1. Background
The term gastroenteritis refers to the inflammation of the gastrointestinal tract, which is responsible for the second main cause of mortality in children, especially those under five years of age (1). On average, infants in resource-limited countries experience six episodes annually. The most common manifestations of acute gastroenteritis are vomiting and diarrhea, which is defined as a change in the consistency of stools to loose or liquid and/or an increase in the frequency of defecations to more than three times daily (2).
The most common cause of acute diarrhea in resource-limited countries is infectious gastroenteritis, which is caused by various microbial pathogens depending on the age group, geographical region, and type of diarrhea (3). Acute watery diarrhea is mostly due to Rotavirus, Escherichia coli, and Cryptosporidium, while invasive, or bloody, diarrhea is most often caused by Shigellosis among children in resource-limited settings (4, 5). Among the four species of Shigella — Shigella dysenteriae, S. flexneri, S.boydii, and S. sonnei — S.flexneri is the predominant species in resource-limited countries (6).
Shigellosis usually begins with constitutional symptoms such as malaise, high-grade fever, and anorexia, followed by abdominal cramps, diarrhea, nausea, and vomiting. Initially, it presents with watery diarrhea; however, it may gradually contain mucus or blood (7). Occasionally, shigellosis is accompanied by systemic complications. Bacteremia, metabolic disturbances, leukemoid reaction, reactive arthritis, hemolytic-uremic syndrome, and neurological manifestations, including convulsion or encephalopathy, are among the known extraintestinal complications (8).
Definitive diagnosis of shigellosis is based on stool culture; however, it should be suspected in all patients who present with abdominal cramps, tenesmus, small volume, bloody/mucous diarrhea, and fever, particularly if the stool exam indicates fecal polymorphonuclear leukocytes (9). The mainstay of treatment for shigellosis is the correction of electrolyte and fluid disturbances along with antibiotic therapy if indicated. The choice of antibiotic regimen depends on various factors; however, ceftriaxone is preferred as the first line of parenteral therapy, and azithromycin is the preferred initial oral treatment in children (10, 11).
2. Objectives
In the current study, we investigated the clinical and laboratory findings of patients diagnosed with shigellosis during an outbreak of gastroenteritis in late summer 2022 in our region, which can help in understanding some new clinical aspects of less common Shigella strains.
3. Methods
This cross-sectional study was performed on all children and adolescents who were admitted with diarrhea during an outbreak of gastroenteritis in summer 2022 at Besat Hospital, the referral center for pediatric infectious disease in Hamadan province, Iran. The investigation started when a patient with multi-organ failure, following bloody diarrhea, was referred to our hospital. This case increased our vigilance and awareness of a possible outbreak emerging in a specific region in the west of Iran, and the required actions were immediately started after the referral of subsequent cases.
A probable outbreak case was considered as a previously healthy patient who suddenly developed diarrhea with a history of exposure to a suspected source of infection and a negative stool culture. A confirmed case of the outbreak was defined as an individual who had symptoms compatible with shigellosis, including abdominal cramps, nausea, vomiting, fever, and diarrhea, with a history of exposure to a suspected source of infection and a positive stool culture for Shigella species. A confirmed case of S. sonnei gastroenteritis was defined as an individual presenting with compatible symptoms and exposure history, along with a positive stool culture and serologic evaluation of cultured bacteria for S. sonnei.
Clinical and demographic characteristics such as age, sex, residential area, type of nutrition, date of referral, hospitalization duration, symptoms at the time of admission, prior antibiotic use before hospitalization, degree of dehydration upon arrival, type of treatment, and the need for intensive care unit (ICU) admission were all recorded in a checklist for each case. We also collected available laboratory data such as complete blood count, biochemistry, urine analysis, urine culture, stool analysis, and stool culture for each patient.
An investigation of the possible primary source of infection according to the patient's exposure history was also performed by the environmental health service, and several samples of common water and food sources of diagnosed patients were evaluated. To identify Shigella species, stool cultivation was done on xylose lysine deoxycholate (XLD) agar (Condalab, Spain) and eosin methylene-blue lactose sucrose (EMB) agar (Condalab, Spain). After 24 hours, lactose-negative colonies suspected of Shigella were cultured on differential media, including triple sugar iron (TSI), sulfur, indole, motility (SIM), methyl red Voges Proskauer (MR-VP), Simmons citrate agar, lysine decarboxylase agar, urea agar, and phenylalanine deaminase (PDA) agar (all from Ibresco, Iran). After initial confirmation of Shigella species, antisera specific to Shigella species (Baharafshan, Iran) were used to confirm the isolates phenotypically.
To determine the antibiotic sensitivity of the isolates, an antimicrobial susceptibility test was performed using the disk diffusion method according to the guidelines of the Clinical and Laboratory Standards Institute (CLSI 2023) on Mueller Hinton Agar medium (Condalab, Spain). The susceptibility profiles were determined for cefixime (30 μg), ceftriaxone (30 μg), ciprofloxacin (5 μg), imipenem (10 μg), cotrimoxazole (1.25/23.75 μg), cephalexin (10 μg), azithromycin (15 μg), amikacin (30 μg), and levofloxacin (5 μg) antibiotics (HiMedia BioSciences Company).
Qualitative and quantitative variables were presented by mean ± SD and frequency (%), respectively. Chi-square and Fisher’s exact test were used to determine the association between two classification variables. The SPSS (version 16) software was used to analyze the data. The significance level in this study was less than 0.05. The study was approved by the ethics committee of Hamadan University of Medical Sciences (IR.UMSHA.REC.1401.490).
4. Results
In the current study, 43 cases were included. Among them, 22 cases (51.2%) were male. The average age of the patients was 93.21 months with a standard deviation of 41.8 months. Patients were hospitalized for a minimum of 2 days and a maximum of 7 days (4.29 ± 1.2). A total of 69.2% of patients were fed with breast milk, 15.4% with breast milk and formula, and 7.7% with formula alone.
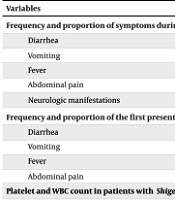
The first clinical manifestation in 59.4% of children was diarrhea, followed by vomiting, fever, and abdominal pain. Diarrhea was the most common manifestation at 100%, with 57.6% of cases being bloody. Other common manifestations were vomiting, fever, abdominal pain, and neurological manifestations in decreasing order of frequency. Detailed frequencies and proportions are presented in Table 1. The average measured temperature of the patients was 38.59 degrees Celsius, with a standard deviation of 0.75.
| Variables | No. (%) |
|---|---|
| Frequency and proportion of symptoms during the disease period a | 43 (100) |
| Diarrhea | 32 (74.4) |
| Vomiting | 31 (72.1) |
| Fever | 28 (65.1) |
| Abdominal pain | 15 (53.6) |
| Neurologic manifestations | |
| Frequency and proportion of the first presenting symptoms a | 19 (44.2) |
| Diarrhea | 5 (11.6) |
| Vomiting | 4 (9.3) |
| Fever | 4 (9.3) |
| Abdominal pain | |
| Platelet and WBC count in patients with Shigella gastroenteritis | |
| WBC b | |
| 2500 - 10000 c | 29 (69.0) |
| 10000 - 15000 | 9 (21.4) |
| 15000 - 20000 | 3 (7.1) |
| < 2500 | 1 (2.4) |
| Platelet b | |
| < 150000 c | 1 (2.4) |
| 150000 - 450000 | 40 (95.2) |
| > 450000 | 1 (2.4) |
Abbreviation: WBC, White blood cell.
a Due to symptom overlap, the total percentage does not sum to 100%.
b One patient did not have blood sample, so the results are related to 42 cases.
c Number per microliter (µL).
The most common neurological symptoms observed were headache (11 cases, 39.3%), decreased level of consciousness (3 cases, 10.7%), and seizure (1 case, 3.6%). Additionally, 46.4% of patients did not exhibit any neurological symptoms. There was no significant relationship between neurological symptoms and age, gender, and occurrence of fever in patients.
Regarding antibiotic usage, eight patients (18.6%) had been treated with antibiotics prior to admission, including amoxicillin, co-amoxiclav, cefixime, ceftriaxone, and cotrimoxazole. Dehydration status was determined for 31 cases upon hospitalization. Among these cases, 17 patients (54.8%) were found to have dehydration, with 54.5% experiencing mild dehydration, 27.3% experiencing moderate dehydration, and 18.2% experiencing severe dehydration. Additionally, eight patients required admission to the ICU.
During their hospital stay, 39 patients (90.7%) received antibiotics, while four patients improved with rehydration therapy alone, without the need for antibiotics. Five patients showed improvement with ceftriaxone. However, stool culture results later identified S. sonnei resistant to ceftriaxone and sensitive to ciprofloxacin. As a result, antibiotic therapy was switched from ceftriaxone to ciprofloxacin in three patients, and ciprofloxacin was used as the first-line treatment in subsequent cases requiring antibiotics. Only one patient (2.3%, the first referred patient) died during the study period, while the rest fully recovered (clinical success rate: 97.7%).
In terms of laboratory findings, 26 out of 43 patients (60.47%) had a red blood cell (RBC) count higher than five, and 33 out of 43 patients (76.74%) had a white blood cell (WBC) count higher than five in their stool analysis. As indicated in Table 1, blood sample WBC counts were 2500 - 10000 per microliter (µL) in most patients. Additionally, one patient had a platelet count below the normal level. Furthermore, six out of 39 patients (15.38%) had a WBC count higher than five, and eight out of 39 patients (20.51%) had a RBC count higher than five in their urine analysis. The patient who expired due to multiorgan failure was one of the cases with higher-than-normal RBC and WBC counts in urinalysis (urinalysis was performed in 39 cases during this evaluation).
Of the total patients, four cases had a serum sodium level below 130 mg/dL (hyponatremia), while the remaining patients had levels within the normal range. As for potassium levels, four patients had levels below 3.5 mg/dL (hypokalemia), three patients had levels above 4.5 mg/dL (hyperkalemia), and the rest had normal levels. Furthermore, one case showed elevated AST levels, but there were no reported cases of abnormal ALT levels. In 13 patients (30.2%), the BUN/Cr ratio was higher than 20, which indicates dehydration. The stool culture results of 28 patients (65.1%) were positive for S. sonnei, and the rest were negative. All cases of S. sonnei that grew in stool culture were resistant to cefixime, ceftriaxone, cotrimoxazole, cephalexin, and azithromycin and were sensitive to amikacin, ciprofloxacin, levofloxacin, and imipenem.
5. Discussion
Investigation of outbreaks is a valuable way of gaining information about the pattern of infectious diseases and antibiotic resistance in a region. Here, we discuss an outbreak of shigellosis to provide an epidemiologic view of this disease in Iran.
Shigellaflexneri is the leading cause of dysentery in developing countries; however, S. sonnei is becoming increasingly prevalent in these regions (12). Moradi et al. evaluated the frequency of various Shigella species in Iran from 2000 to 2020, and they reported S. sonnei as the predominant type in Iran (cause of dysentery in 54.1% of cases). Shigellaflexneri, S.dysenteriae, and S.boydii were the next common culprits (13). Another study evaluating the pattern of Shigella infection from 2016 to 2022 in the south of Iran reported that the leading species has changed from S.flexneri to S. sonnei in the last three years of this study (14). Consistent with these recent epidemiological studies in Iran, the investigated outbreak was caused by S. sonnei, and this organism was detected in 65.1% of stool cultures. Shigellosis is known to be more prevalent in children under 10 years of age and in boys; however, the recent study in the south of Iran and our investigation showed similar prevalence among both genders (14).
The main clinical features of shigellosis are known as diarrhea, abdominal pain, and vomiting (12). In the evaluation of the mentioned outbreak, we also detected similar clinical presentations among patients. For example, all cases had diarrhea, and it was the first presentation in the majority of cases. Vomiting, fever, and abdominal pain were the next common features among patients. According to previously available data, the most prevalent extraintestinal manifestation of shigellosis is neurological symptoms and signs (12). The investigation of the current outbreak also showed compatible results, as more than half of the cases had various degrees of neurological complications, from headaches to seizures.
Although the risk of death is generally lower with S. sonnei compared to other Shigella species, one fatality occurred in our study. This patient was the first referred to our center with multi-organ failure and severe renal failure, likely due to bacteremia and septicemia. Antibiotic resistance and choosing the best antibiotic regimen for shigellosis is a challenging issue nowadays. Cefixime and ceftriaxone are considered acceptable antibiotic regimens for candidates of oral and intravenous treatments, respectively. While some experts recommend ciprofloxacin only as a backup therapy for severe forms of the disease, the World Health Organization (WHO) recommends it as the first-line treatment for shigellosis across all age groups, even with past concerns about quinolone-related joint side effects in children (12, 15).
In our investigation, all cases of S. sonnei that grew in stool culture were resistant to cefixime, ceftriaxone, cotrimoxazole, cephalexin, and azithromycin. They were sensitive to amikacin, ciprofloxacin, levofloxacin, and imipenem. Consistently, a systematic review and meta-analysis by Baharvand et al. reported that the prevalence of resistance to ciprofloxacin was 3%, while there were resistance rates of 28% for ceftriaxone and 35% for cefixime (16). Another notable finding from this study was an upward trend in resistance rates over the last two decades, with ciprofloxacin increasing from zero to six percent and ceftriaxone from six to 42 percent (16). These results justify the usage of ciprofloxacin as the first-line therapy for shigellosis, especially in severe cases. The study conducted in southern Iran also reports the lowest resistance rate for ciprofloxacin, which supports the appropriateness of using ciprofloxacin as first-line therapy in an outbreak in Iran (14).
On the other hand, concerns about joint-related side effects have led to the Iranian Integrated Management of Childhood Illness (IMCI) recommending cefixime as the first-line treatment, with ciprofloxacin used only if there is an inadequate response. However, based on the results of our study, we recommend that, in line with the WHO's guidance, ciprofloxacin should also be the first-line outpatient treatment in our country (15). Additionally, all cases in our study were resistant to ceftriaxone, so intravenous ciprofloxacin should also be considered for inpatient management, if necessary.
The main limitation of this study is the absence of a shigellosis surveillance system in our region prior to the outbreak. As a result, we lack sufficient data to compare sporadic shigellosis cases with those that occurred during the outbreak in terms of clinical manifestations and antibiotic resistance patterns. We recommend establishing a surveillance system for shigellosis to monitor disease trends and enable timely outbreak detection.
5.1. Conclusions
Although shigellosis is usually associated with low mortality rates, careful monitoring of cases is necessary as it can lead to death in some patients with severe infection. All cases in this study were infected with the S. sonnei serotype and were resistant to third-generation cephalosporins. Given this experience, we recommend that in the event of an outbreak or increased prevalence of shigellosis in a region, clinicians should consider uncommon microbial sources and make timely efforts to identify the type and patterns of antibiotic resistance to effectively control the outbreak. Furthermore, it is advised that the first-line treatment in Iran should also align with the WHO's guidelines, which recommend ciprofloxacin.
Shigellosis is typically associated with low mortality rates; however, careful monitoring of cases is essential, as it can lead to death in some severe instances. In the event of an increased prevalence of shigellosis in a region, clinicians should consider uncommon microbial sources and patterns of antibiotic resistance. This approach is crucial for effectively managing outbreaks and ensuring appropriate treatment. In alignment with the WHO's recommendation, ciprofloxacin is advised as the first-line treatment in Iran. This recommendation is based on its efficacy and the observed resistance patterns to other antibiotics.