as depression) have been identified as the most important risk factors for suicide (2); major depressive disorder (MDD) has been reported in 38% of people who have attempted suicide, whereas 75% have been diagnosed with a depression syndrome (such as MDD or depressive disorder not otherwise specified (NOS)) (3).
In recent years, clinical studies on MS have increased. In this regard, a part of MS-related research has corroborated the relationship of depression, anxiety, and stress with fatigue (4-11) and reduced quality of life (5, 12-17); while some others have emphasized the predictive role of these symptoms in MS (5, 7, 9, 13-16). However, these studies have often focused on depression and anxiety (6, 7, 12, 17) and have shown the role of stress only in relation to inflammation (18), relapses (19, 20), disease activity (21), and brain lesions (22). Besides, research on quality of life focused on only two overall components of mental and physical health (5, 14, 15, 17, 23, 24), and limited studies have separately examined the predictive role of psychological symptoms in each aspect of health (25). In the meantime, the lack of control of confounding factors or small sample size is another problem that has affected the quality of the results (26). In addition, previous research which has used various tools and subsequently conducted studies on depression, anxiety, and stress in MS have not revealed consistent findings. In this regard, some studies have shown the role of these symptoms on clinical and health components (6, 15) and in others, they have not emerged as significant predictors (5, 27). Therefore, increasing awareness about the predictive validity of valid self-report instruments for measuring depression, anxiety, and stress in MS and can enhance the conviction of clinicians to use multi-symptom psychological tools and therapeutic interventions, particularly in MS clinical practices (28-31).
2. Objectives
Since evaluation and understanding of depression, anxiety and stress could have an increasingly important role in the diagnosis, treatment, and care management of psychological symptoms in MS patients, the present study aims to assess the concurrent and predictive validity of the Depression Anxiety Stress Scale-21 (DASS-21) in patients with MS.
3. Methods
3.1. Population and Sample
The present research was a cross-sectional study. The study population included all the members of the MS Society of Guilan Province (the north of Iran) in 2010, from which 162 sample patients with pathologic criteria for MS were selected using the consecutive sampling method. Inclusion criteria were patients diagnosed with MS disease based on the McDonald Criteria (32), with the diagnosis confirmed by a neurologist (the diagnosis of MS was confirmed from the clinical symptoms and characteristics of the patients and evidence of lesions in two or more locations in the central nervous system), and having a registered file in the MS Society and receiving the definitive diagnosis of this disease. The exclusion criteria were: (a) occurrence of an acute MS attack, (b) presence of severe cognitive problems in a way that the patient was unable to fill out the questionnaires and research tools, and (c) existence of any debilitating disease or physical complication associated with MS. Subsequently, after ensuring that all the instruments were evaluated and the forms were completed, it was confirmed that none of the patients would be excluded from the study.
3.2. Instruments
3.2.1. Depression Anxiety Stress Scales-21 (DASS-21)
The Persian version of this instrument that was originally developed by Lovibond and Lovibond (33) has been used to assess depression, anxiety, and stress in MS patients. The DASS-21 questionnaire consists of three seven-item subscales for the assessment of depression, anxiety, and stress. In this study, MS patients were asked to carefully read each statement in DASS-21 and then rate their health status during the last week on each scale. In DASS-21, the classification of responses for each scale is in a range between 0 and 3, and higher scores indicate more severe symptoms of depression, anxiety, and stress (34). The test-retest reliability of the Persian version of DASS over four weeks was r = 0.72. Internal consistency reliability was assessed using Cronbach’s alpha coefficient. For the total scale, alpha was 0.91 (depression, α = 0.92; anxiety, α = 0.88, and stress, α = 0.82). In sum, evidence confirms the preliminary reliability and preliminary construct validity of the Persian translation of DASS (35).
3.2.2. Fatigue Severity Scale (FSS)
The Persian version of this tool has been used to measure fatigue severity (36). This tool was initially created by Krupp to measure the fatigue level of MS patients. It is a 9-item scale that examines the amount of fatigue with scores ranging from 1 to 7. A score of 1 indicates that the person strongly opposes, and a score of 7 indicates that a person fully agrees. The total score will be between 1 and 7 points and 7 shows the highest fatigue. The criterion validity of this tool has been reported as 0.68 and the internal consistency coefficient as 0.81 (37). The psychometric properties of FSS have been evaluated in Iran and indicate a very high Cronbach’s alpha score (α = 0.93). The coefficient of item-total correlation for each item was in an acceptable range of 0.43 to 0.85. The results of concurrent validity showed that FSS has a good correlation with the constructs of depression, anxiety, and physical dimensions of quality of life (P < 0.001) (36).
3.2.3. Short Form Health Survey (SF-36) Questionnaire
Developed by Ware and Sherburne, SF-36 measures physical and mental health with respect to 36 items and 8 subscales, including physical functioning (PF), role limitations due to physical health (RP), bodily pain (BP), general health (GH), vitality (VT), social functioning (SF), role limitations due to emotional problems (RE), and mental health (MH) (38). The score of each criterion will be between 1 and 100, and higher scores indicate better quality of life. Psychometric properties of SF-36 were recently evaluated on a group of MS patients, and the results showed that the internal consistency of SF-36 subscales, except social functioning and emotional problems (α = 0.42 to 0.93), was favorable. The SF-36 items had a positive correlation with subscales on their own (r = 0.48 to 0.95). Each subscale had an inverse correlation with clinical and psychological constructs (r = -0.27 to -0.71; P < 0.001) (39).
3.2.4. Data Analysis
In order to describe the data in this study, central tendency measures were used. In the inferential statistics section, we applied Pearson’s correlation analysis to test the concurrent validity. Also, multivariate hierarchical regression analyses were used to evaluate the predictive validity of DASS-21, after adjusting the possible impact of confounding factors such as age, gender, marital status, and education (all P values less than 0.05). All statistical analyses were performed using IBM SPSS Statistics 24.0 software.
4. Results
In this study, 162 MS patients were selected as the sample and were analyzed in terms of demographic variables. Accordingly, the mean age of patients was 34.01 ± 9.45 (in a range from 16 to 58), and their average level of education was 11.72 ± 3.49 (in a range from 0 to 19). Table 1 shows the results obtained from studying the demographic and clinical variables of MS patients (n = 162).
| Variable | No. (%) |
|---|---|
| Gender | |
| Male | 48 (29.6) |
| Female | 114 (70.4) |
| Marital status | |
| Single | 39 (24.1) |
| Married | 123 (75.9) |
| Relapse background | |
| Lack of relapse | 18 (11.1) |
| Once | 30 (18.5) |
| Twice | 27 (16.7) |
| Three times | 25 (15.4) |
| More than 3 times | 62 (38.3) |
| Hospitalization background | |
| Lack of hospitalization | 62 (38.3) |
| Once | 59 (36.4) |
| Twice | 19 (11.7) |
| Three times | 9 (5.6) |
| More than 3 times | 13 (8) |
| MS type | |
| Relapsing-Remitting (RR) | 118 (72.8) |
| Primary-Progressive (PP) | 4 (2.5) |
| Secondary Progressive (SP) | 34 (21) |
| unknown | 6 (3.7) |
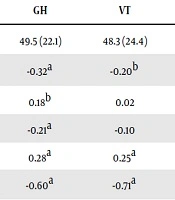
In order to assess the concurrent validity of DASS-21 subscales, Pearson’s correlation method was applied (Table 2). According to the data shown in this table, all symptoms of depression, anxiety, and stress have a significant positive relationship with fatigue and significant negative relationship with SF-36 components (r = 0.29 to -0.71; P < 0.01). Among the demographic variables, age (except for role limitations due to emotional problems) and education level (interval scale) have a significant relationship with all variables. The point-biserial correlation coefficients for two variables of gender (men = 0 and women = 1) and marital status (single = 0 and married = 1) also showed that gender has a significant relationship with physical functioning, role limitations due to physical health, and general health. Furthermore, marital status has a significant relationship with fatigue, physical functioning, and general health.
| Variable | Fatigue | PF | RP | BP | GH | VT | SF | RE | MH | D | A | S |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| M (SD) | 4.9 (1.7) | 55 (33) | 44.4 (39.5) | 62.1 (32.1) | 49.5 (22.1) | 48.3 (24.4) | 61.6 (27.3) | 49.8 (40.2) | 55 (22.4) | 8.2 (6.3) | 7.4 (5.4) | 11.4 (5.8) |
| Age | 0.27a | -0.40a | -0.28a | -0.16b | -0.32a | -0.20b | -0.18b | -0.13 | -0.13 | 0.24a | 0.12 | 0.14 |
| Gender | -0.04 | 0.21a | 0.22a | 0.03 | 0.18b | 0.02 | 0.10 | 0.12 | 0.09 | -0.06 | -0.05 | -0.07 |
| Marital status | 0.23a | -0.28a | -0.15 | -0.14 | -0.21a | -0.10 | -0.08 | -0.09 | -0.06 | 0.11 | 0.11 | 0.09 |
| Education | -0.23a | 0.29a | 0.32a | 0.23a | 0.28a | 0.25a | 0.26a | 0.27a | 0.24a | -0.41a | -0.40a | -0.40a |
| Depression | 0.37a | -0.46a | -0.47a | -0.39a | -0.60a | -0.71a | -0.48a | -0.53a | -0.68a | 1 | 0.71a | 0.82a |
| Anxiety | 0.31a | -0.45a | -0.57a | -0.48a | -0.53a | -0.59a | -0.44a | -0.56a | -0.57a | 0.71a | 1 | 0.77a |
| Stress | 0.29a | -0.34a | -0.48a | -0.43a | -0.48a | -0.63a | -0.45a | -0.58a | -0.67a | 0.82a | 0.77a | 1 |
aP < 0.01
bP < 0.05
Table 3 presents a set of multivariate hierarchical regression analyses with the aim of assessing the predictive validity of DASS-21 and how much symptoms of depression, anxiety, and stress (as predicting variables) can explain the changes in criterion variables such as fatigue and SF-36 components. These regression analyses were performed after controlling the confounding factors. For this purpose, Pearson’s correlation coefficients and point-biserial correlation coefficients between criterion variables and some possible confounding variables such as age, gender, education level, and marital status were calculated (refer to Table 2), and then for those variables that had a significant relationship with criterion variables (P < 0.05), their effects on the relationships between three symptoms of depression, anxiety, and stress as well as criterion variables was controlled. Hence, in the regression analyses, the possible confounding factors (P < 0.05) were applied to the regression equation before entering the predicting variables of depression, anxiety, and stress so that any confounding effect was removed. In the next step, the subscales of depression, anxiety, and stress were applied to the regression equation in the predictive block (Table 3).
| Criterion Variables | Model Summary | Control & [Predictive] Variables | β | P-Value | ∆R2 |
|---|---|---|---|---|---|
| Fatigue | Step 1: Age | 0.22 | 0.018a | 0.08 | |
| Marital status | 0.003 | 0.976 | |||
| Education | -0.17 | 0.029a | |||
| R2 = 0.18 (F4,157 = 8.40, P < 0.0001) | Step 2: [Depression] | 0.31 | 0.000a | 0.15 | |
| R2 = 0.15 (F4,157 = 7.16, P < 0.0001) | [Anxiety] | 0.26 | 0.002a | 0.13 | |
| R2 = 0.14 (F4,157 = 6.41, P < 0.0001) | [Stress] | 0.22 | 0.006a | 0.12 | |
| PF | Step 1: Age | -0.31 | 0.001a | 0.19 | |
| Gender | 0.12 | 0.097 | |||
| Marital status | -0.01 | 0.862 | |||
| Education | 0.20 | 0.007a | |||
| R2 = 0.31 (F5,156 = 14.37, P < 0.0001) | Step 2: [Depression] | -0.36 | 0.000a | 0.29 | |
| R2 = 0.33 (F5,156 = 15.72, P < 0.0001) | [Anxiety] | -0.39 | 0.000a | 0.31 | |
| R2 = 0.26 (F5,156 = 11.08, P < 0.0001) | [Stress] | -0.25 | 0.001a | 0.24 | |
| RP | Step 1: Age | -0.18 | 0.019a | 0.15 | |
| Gender | 0.16 | 0.028a | |||
| Education | 0.26 | 0.001a | |||
| R2 = 0.29 (F4,157 = 15.99, P < 0.0001) | Step 2: [Depression] | -0.38 | 0.000a | 0.27 | |
| R2 = 0.40 (F4,157 = 26.34, P < 0.0001) | [Anxiety] | -0.53 | 0.000a | 0.39 | |
| R2 = 0.30 (F4,157 = 17.17, P < 0.0001) | [Stress] | -0.40 | 0.000a | 0.29 | |
| BP | Step 1: Age | -0.10 | 0.194 | 0.05 | |
| Education | 0.21 | 0.010a | |||
| R2 = 0.16 (F3,158 = 10.39, P < 0.0001) | Step 2: [Depression] | -0.35 | 0.000a | 0.15 | |
| R2 = 0.24 (F3,158 = 16.45, P < 0.0001) | [Anxiety] | -0.45 | 0.000a | 0.22 | |
| R2 = 0.19 (F3,158 = 12.77, P < 0.0001) | [Stress] | -0.40 | 0.000a | 0.18 | |
| GH | Step 1: Age | -0.36 | 0.000a | 0.17 | |
| Gender | 0.10 | 0.178 | |||
| Marital status | 0.21 | 0.016a | |||
| Education | 0.22 | 0.004a | |||
| R2 = 0.43 (F5,156 = 23.61, P < 0.0001) | Step 2: [Depression] | -0.54 | 0.000a | 0.41 | |
| R2 = 0.40 (F5,156 = 20.69, P < 0.0001) | [Anxiety] | -0.50 | 0.000a | 0.38 | |
| R2 = 0.34 (F5,156 = 15.86, P < 0.0001) | [Stress] | -0.42 | 0.000a | 0.32 | |
| VT | Step 1: Age | -0.15 | 0.066 | 0.07 | |
| Education | 0.21 | 0.009a | |||
| R2 = 0.51 (F3,158 = 54.12, P < 0.0001) | Step 2: [Depression] | -0.72 | 0.000a | 0.50 | |
| R2 = 0.36 (F3,155 = 29.78, P < 0.0001) | [Anxiety] | -0.58 | 0.000a | 0.35 | |
| R2 = 0.41 (F3,158 = 37.01, P < 0.0001) | [Stress] | -0.63 | 0.000a | 0.40 | |
| SF | Step 1: Age | -0.12 | 0.121 | 0.07 | |
| Education | 0.23 | 0.004a | |||
| R2 = 0.24 (F3,158 = 16.71, P < 0.0001) | Step 2: [Depression] | -0.44 | 0.000a | 0.23 | |
| R2 = 0.21 (F3,158 = 14.45, P < 0.0001) | [Anxiety] | -0.40 | 0.000a | 0.20 | |
| R2 = 0.22 (F3,158 = 15.14, P < 0.0001) | [Stress] | -0.41 | 0.000a | 0.21 | |
| RE | Step 1: Education | 0.27 | 0.000a | 0.07 | |
| R2 = 0.29 (F2,159 = 31.96, P < 0.0001) | Step 2: [Depression] | -0.50 | 0.000a | 0.28 | |
| R2 = 0.32 (F2,159 = 36.96, P < 0.0001) | [Anxiety] | -0.54 | 0.000a | 0.31 | |
| R2 = 0.34 (F2,159 = 40.41, P < 0.0001) | [Stress] | -0.56 | 0.000a | 0.33 | |
| MH | Step 1: Education | 0.24 | 0.002a | 0.05 | |
| R2 = 0.47 (F2,159 = 70.76, P < 0.0001) | Step 2: [Depression] | -0.70 | 0.000a | 0.46 | |
| R2 = 0.32 (F2,159 = 37.71, P < 0.0001) | [Anxiety] | -0.56 | 0.000a | 0.31 | |
| R2 = 0.44 (F2,159 = 63.49, P < 0.0001) | [Stress] | -0.68 | 0.000a | 0.44 |
aP < 0.05
Regression analysis in the first step revealed that among the demographic variables, the variable of age significantly explains the variance of fatigue, physical functioning, role limitations due to physical health, and general health. Gender could explain only the variance of “role limitations due to physical health”. Similarly, marital status explains only the variance of general health. Finally, the education level could explain the variance of all criterion variables. After removing the confounding effect of control variables, regression analyses in the second step showed that symptoms of depression, anxiety, and stress significantly predict the variance of all criterion variables (in the range of 12% to 50%).
5. Discussion
In the present study, the concurrent validity of DASS-21 was assessed through the desirable and acceptable correlations of its subscales with other constructs that are expected to have significant positive or negative relationships with these subscales. The findings showed that all the three subscales of DASS-21 in MS patients have a significant positive relationship with fatigue and a significant negative relationship with the eight dimensions of health (in SF-36). Consistent with this finding, previous studies have reported that MS patients with higher scores on symptoms of depression, anxiety, and stress experience higher intensities of fatigue and lower levels of health components (4, 5, 17). A possible explanation is that depression, anxiety, and stress can have a negative impact on self-efficacy, self-worthiness perception, and the coping resources of the patients, which can lead to a reduction in health-related quality of life. The etiology of fatigue is not clear and is a multifactorial phenomenon as well. Thus, it is likely that effective biological changes in depression, anxiety, and stress can lead to exacerbation of fatigue.
The assessment of the predictive validity of DASS-21 showed that scores of depression, anxiety, and stress can explain a significant ratio of the variance of fatigue. In this regard, Greeke et al. (40) found that depression and fatigue have a significant relationship, and the change over time in depression leads to fatigue exacerbation. In a study on 122 MS patients, Labuz-Roszak et al. (6) identified depression and anxiety as significant predictor variables for fatigue. Recently, Brenner et al. (41) reported a significant correlation between depression and fatigue, while there was no relationship between stressful life events and fatigue. Additionally, another study using path analysis showed that depression has a direct effect on fatigue in MS patients and can predict it (42). A basic explanation for these results is the role of biological processes (41). It seems that psychological symptoms may be related to fatigue in terms of etiology and through inflammatory processes (i.e., cytokines, leading to the appearance of sickness behavior). Cytokines are central to the pathogenesis of MS (43). For example, Martins et al. (44) indicated that MS patients have elevated serum levels of both pro- and anti-inflammatory cytokines. In the meantime, one of the cytokines reported in MS is interleukin-6 (IL-6) (41). Levels of IL-6 increase sensitivity to stress (45) and are associated with fatigue (41). Theoretically, it can mediate stress activation and fatigue exacerbation. There is also a possible connection between stressful life events and MS exacerbations (46) that can lead to exacerbation of fatigue.
Moreover, despite the distinction between depression and fatigue, there is a great deal of overlap between their symptoms. For example, depression can predict later fatigue, and fatigue can predict later depression (7). Therefore, more detailed and comprehensive studies are needed to examine the underlying biological mechanisms of psychological symptoms and fatigue. Some conflicting results may be due to the use of different methods and questionnaires to diagnose both fatigue and psychological symptoms as well as reporting bias.
Our analyses also showed that DASS-21 after controlling the confounding factors has been able to predict all aspects of SF-36. Although similar studies that examine each aspect of health-related quality of life separately are limited, this finding is consistent with some previous results. In a recent study, Fernandez-Munoz and colleagues (42) demonstrated that depression with two components of SF-36, including bodily pain and mental health, were significantly associated with MS patients, while there was no relationship between depression and physical function. Kargarfard et al. (25) found that depression in MS patients could predict health components, including role limitations due to emotional problems, pain, emotional wellbeing, health perception, cognitive function, and health distress. Although depression could not predict the components of physical health, role limitations due to physical health, energy, social function, and sexual function. However, in their study, the multiple sclerosis quality of life questionnaire was used to measure health, which has more and different subscales from SF-36. Nourbakhsh et al. (24), in a longitudinal study, revealed that changes in depression were associated with changes in the components of physical health in SF-36. Barzegar et al. (23) in a comparative study on two groups of MS patients and neuromyelitis optica spectrum disorder, reported that depression and anxiety were independent and significant predictors of mental health dimensions. In addition, Enns et al. (47) showed that depression and anxiety can predict general functional impairment in a group of patients with inflammatory bowel disease, MS and rheumatoid arthritis even after accounting for the effects of demographic, clinical and psychological variables. It seems that depression, anxiety, and stress can decrease mental and physical health by energy depletion, decline in activity, reduction of participation in social practices, impairment in daily functioning, and weakness in positive thinking in MS patients. This indicates that the development and expansion of therapeutic interventions for MS patients aimed at reducing the symptoms of depression, anxiety, and stress can lead to the reduction/prevention of clinical fatigue symptoms and improved health components in these patients. This hypothesis is supported by a review reporting that appropriate intervention produced improvements in both physiological and physiological aspects in MS (48). In this case, the psychological treatments with the highest recommendation grade are cognitive behavioral therapy (CBT) and interpersonal therapy (IPT) (49). It is worth mentioning that CBT can be administered individually, in a group setting, or by the computer; all of which have shown efficacy in MS patients with low dropout rates (50, 51).
5.1. Limitations
The first limitation of this study was that self-report measures were not used for examining the cognitive status of MS patients. In this regard, the content recorded in the history of patients in the MS Society was used. Previous studies have corroborated the links between cognitive disorders and changes in psychological symptoms (52). The second limitation of this study is that we did not consider the role of the drugs that the patients were taking. This issue can play a role in the appearance of symptoms assessed in this research. Cross-sectional data was another limitation that did not allow authors the possibility to interpret the stability of the predictive validity of DASS-21 over time. However, the following are some of the merits of the present study. In particular, applying relatively stringent restrictions on the control and use of statistical methods can increase the accuracy of the findings. Also, these findings appear to have direct implications for the interpretation of information in future treatment trials, and may be useful in the clinical presentation of patients in various studies and clinical practice guidelines.
5.2. Conclusion
Overall, our study results indicated that symptoms of depression, anxiety, and stress had a significant positive relationship with fatigue and a significant negative relationship with health components. Furthermore, DASS-21 was able to predict a significant proportion of variance of fatigue and eight dimensions of SF-36. Thus, based on the findings, therapeutic interventions for patients’ psychological symptoms to improve their clinical and health dimensions are recommended.