1. Background
Drug adherence is the rate that the patient follows his/her treatment plan [1]. Poor drug adherence is a major problem in all fields of medicine and psychiatry is not an exception [2]. Drug non adherence has a major role in relapse and re-hospitalization [3]. Patients with mood disorders including major depressive disorder and bipolar mood disorder are a major part of psychiatric patients. They have a high rate of relapse so dug adherence issue has a very important role in these patients [4].
Drug non adherence is associated with different factors including type of illness, patient’s character, drug side effects, patient-doctor relationship [5]. Also it may be the result of costs, personal judgment, cultural or religious ideas about treatment, type of personality and defense mechanisms such as illness denial [6]. Other factors include wrong ideas that drugs are addictive and absence of care giver [7]. Many studies have been conducted to determine the predicting factors of adherence in psychiatric patients. Psychiatric disorders which impair judgment and insight also could result in drug non adherence [8]. Medication side effects [9, 10], youth [7, 10, 11], negative attitude toward medications [9-12], and co-morbid substance abuse [10, 13-16], are well known predictors of non-adherence. Some studies about drug adherence in patients with mood disorder had been conducted in our country, but their findings are paradoxical.
Noncompliance remains one of the greatest challenges when prescribing psychotropic medication and can render any treatment regimen wasteful and ineffective. While rates reported in studies of noncompliance vary widely, non-compliance can clearly increase treatment costs and prolong the duration of hospitalization. Furthermore, noncompliance has a human cost in terms of morbidity and mortality. The causes of non-adherence vary in different regions according to social, cultural, and economic issues.
2. Objectives
Because of the importance of drug adherence in management of the patients we decided to study the factors associated with poor drug adherence in patients with mood disorders in our region.
3. Patients and Methods
Our study was a cohort, prospective and descriptive type study which took place from 2012 to 2013 in Beheshti Psychiatric Hospital in Kerman. One hundred-fifty patients who were hospitalized with primary mood disorders including major depressive disorder, bipolar mood disorder (depressed phase, manic phase or mixed phase) were included. The other criteria included were age more than 18, absence of other psychiatric disorders in axis 1 and duration of hospitalization more than two weeks.
Informed consent was obtained from all patients enrolled in the study. Demographic information was taken (including age, sex, marriage status, level of education, and other information such as: substance abuse, number of drugs, number of re hospitalization, insight) at the time of discharge of the patients. Also a valid form of Drug Attitude Inventory (DAI-10) (Persian translation) was completed for each patient at the time of discharge [17]. This inventory included 10 true-false questions which gained positive total score shows positive drug attitude and negative total score shows negative attitude toward treatment. Drug Attitude Inventory (DAI) is a tool for evaluating patients' cooperation in therapeutic programs [18].
Patients were followed monthly until 6 months through telephone. At the time of follow up DAI-10 was reassessed and completed again. Also the Drug Use Inventory was completed in which patients were asked whether they use their medications or not. The causes of non-adherence which were listed in a checklist were clarified (including forgot, side effects, excessive medications, costs, lack of insight, and recovery from illness). Finally the relation between different variables and drug attitude with drug adherence were assessed.
SPSS 17 was used to statistically analyze and data were assessed with descriptive statistical methods and χ2 test. Also to determine the changes in variable (drug adherence) in a long time the repeated measure ANOVA was used. The relation between variables and drug adherence were assessed by ordinal regression model.
4. Results
Demographic characteristics of the patients are shown in Table 1. Fifty four percent of patients were male. Mean ± SD age of illness onset was 28.17 ± 10.64 years old. Mean ± SD number of medications was 3.91 ± 1.07 and Mean ± SD number of re-hospitalizations was 4.05 ± 3.51. Fifty-six percent of patients had received electroconvulsive therapy and 38% of patients had substance abuse or dependency. Eighty-four percent of patients had insight toward their disorder and 88.7% of patients believed that their physician’s diagnosis was true. During 6 months follow up, 10 patients dropped out. Clinical characteristics about patients have shown in Table 1.
Rate of full compliance in patients was 30.7% and rate of partial and noncompliance were 32.7% and 30% respectively. Factors associated with partial and non-drug adherence, were as follows: forgot (36.7%), side effects (22.7%), high number of medications (14.7%), lack of interest in medicine (28%), recovery of illness (18.7%), lack of confidence in physician’s diagnosis (14%) and not referral to prescription (12%). Rate of compliance according to illness diagnosis are shown in Table 2. There was not a significant relation between illness diagnosis and drug adherence.
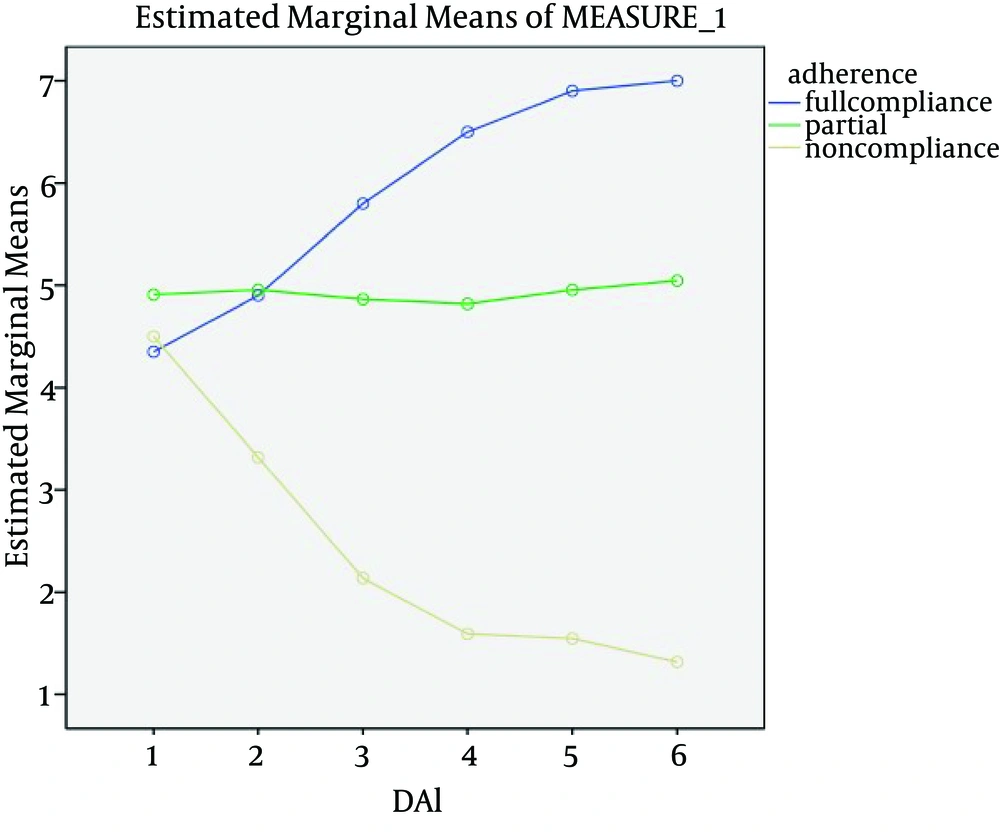
The Mean ± SD DAI-10 score in full compliance group was 5.90 ± 3.54 and Mean ± SD DAI-10 score in partial and noncompliance group were 4.92 ± 2.81 and 2.40 ± 4.27 respectively (Table 3). There was a significant relation between DAI-10 score and drug adherence (Figure 1). Difference of DAI-10 score between full compliance and noncompliance group was significant (P = 0.001), also difference of DAI-10 score between partial compliance and noncompliance group was significant too (P = 0.004). The difference is significant at the 0.05 level. DAI-10 score did not have significant change during time of follow up in each person.
From all studied variables, only DAI-10 score had a significant relation with adherence (P = 0.001) and other variables such as age, sex, marital status, educational level, illness diagnosis, number of medications, and substance abuse did not have a significant relation with drug adherence.
| Variable | No. (%) |
|---|---|
| Single | 47 (31.3) |
| Married | 87 (58) |
| Divorced | 12 (8) |
| Widow | 4 (2.7) |
| Major depressive disorder | 27 (18) |
| Bipolar (depressed phase) | 7 (4.7) |
| Bipolar (manic phase) | 56 (37.3) |
| Bipolar (mixed phase) | 60 (40) |
| ECT | 84 (56) |
| Substance abuse | 57 (38) |
| Insight | 127 (84.7) |
| Trust to physician`s | 133 (88.7) |
Some Demographic Characteristics of Patients
| Diagnosis | Full Compliance, % | Partial Compliance, % | No Compliance, % |
|---|---|---|---|
| 26.9 | 50 | 23.1 | |
| 50 | 33.3 | 16.7 | |
| 34 | 28.3 | 37.7 | |
| 32.7 | 34.5 | 32.7 |
Relation Between Diagnosis and Drug Adherence
| Adherence | DAI Score |
|---|---|
| 5.90 ± 3.54 | |
| 4.92 ± 2.81 | |
| 2.40 ± 4.27 | |
| 4.36 ± 3.86 |
Mean ± SD DAI-10 Score According to Drug Adherence
5. Discussion
In our study, 30.7% of patients had fully complied, 32.7% had partially complied and 30% of them did not comply. It is similar to the results of other studies of Sajatovic et al. [19] in which patients with bipolar disorder under treatment of lithium and anticonvulsant treatment were studied.
A review article that summarized the results of 15 years studies, showed that patients’ failure in drug adherence is a major problem in psychiatric patients with a rate of 4-92% drug non adherence and mean rate of 30 - 35% [20]. Also in Ghaffari-Nejad and Pouya study on 150 psychiatric outpatients, 56 patients (37.4%) had history of early discontinuation of psychotropic medications [21].
In our study rate of full compliance in bipolar (depressed phase) patients was maximum (50%) and in major depressive disorder (MDD) patients was minimum (26.9%). This result indicates that MDD patients had the lowest drug adherence. Also the rate of noncompliance in bipolar (manic phase) was maximum (37.7%) and in bipolar (depressed phase) was minimum (16.7%) although there was no any significant relation between diagnosis and drug adherence.
In a study by Clatworthy et al. [12] on 16 bipolar patients, 81% of patients had partial and noncompliance that is higher than the rate of our study. This could be the result of the low number of cases in this study. In a study about adherence in maintenance phase of treatment among patients with major depressive disorder, results showed that 42% remained adherent in the continuation phase. Younger age, comorbid alcohol, or other substance abuse, comorbid cardiovascular/metabolic conditions, use of older generation antidepressants, and residence in lower-income neighborhoods were associated with lower acute-phase adherence [22]. Also in another study, 31.5% of major depressive disorder patients and 19.5% of bipolar disorder patients had noncompliance [23].
In our study the major factors associated with non-adherence are forget (36.7%), lack of interest in medicine (28%) and side effects (22.7%). In a study by Taj et al. the major causes of noncompliance were side effects (76%) then forget (36%) and cost (22%) [24]. In another study (London) the major causes of noncompliance were patient’s worries about prescribed drugs, side effects, not sure about diagnosis and doubts about need to drug use [20].
In one study the most prevalent factors were no information about benefits of drugs (43%), drug non tolerance (33.5%) and side effects (28.5%) [21]. A meta-analysis estimates that medication non adherence for unipolar and bipolar disorders range from 10 to 60% (median: 40%) and showed that attitudes and beliefs are at least as important as side effects in predicting adherence similar to our study which indicates significant relationship between dug attitude and drug adherence [25].
There is controversial information about the relation between socio-demographic variables with drug adherence. In our study there is no significant relation between demographic factors such as age, sex, educational level, marital status, and substance abuse with drug adherence while in some previous studies claim that treatment non-adherence is associated with substance abuse [9, 10, 12, 15], being unmarried [9, 10], male gender [9-11], young age [10, 13, 14] and low level of education [9]. While some others did not report age [8-10], gender [9, 11], and marital status [9-11] to be associated with adherence.
In our study the only associated factor which had a significant relation with drug adherence was patient’s attitude toward drugs. Patients with higher drug adherence had higher rate of positive attitude toward medications which is similar to many of other previous studies such as Sharifi et al. study on the 76 bipolar patients which showed this issue very well [26].
The rates of non-adherence according to the type of medications (such as anti-depressant, mood stabilizer and anti-psychotics) have not been assessed in current study and further studies must take place to clarify it. Another limitation was telephone follow up. Because of some difficulties for patients such as long distances from patient`s location to hospital we had to telephone follow up to regular follow of them. Further studies with face to face visit are recommended.