1. Background
Renal disease and renal failure are two leading causes of the global burden of diseases and important causes of death in developing countries. Chronic kidney disease (CKD) is considered one of the main global health issues due to its high prevalence, progression to end-stage renal disease (ESRD), and early death (1-4). CKD emanates from various renal damages and is an irreversible, progressive disease that may progress gradually and lead to the loss of renal function and ESRD (5). The accumulation of toxins, liquids, and electrolytes due to the decreased glomerular filtration will lead to the uremic syndrome or patient’s death if it is not treated effectively with renal replacement therapies such as hemodialysis, peritoneal dialysis, or kidney transplantation (6). In spite of increased life expectancy due to dialysis technologies, patients’ problems, especially those related to systemic or metabolic complications and hemodialysis complications, have increasingly grown (5, 7, 8). The lungs’ mechanical function and ventilation are associated with the kidneys’ function in normal and disease conditions (9).
Pulmonary complications are common in patients with advanced chronic kidney disease.
Pulmonary disorders like pulmonary edema, pleural effusion, acute respiratory distress syndrome, increased pulmonary capillary permeability, pulmonary fibrosis, pulmonary calcification, pulmonary hypertension, hemosiderosis, pleural fibrosis, obstructive apnea, muscle myopathy, and low respiratory muscle strength are observed among these patients (10-13). They might be directly due to uremic toxins or indirectly because of anemia, immune suppression, extra calcification, malnutrition, electrolyte disorders, acid-base imbalance, and volume overload (9, 14-19). On the other hand, ESRD can influence pulmonary ventilation or function directly or indirectly (20).
ESRD is an inflammatory state. Although hemodialysis decreases the fluid overload and improves pulmonary function, the inflammation can affect the respiratory system and mortality rate (13). Few studies have examined the changes in pulmonary function among patients with ESRD treated with hemodialysis and have reported controversial results (11).
2. Objectives
After the Rahgoshai’s study, which was conducted in 2010 on 26 patients, we decided to conduct this study in Zahedan to examine the effects of acute hemodialysis on spirometry parameters.
3. Methods
This was a cross-sectional study conducted among ESRD patients who referred to Ali Ibn Abitaleb Hospital for hemodialysis in Zahedan, Southeast of Iran, in 2016. The Research Ethics Committee of Zahedan University of Medical Sciences approved the study protocol (code of ethics: IR.ZAUMS.REC.1395.288). Informed consent was obtained from all the patients at the time of study enrollment.
The inclusion criteria included patients with ESRD, age above 18 years, records of hemodialysis three times a week at least for three months, KT/V > 1.2, ability to perform PFT, and being hemodynamically stable. The exclusion criteria were being a smoker (currently or recently), having pulmonary diseases such as acute pulmonary infection, asthma, chronic obstructive pulmonary disease, tuberculosis, cardiovascular diseases, neuromuscular disorders, history of chest or abdominal surgery, pulmonary distress, and diuretic users.
Hemodialysis was done using Dialog + B-Braun dialysis machines (Melsungen, Germany) that lasted four hours each time. The blood flow rate varied from 300 to 350 mL/min and the dialysate flow was constant at 500 mL/min. The dialyzer membrane was low-flux biocompatible, and bicarbonate buffer was used. The ultrafiltration rate was based on the patients’ conditions and their weight gain during the interdialytic period. Blood pressure was stable before and after hemodialysis.
Patients’ data including age, gender, and body mass index (BMI) were recorded and spirometry was done one hour before and one hour after hemodialysis with a Spirolab III spirometer (MIR, Roma, Italy). All the spirometry tests were performed by the same technician. The calculated parameters included vital capacity (VC), forced vital capacity (FVC), forced expiratory volume in the first second (FEV1), FEV1/FVC, peak expiratory flow (PEF), and forced expiratory flow between 25% and 75% FVC (FEF 25% - 75%).
Data analysis was carried out using SPSS (Statistical Package for the Social Sciences, version 18, SPSS Inc. Chicago, IL). A paired t-test was used to compare the spirometry parameters before and after hemodialysis. P value of less than 0.05 was considered statistically significant.
4. Results
A total number of 50 ESRD patients (30 men and 20 women) were evaluated. The mean age was 42.40 ± 13.52 for men and 43.05 ± 14.27 for women, respectively. Baseline data of the patients are presented in Table 1, which means of age and BMI were not significantly different between men and women.
| Gender | Number | Age | BMI | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Mean ± SD | Min | Max | P Value | Mean ± SD | Min | Max | P Value | ||
| Male | 30 | 42.40 ± 13.53 | 20 | 69 | 0.781 | 21.65 ± 3.12 | 16.11 | 28.07 | 0.271 |
| Female | 20 | 43.05 ± 14.27 | 23 | 78 | 23.02 ± 5.12 | 17.48 | 39.06 | ||
aValues are expressed as mean ± SD.
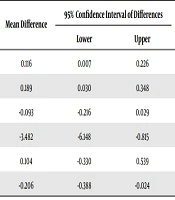
A comparison of PFT before and after hemodialysis is summarized in Table 2. Regardless of gender, comparing post-dialysis PFT parameters to pre-dialysis showed that the means of FVC and FEV1 significantly increased (P = 0.021, P = 0.037 respectively), the means of FEF 25% - 75% and FEV1/FVC significantly decreased (P = 0.027, P = 0.012 respectively), while PEF and VC did not show significant differences.
| Parameter | Values | Mean Difference | 95% Confidence Interval of Differences | P Value | ||
|---|---|---|---|---|---|---|
| Before HD | After HD | Lower | Upper | |||
| FEV1 | 2.093 ± 0.658 | 2.210 ± 0.704 | 0.116 | 0.007 | 0.226 | 0.037 |
| FVC | 2.362 ± 0.821 | 2.551 ± 0.968 | 0.189 | 0.030 | 0.348 | 0.021 |
| VC | 3.736 ± 0.530 | 3.642 ± 0.725 | -0.093 | -0.216 | 0.029 | 0.132 |
| FEV1/FVC | 88.760 ± 10.823 | 85.278 ± 12.934 | -3.482 | -6.148 | -0.815 | 0.012 |
| PEF | 4.586 ± 1.740 | 4.691 ± 1.802 | 0.104 | -0.330 | 0.539 | 0.631 |
| FEF 25% - 75% | 2.802 ± 1.154 | 2.596 ± 1.081 | -0.206 | -0.388 | -0.024 | 0.027 |
Abbreviations: FEF, forced expiratory flow; FEV1, forced expiratory volume in first second; FVC, forced vital capacity; PEF, peak expiratory flow; VC, vital capacity.
aValues are expressed as mean ± SD.
Tables 3 and 4 display the PFT changes after HD in comparison to before HD according to gender. The table shows significant changes in FVC, FEV1 and FEV1/FVC (P = 0.027, P = 0.003, and P = 0.038 respectively) only in men. Data shows no relationship between PFT changes and BMI, solid weight change, or ultrafiltration volume.
| Parameter | Values | Mean Difference | 95% Confidence Interval of Differences | P Value | ||
|---|---|---|---|---|---|---|
| Before HD | After HD | Lower | Upper | |||
| FEV1 | 2.355 ± 0.538 | 2.566 ± 0.573 | 0.217 | 0.077 | 0.344 | 0.003 |
| FVC | 2.747 ± 0.731 | 3.046 ± 0.842 | 0.298 | 0.036 | 0.560 | 0.027 |
| VC | 3.795 ± 0.544 | 3.798 ± 0.545 | 0.032 | -0.034 | 0.041 | 0.836 |
| FEV1/FVC | 87.082 ± 11.440 | 82.928 ± 12.564 | -4.153 | -8.061 | -0.245 | 0.038 |
| PEF | 5.266 ± 1.718 | 4.390 ± 1.771 | 0.123 | -0.604 | 0.852 | 0.730 |
| FEF 25% - 75% | 3.107 ± 1.314 | 2.878 ± 1.237 | -0.229 | -0.508 | -0.049 | 0.103 |
Abbreviations: FEF, forced expiratory flow; FEV1, forced expiratory volume in first second; FVC, forced vital capacity; PEF, peak expiratory flow; VC, vital capacity.
aValues are expressed as mean ± SD.
| Parameter | Values | Mean Difference | 95% Confidence Interval of Differences | P Value | ||
|---|---|---|---|---|---|---|
| Before HD | After HD | Lower | Upper | |||
| FEV1 | 1.761 ± 0.656 | 1.757 ± 0.593 | -0.003 | 0.177 | -0.184 | 0.967 |
| FVC | 1.872 ± 0.662 | 1.922 ± 0.732 | 0.050 | 0.196 | -0.095 | 0.482 |
| VC | 3.660 ± 0.513 | 3.443 ± 0.879 | -0.217 | 0.062 | -0.496 | 0.121 |
| FEV1/FVC | 90.895 ± 9.824 | 88.268 ± 13.064 | -2.627 | 1.171 | -6.426 | 0.165 |
| PEF | 3.722 ± 1.369 | 3.802 ± 1.436 | 0.080 | 0.509 | -0.348 | 0.700 |
| FEF 25% - 75% | 2.414 ± 0.777 | 2.237 ± 0.719 | -0.176 | 0.060 | -0.414 | 0.136 |
Abbreviations: FEF, forced expiratory flow; FEV1, forced expiratory volume in first second; FVC, forced vital capacity; PEF, peak expiratory flow; VC, vital capacity.
aValues are expressed as mean ± SD.
5. Discussion
CKD occurring due to diabetes, hypertension, obesity, and aging is a worldwide health problem. It can lead to ESRD, increased morbidity and mortality, and decreased quality of life. Almost all systems of the body are adversely affected by ESRD, such as respiratory, cardiovascular, and metabolic systems. The respiratory system is affected by ESRD complications and hemodialysis treatment (5).
The results of this study suggest that hemodialysis did not significantly change spirometry parameters in women, while it significantly increased FEV1 and FVC and decreased FEV1/FVC in men.
CKD, which can lead to ESRD, is a general health problem all over the world and impairs the quality of life and mortality. Unfortunately, the prevalence of ESRD is rising along with the increase in diabetes, hypertension, and obesity (21). In ESRD patients, all the body systems are affected, and they suffer from serious respiratory, coronary, and metabolic complications (5, 9).
The male to female ratio in our study was 60%, which may be related to the higher prevalence of CKD among men or the lack of treatment due to costliness for females due to social, cultural, and economic limitations.
As mentioned in the results, the pulmonary function of men significantly improved after hemodialysis compared to before hemodialysis, according to FEV1 and FEC spirometry parameters. Our results on FVC were similar to those of Sharma in 2017 (9) and several other studies (5, 15, 22, 23). FVC increased similar to Rahgoshai et al.’s study (14), but FEV1 increased in the present study, which was not the case in that study. Decreased FVC, restrictive pattern, and decreased airflow in spirometry have been observed in some studies, which can be justified by acute clinical pulmonary edema resulted from increased capillary permeability and hypoalbuminemia (24). Considering the results of FEV1/FVC and FEV1 changes in this study, it was shown that large airways have not been affected by the acute renal failure condition, and the reduction in FEV1 was mainly due to the FVC decrease and restrictive lung disease. Lang et al. (25) in Munich University in Germany in 2006 examined the early effects of hemodialysis on the pulmonary function of 14 patients with ESRD, and unlike our study, they concluded that regardless of the type of used membrane, hemodialysis did not have an early impact on the pulmonary function of uremic patients.
The mean FEV1/FVC had a significant decrease after dialysis in men; however, this difference was not significant for women in this study. Having no significant change in FEV1/FVC for the women after dialysis is justified with the lack of any significant changes in their FEV1/FVC parameters that was similar to Sharma et al.’s study (9). Differences in VC, PEF, and FEF parameters were not significant for all the patients (both men and women) after dialysis compared to before. Rahgoshai et al. (14) similarly examined the short-term effects of dialysis on the respiratory function of 26 patients in Imam Hussein Hospital in Tehran in 2006 and concluded that FVC increased greatly immediately after dialysis ,while no obvious improvement happened for VC, FEV1/FVC, and FEV1. The significant increase in FVC after dialysis in our study and the lack of a relationship between spirometry parameters and BMI are similar to the findings of the mentioned study.
Plesner et al. (26) examined changes in spirometry parameters in COPD patients undergoing dialysis in 2016 and found that improvement in the FEV1/FVC ratio and FEV1 was significantly related to patients’ ultra-filtrated volume; furthermore, when this volume was more than 0.3 of the body weight, a significant improvement in the FEV1/FVC ratio and FEV1 was seen. This is while in our study, there was no relationship between ultra-filtrated volume and spirometry parameters.
Our results are consistent with the findings of some studies and contradictory to others. Moreover, the results of some studies have not been exactly the same as our results. Differences in hemodialysis methods, dialysis duration, membrane type, disease severity, underlying diseases, and even inclusion criteria may be the reasons for this discrepancy. The small sample size in many studies was a limitation to the generalizability of the results.
5.1. Conclusions
In patients with ESRD on maintenance intermittent hemodialysis, hemodialysis may improve pulmonary function tests in men. More larger studies are required to better understand the valid effect of hemodialysis on spirometry parameters.