1. Background
Pregnancy and childbirth are important for women and their families. The psychological state of the mother undergoes dramatic changes during pregnancy and after childbirth (1) that can predispose her to anxiety during pregnancy, childbirth, and postpartum. Therefore, a comparison of pregnant and non-pregnant women in terms of mood and anxiety suggests that pregnant women may be at increased risk of depression and anxiety disorders (2). In addition, many pregnancies occur under certain conditions, such as chronic maternal illness or poor obstetrics history (3), which exacerbate pregnancy anxiety.
Besides, maternal mental health influences outcomes of normal pregnancy (4, 5), pregnancy-induced by assisted reproductive technology (6), the health and development of the baby (7), and maternal prenatal intention to breastfeed (8) and maternal lifestyle in terms of the alcohol drinking in pregnancy (9). The findings of a systematic review revealed that the adverse effects of anxiety in pregnancy on children’s health are extensive and can be classified into four groups of biological, mental, behavioral, and medical (7). Furthermore, high maternal anxiety increased the likelihood of preterm labor (10) as well as the rate of childbirth fear and a preference for cesarean (11).
Pregnancy anxiety has been shown to be more prevalent than what was expected before. In a Brazilian study, pregnancy anxiety was present in 26.8% of the pregnant women (12). Results of a longitudinal Spanish study showed that the prevalence of pregnancy anxiety was 19.5%, 16.8%, and 17.2%, in the first, second, and third trimesters, respectively (13). Another study in Bangalore City included 380 pregnant women with gestational age less than 24 weeks and without any obstetric complication showed that 55.7% of participants had pregnancy anxiety (14). A study aimed to compare pregnant and non-pregnant women in terms of mood and anxiety suggested that the prevalence rate of any mood or anxiety disorder was 18.2% during pregnancy (2), and finally, the prevalence of anxiety symptoms was reported 15.6 % in early pregnancy (11).
Several risk factors have been shown to be associated with pregnancy anxiety as follows: occupation, previous pregnancy complications, a history of miscarriage or risk of preterm birth (15), the number of abortions, cigarettes smoked daily, and drug use (12, 13), the presence of previous illness and changes in social relationships (13), lower socioeconomic status, low social support and depression (14), younger age (9, 11, 16), low level of education (9, 11, 15), unemployed, psychiatric history of either depression or anxiety (11), unmarried, lower household income (9, 15), nulliparity (9, 16), unplanned-unwanted pregnancy (12, 14, 15), general anxiety (9), adverse physiological symptoms such as vaginal bleeding and fever (15), and nuclear family nature (16).
In assessing pregnancy anxiety, due to the lack of a specific, valid, and reliable Farsi instrument, non-specific pregnancy scales such as the Spielberger State-Trait Anxiety questionnaire have been used, which only measure state or trait anxiety (4). Since a pregnant woman with significant pregnancy anxiety may obtain a score within the normal range of the Spielberger State-trait Anxiety questionnaire, it is necessary to use a specific pregnancy anxiety measurement scale in the studies (17).
Few scales have been developed to measure pregnancy anxiety (4). One of the scales designed to measure pregnancy anxiety is the anxiety scale for pregnancy (ASP) developed by Doyle-Waters et al. (18) and then translated and validated into Farsi. The results of the validation study of the Farsi version of the scale indicated that the instrument had acceptable reliability, content validity, predictive validity, discriminative validity, and concurrent validity (19).
Midwives are among the first caregivers of pregnant women during pregnancy, childbirth, and postpartum. They are responsible for identifying anxious women and providing appropriate advice and care. Therefore, identifying pregnant women with high levels of anxiety using valid and reliable scales is of particular importance in the midwifery field. To the best of our knowledge, few studies were conducted to investigate pregnancy anxiety in Iran using a valid scale.
2. Objectives
The aim of the present study was to investigate pregnancy anxiety associated factors in pregnant women.
3. Methods
The present study is a descriptive-analytical study, which was performed on 322 pregnant women who were admitted to health centers of Sabzevar City from November 2018 to March 2018. Eight health centers were randomly selected in four regions of north, south, east, and west of Sabzevar. Using the SIB system, 40 pregnant women among those who were registered in each health clinic were randomly selected; thus the number of women in the first, second, and third trimesters were proportionate to their number in the center. Midwives in each center were responsible for collecting data according to the list of women’s names provided by SIB system.
Pregnancy in selected women was confirmed based on the first day of the last menstrual period or the first-trimester ultrasound scan. The revised version of the Farsi anxiety scale for pregnancy (F-ASP-R) was distributed to the pregnant women referred to Sabzevar Health centers. The inclusion criteria were reading literacy, willingness to participate in the study, and no psychological disorders required treatment.
The instruments used were demographic questionnaire, the F-ASP-R, and the World Health Organization Psychological Well-being questionnaire (WHO-5 well-being index). The demographic questionnaire included questions about age, employment status, education, parity, a history of miscarriage, and desirability of pregnancy. Doyle-Waters et al. (18) developed the ASP and confirmed its validity and reliability. The original version has 14 items (7 items with negative expression and 7 items with positive expression). The scale has five factors, including infant, labor, marital, attractiveness, and support. Each item is rated on a 4-point Likert scale from 1 (not at all) to 4 (very severe) (18). The minimum and maximum score of this scale are 14 and 56, respectively. This questionnaire was translated and validated in Iran. The results showed that the reliability, content validity, predictive validity, discriminative validity, and concurrent validity were acceptable, but the reliability of the factors was weak. It was suggested that in revising the Farsi version, items with positive expression be converted to items with negative expression, and again, the construct validity and reliability of the scale be checked (19).
In the present study, the revised version with 14 negatively-worded items was used. The WHO-5 was developed by the World Health Organization in several languages, including Persian (20). The validity and reliability of this scale have been investigated in pregnant women in Iran (21). The scale consists of five items with a positive expression that measure one’s well-being and mental well-being over the past two weeks. Items are scored from zero (not at all) to 5 (always), and the lowest and highest possible score on this scale is zero and 25 and can be converted to zero to 100 as well. A score of less than 50 indicates a probability of depression. This scale has been used for screening depression in various studies.
Data were analyzed with SPSS 18 software. Descriptive statistics were calculated. To determine the relationship between variables with pregnancy anxiety, student t-test, and one-way ANOVA were used. Prior to each analysis, the normality of the anxiety scores was tested at the levels of independent variables. Multiple regression analyses were used to examine the relationships between variables and confounding factors. Construct validity was evaluated by confirmatory factor analysis (CFA). The reliability of the scale was assessed by Cronbach’s alpha coefficient. This study with the ethics code IR.MEDSAB.REC.1397.019 was approved by the Research Ethics Committee of Sabzevar University of Medical Sciences.
4. Results
Three hundred and sixteen women filled out the F-ASP-R completely, and six women were excluded because of incomplete completion of the pregnancy anxiety questionnaire. The mean score of the pregnancy anxiety was 32.63 ± 8.9 out of 56, and 49.7% of the study participants scored below the average. The mean age, pre-pregnancy body mass index (BMI), and gestational age of the participants were 28.97 ± 5.9 (year), 25.16 ± 4.4 (kg/m2), and 22.84 ± 10.2 (week), respectively. The F-ASP-R and WHO-5 well-being mean scores were 32.80 ± 8.9 and 58.03 ± 23.0, respectively.
Seventy point seven percent of samples had psychological well-being scores below 50. Forty-four percent and 17.7% of women were in the third and first trimester of pregnancy, respectively. There was no significant correlation between pregnancy anxiety and gestational age, maternal age, BMI, interval from previous childbirth, marriage age and number of sleep hours in the last 24 hours before completing the questionnaire (P > 0.05).
This scale was previously content validated, and the validity and reliability of the questionnaire had been demonstrated, but the reliability of its factors weas poor and needed further investigation. It was possible that disagreement of items wording (positive or negative) impaired structure validity and reduced the reliability coefficient of the scale’s factors; so, in this study, the construct validity and reliability of the scale with confirmatory factor analysis were again evaluated by converting all positive items to negative items. The results showed that compared to the original Farsi version (root mean square error of approximation (RMSEA) = 0.087, standardized root mean square residual (SRMR) = 0.092, chi-square/df = 4.03, comparative fit index (CFI) = 0.87) the revised version with 14 negative items is more valid (RMSEA = 0.08, SRMR = 0.076, chi-square/df = 3.09, CFI = 0.96). The 14 items of pregnancy anxiety scale and Cronbach’s alpha coefficients of the scale factors are shown in Table 1. The reliability of the instrument factors rated 0.556 to 0.815.
| Item Number | Factors | Items | Mean ± SD | Cronbach’s Alpha Coefficient |
|---|---|---|---|---|
| 1 | Fetus | I am worried about the baby’s health | 1.0 ± 2.94 | 0.794 |
| 6 | I am worried that my baby will have a disease or defect | 1.1 ± 3.15 | ||
| 12 | I am worried about my baby being injured during childbirth | 1.0 ± 3.11 | ||
| 2 | Labor | Thinking about the pain of childbirth disturb me | 1.1 ± 2.73 | 0.815 |
| 5 | I am worried about losing control during labor and delivery | 1.1 ± 2.37 | ||
| 14 | I was terrified of feeling powerless during labor pains | 1.1 ± 2.56 | ||
| 8 | Marital | I am worried that I’m not sexually attractive to my husband | 1.0 ± 1.75 | 0.768 |
| 10 | I am unhappy and worried about my husband’s poor participation in this pregnancy | 1.0 ± 1.68 | ||
| 11 | I am worried that my husband won’t support me | 1.1 ± 1.88 | ||
| 3 | Attractive | I am worried about not returning to my previous form after giving birth | 1.1 ± 2.03 | 0.568 |
| 13 | I am worried about the natural changes in my body | 1.1 ± 2.16 | ||
| 4 | Support | I am worried that people in my family and relatives will not care and help me | 1.1 ± 1.92 | 0.664 |
| 7 | I am not sure doctors, nurses, and midwives will take good care of me | 1.0 ± 2.52 | ||
| 9 | I feel worried that I don’t have enough support from people living near me | 1.0 ± 1.84 | ||
| All items | 8.9 ± 32.81 | 0.868 |
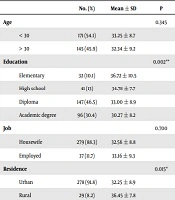
Table 2 shows the distribution of mean pregnancy anxiety scores according to demographic variables. Rural women, women with incomes lower than sufficient, and women with education levels lower than diplomas had higher gestational anxiety than urban women, women with sufficient incomes or higher than sufficient, and women with education higher than diploma, respectively.
| No. (%) | Mean ± SD | P | |
|---|---|---|---|
| Age | 0.345 | ||
| < 30 | 171 (54.1) | 33.25 ± 8.7 | |
| > 30 | 145 (45.9) | 32.34 ± 9.2 | |
| Education | 0.002** | ||
| Elementary | 32 (10.1) | 36.72 ± 10.5 | |
| High school | 41 (13) | 34.78 ± 7.7 | |
| Diploma | 147 (46.5) | 33.00 ± 8.9 | |
| Academic degree | 96 (30.4) | 30.27 ± 8.2 | |
| Job | 0.700 | ||
| Housewife | 279 (88.3) | 32.56 ± 8.8 | |
| Employed | 37 (11.7) | 33.16 ± 9.3 | |
| Residence | 0.015* | ||
| Urban | 278 (91.8) | 32.25 ± 8.9 | |
| Rural | 29 (8.2) | 36.45 ± 7.8 | |
| Income | < 0.001*** | ||
| Less than enough | 59 (19) | 36.80 ± 10.7 | |
| Enough or more | 257 (81) | 31.64 ± 8.2 | |
| Housing | 0.410 | ||
| Tenant | 161 (51) | 33.02 ± 8.9 | |
| Owner | 155 (49) | 32.02 ± 8.8 | |
| Body mass index | 0.988 | ||
| < 18.5 | 16 (5.7) | 32.75 ± 10.8 | |
| 18.5 - 24.9 | 137 (45.7) | 33.54 ± 8.3 | |
| 25 - 29.5 | 104 (35.5) | 32.50 ± 9.0 | |
| > 30 | 39 (13.1) | 33.10 ± 9.5 |
The mean of pregnancy anxiety according to obstetrics variables is shown in Table 3. Women with pregnancy complications, women who were hospitalized during pregnancy, and women with a history of dysmenorrhea had higher pregnancy anxiety scores than their counterparts. Women who attended childbirth preparation classes or had knowledge about analgesia during labor had a lower pregnancy anxiety score than their counterparts. The results showed that the anxiety score of women who wished for cesarean was higher than women who tended to give birth normally.
| No. (%) | Mean ± SD | P | |
|---|---|---|---|
| Parity | 0.246 | ||
| Nullipara | 117 (37.1) | 32.00 ± 8.8 | |
| Primi- or multipara | 199 (62.9) | 33.00 ± 9.0 | |
| Gestational age | 0.239 | ||
| First trimester | 50 (18.5) | 32.07 ± 10.1 | |
| Second trimester | 108 (34.2) | 33.10 ± 8.6 | |
| Third trimester | 124 (39.2) | 31.19 ± 8.6 | |
| Type of pregnancy | 0.027* | ||
| Wanted | 219 (69.3) | 31.90 ± 8.7 | |
| Unwanted or unplanned | 97 (30.7) | 34.29 ± 9.2 | |
| History of abortion | 0.114 | ||
| Yes | 67 (21.2) | 34.64 ± 9.4 | |
| No | 249 (78.8) | 32.50 ± 8.8 | |
| Pregnancy complications | 0.046* | ||
| Yes | 42 (13.3) | 35.02 ± 9.4 | |
| No | 274 (86.7) | 32.22 ± 8.8 | |
| Down syndrome screening | 0.223 | ||
| Yes | 235 (74.4) | 32.33 ± 8.4 | |
| No | 81 (25.6) | 33.78 ± 10.2 | |
| Chronic disease | 0.281 | ||
| Yes | 29 (9.2) | 34.37 ± 7.4 | |
| No | 287 (90.8) | 32.52 ± 8.9 | |
| History of infertility | 0.117 | ||
| Yes | 21 (6.6) | 35.60 ± 10.4 | |
| No | 295 (93.4) | 32.39 ± 8.8 | |
| Hospitalization during pregnancy | 0.046* | ||
| Yes | 22 (7.0) | 36.50 ± 8.9 | |
| No | 294 (93.0) | 32.39 ± 8.8 | |
| Awareness of painless delivery | 0.004** | ||
| Yes | 111 (35.1) | 30.70 ± 8.5 | |
| No | 205 (64.9) | 33.74 ± 9.0 | |
| Attending a childbirth preparation class | 0.043* | ||
| Yes | 93 (29.5) | 31.06 ± 8.2 | |
| No | 223 (70.5) | 33.29 ± 9.2 | |
| Wish for cesarean | 0.035* | ||
| Yes | 107 (33.9) | 34.11 ± 8.8 | |
| No | 209 (66.1) | 31.90 ± 8.9 | |
| History of dysmenorrhea | < 0.001*** | ||
| Not at all | 64 (20.3) | 30.73 ± 8.9 | |
| Sometimes | 120 (38.0) | 31.00 ± 9.2 | |
| Half the cases | 47 (14.9) | 35.73 ± 7.4 | |
| Mostly | 53 (16.8) | 35.59 ± 8.2 | |
| Always | 32 (10) | 35.23 ± 8.9 | |
| Previous delivery method | 0.651 | ||
| Normal | 127 (65.1) | 32.19 ± 8.7 | |
| Emergency cesarean | 20 (10.3) | 34.85 ± 8.7 | |
| Elective cesarean | 48 (24.6) | 32.96 ± 9.7 | |
| Physical activity | 0.048* | ||
| Not at all | 91 (28.8) | 34.18 ± 8.5 | |
| Once a week to daily | 225 (71.2) | 32.00 ± 9.0 |
Table 4 shows the mean of pregnancy anxiety according to psychological variables. Overall, women who described their pregnancy bad or very bad, women who did not feel well, women who had lower psychological well-being, women with unwanted pregnancies, those who received low emotional support from their spouses, and women who were not satisfied with their marital relationships, scored higher pregnancy anxiety than their counterparts.
| No. (%) | Mean ± SD | P | |
|---|---|---|---|
| Mental well-being | 0.012* | ||
| < 50 | 113 (35.7) | 34.45 ± 9.3 | |
| ≥ 50 | 203 (64.3) | 31.81 ± 8.6 | |
| Perceived health | < 0.001*** | ||
| Not at all to low | 30 (9.5) | 40.40 ± 8.4 | |
| Moderate | 89 (28.2) | 33.19 ± 8.6 | |
| Good to very good | 197 (62.3) | 31.27 ± 8.5 | |
| Spouse emotional support | < 0.001*** | ||
| Not at all | 13 (4.2) | 39.30 ± 11.5 | |
| Low to moderate | 56 (17.6) | 37.25 ± 8.5 | |
| Good or very good | 247 (78.2) | 31.45 ± 8.4 | |
| Satisfaction with marital relationship | < 0.001*** | ||
| Not at all to moderate | 43 (13.6) | 38.34 ± 8.4 | |
| Good or very good | 273 (86.4) | 31.93 ± 8.7 | |
| Satisfaction with pregnancy | 0.003** | ||
| Low satisfied | 47 (15) | 34.04 ± 8.9 | |
| Moderately satisfied | 122 (38.5) | 34.59 ± 8.8 | |
| Satisfied/very satisfied | 147 (46.5) | 30.95 ± 8.8 | |
| Satisfaction with the previous delivery | 0.680 | ||
| Low satisfied | 17 (10.4) | 31.76 ± 9.9 | |
| Moderately satisfied | 52 (31.7) | 34.10 ± 9.3 | |
| Satisfied | 78 (47.5) | 32.65 ± 8.5 | |
| Very satisfied | 17 (10.4) | 31.83 ± 9.3 |
Table 5 shows the risk factors of pregnancy anxiety. To investigate the independent risk factors of pregnancy anxiety, the significant variables of Tables 2-4 were separately entered into the multiple regression as independent variables, respectively. The regression was performed by backward method. In the first regression, income (P = 0.001, CI [-6.867, -1.833]) and education (P = 0.035, CI [-4.469, -.170]) remained in the model. In the second regression, a history of dysmenorrhea (P < 0.001), lack of knowledge about analgesia during labor (P = 0.003), a history of hospitalization (P = 0.046), pregnancy complications (P = 0.023), and unwanted pregnancy (P = 0.008) remained in the model. In the third regression, poor emotional support (P = 0.005), perceived poor health (P < 0.001) and lower marital satisfaction (P = 0.036) remained in the model.
| Model | Non-standard Coefficients | Standard Coefficients | t | P | |
|---|---|---|---|---|---|
| B | SE | Beta | |||
| A history of dysmenorrhea (not at all or sometimes vs. often or always) | 3.97 | 0.93 | 0.22 | 4.29 | 0.001*** |
| Spouse emotional support (not to moderate vs. good or excellent) | -3.48 | 0.97 | -0.20 | -3.57 | < 0.001*** |
| Feeling healthy (not at all or slightly vs moderate to very good) | -1.98 | 0.75 | -0.15 | -2.66 | 0.008** |
| Unwanted pregnancy | 2.35 | 0.99 | 0.12 | 2.37 | 0.019* |
| A history of hospitalization in pregnancy (yes vs. no) | -3.60 | 1.77 | -0.105 | -2.03 | 0.044* |
| Lack of awareness about painless delivery (no vs. yes) | 2.30 | 0.98 | 0.12 | 2.36 | 0.019* |
aF = 11.35, P < 0.001, adjusted R square = 0.215; *, P < 0.05; **, P < 0,01; ***, P < 0.001.
The mentioned variables were again entered into multiple regression analysis. The results showed that six variables, including unwanted pregnancy, a history of dysmenorrhea, a history of hospitalization during pregnancy, lack of knowledge about analgesia during labor, poor-perceived health, and receiving poor emotional support from spouse are independent risk factors of pregnancy anxiety (Table 5).
5. Discussion
This study investigated pregnancy anxiety and its social and psychosocial risk factors in pregnant women. Approximately, 50% of the women scored below the average F-ASP-R score. This result is comparable with that of Nath’s study in Bangalore City on 380 pregnant women with gestational age less than 24 weeks which showed that 55.7% of the participants had pregnancy anxiety (14).
The results of the present study indicated no significant difference in pregnancy anxiety scores between the three trimesters of pregnancy, which is similar to results of previous studies (9, 13, 14); however, in a study on 500 low-risk Indian pregnant women, the highest prevalence of pregnancy anxiety was reported during the third trimester of pregnancy (16). In Ding’s study on 990 pregnant women, pregnancy anxiety decreased from the first to the third trimester (15).
Moreover, many variables showed a significant relationship with pregnancy anxiety in this study, but finally, six variables could predict pregnancy anxiety, including unwanted pregnancy, receiving poor emotional support from spouse, a history of hospitalization during pregnancy, poor-perceived health, a history of dysmenorrhea, and lack of knowledge about analgesia during labor.
In a US study on 311 pregnant women, demographic factors such as adolescence, low education, low income, nulliparity, and psychological factors such as unwanted pregnancy and general anxiety were predictive of pregnancy anxiety while age, religion, gestational age, unplanned pregnancy, and symptoms of depression were not independent risk factor for pregnancy anxiety (9). The results of a study in China showed that maternal education, family economic status, unwanted pregnancy, a history of abortion, adverse physiological symptoms such as vaginal bleeding and fever were risk factors for pregnancy anxiety (15). In a Brazilian study on 209 pregnant women, occupation, previous pregnancy complications, a history of miscarriage or risk of preterm birth, unwanted pregnancy, the number of abortions, and the number of cigarettes smoked daily increased the risk of pregnancy anxiety (12). The results of a longitudinal study on 385 Spanish pregnant women indicated that being a smoker, the presence of previous illness, and changes in social relationships were predictive factors of anxiety symptoms (13). In another study in Bangalore City, determinants of anxiety were lower socioeconomic status, low social support, and depression (14). In Rubertson’s study, women under 25 years of age, those with a low level of education or unemployed women, and those with a self-reported history of depression or anxiety were at an increased risk of anxiety symptoms during early pregnancy (11).
The results of a cross-sectional study in the United States showed that pregnancy anxiety was higher in women who had a less positive attitude toward pregnancy. In addition, low family income and poor spousal support were influenced women’s anxiety (22). Another study on 500 low-risk pregnant women in Kerala, India, identified nulliparity, maternal age, and the nuclear family as risk factors for pregnancy anxiety (16).
In the present study, the F-ASP-R with 14 negatively worded items were used (18). The initial Farsi version of the instrument did not show relatively acceptable indices in terms of reliability of the two factors that were likely due to the low number of items in the factor or the presence of positive and negative items in a factor (19). Therefore, the researcher’s suggestion was to revise the scale and to match the expression of the items. In the present study, the confirmatory factor analysis confirmed the structural validity of the revised scale. The internal consistency of the F-ASP-R with 14 negative items was 0.868, which was significantly improved compared to the Cronbach’s alpha coefficient of the F-ASP with both positive and negative items (0.709). The Cronbach’s alpha coefficients of factors were also between 0.556 and 0.815 whereas in the previous version there were three factors with coefficients of 0.18, 0.29, and 0.31 (19). The results of this study make it more likely that item wordings may interfere with the reliability of the scale. There are studies that have yielded similar results (23-25). One study found that negative items often did not correlate with the total score of the scale (26). Another study showed that negative items produce weaker reliability than positive items (27). It should be noted that two recent studies have been conducted on scales that have described a positive concept. Certainly, anxiety is a negative concept that is best described with negative items.
The limitations of this study include limitations on the use of self-administered scales rather than being interviewed by a psychiatrist. The strength point of this study is that it was able to investigate the revised scale’s reliability and validity. It is suggested that in future studies on scale adoption or scale development, the expression of identical items should be noted, and a study on one scale with both positive and negative items once and with identical items (positive or negative) should be performed, and the results compared.
5.1. Conclusions
We found a high level of pregnancy anxiety in this sample. Pregnancy anxiety is predicted by a history of hospitalization, lack of knowledge about analgesia during labor, unwanted pregnancy, poor spousal emotional support, a history of dysmenorrhea, and poor-perceived health.