1. Background
Demodex species are mites with a cosmopolitan distribution, having adapted to a wide range of climatic conditions, and they represent a significant public health concern, particularly in underdeveloped countries (1). Among the diverse microorganisms residing on and within the human body, Demodex mites are among the most common commensal arthropods, predominantly inhabiting the pilosebaceous units of the facial skin (2).
Demodex species are permanent ectoparasites belonging to the order Acarina of the class Arachnida (3). Also, they belong to the family Demodicidae, are represented by seven genera, and almost 108 species. More than 100 species of Demodex have been identified; however, only two species, Demodexbrevis (Akbulatova, 1963) and D.folliculorum (Simon, 1842), are known to inhabit the human body (4-7). Demodex species undergo several developmental stages during their life cycle. Mating occurs between mature males and females approximately half a day after reaching adulthood, after which eggs are deposited within hair follicles or sebaceous glands. The six-legged larvae that emerge subsequently pass through two nymphal stages before developing into adults. These mites have a relatively short lifespan, typically ranging from 14 to 18 days, and spend their entire life cycle on the host (8-10).
These mites are predominantly found on the human face, particularly in the regions of the forehead, nose, cheeks, and chin. The most common species affecting human skin are D.folliculorum and D.brevis (11). Demodexfolliculorum lives in clusters within the funnel-shaped portion of hair follicles, whereas D. brevis, which is shorter in length, inhabits the deeper parts of sebaceous or meibomian glands. Adult D.folliculorum is 0.3 - 0.4 mm in length and that of D. brevis is 0.15 - 0.2 mm in length. Their bodies are covered with scales and they have pin‑like mouth parts for eating oils, skin cells, and hormones gathering in the hair follicles (6). Both species feed on sebum for nutrition and survival. In addition, D.folliculorum can be found in the eyebrows, eyelashes, and meibomian glands, where its presence may be associated with Demodex blepharitis (3, 4).
Demodex mites affect the skin of the nose, forehead, chin, and cheeks, and are characterized by flushing followed by erythema due to capillary dilation, along with papules and pustules resembling acne (12, 13). Several factors have been reported to promote the proliferation of Demodex mites. These include age, gender, occupation, education level, using facial cosmetics, personal hygiene, washing the face regularly, immune suppression, environmental stress, hypervascularization (excessive blood vessel formation), poor personal hygiene, sharing hygiene items (such as towel, soap), high density of sebaceous glands, and hyperplasia (enlargement) of the sebaceous glands. A few studies have investigated the influence of pH, skin moisture, and temperature on the abundance of Demodex mites (4, 14-16).
Demodex dermatitis is primarily transmitted through the use of shared personal items, close physical contact, and poor hygienic practices. Although these mites typically exist as harmless commensals on the human body, an increase in their numbers can lead to pathogenic effects and cause demodicosis. Demodicosis is most often observed in folliculitis. Depending on the location, it can cause small pustules at the base of a hair shaft on congested, inflamed skin. Demodicosis can also cause swelling, itching, and erythema of the eyelid margins. Under normal conditions, they coexist with the host without causing pathology; however, factors such as frequent use of cosmetic products on the skin, inadequate facial cleansing, increased sebum secretion (especially with sweating in warm climates), and steroid use can convert them into disease-causing agents.
Demodex mites facilitate bacterial proliferation by creating a favorable microenvironment, leading to intense skin reactions, visible pigmentation changes, and abscess formation. These mites play a critical role in the etiology and pathogenesis of several dermatoses, including acne vulgaris (a chronic inflammation of unknown etiology, affecting young adults and characterized by skin with comedones, papules, pustules, nodules, cysts, etc., mostly affecting follicles and sebaceous glands), rosacea (a common skin condition of uncertain etiology, which usually affects the center of the face among the middle-aged, causing transient or permanent facial erythema, telangiectasia, edema, papules, pustules, nodules, and scars), eczema, perioral dermatitis, seborrheic dermatitis (a common condition with uncertain etiology that makes the skin greasy, scaly, and flaky, and occasionally itchy and inflamed; areas of the skin rich in oil-producing glands are often affected, including the scalp, face, and chest), folliculitis (inflammation of the hair follicles of the skin), and blepharitis (characterized by inflammation, swelling, scaling, reddening, burning, itching, and crusting of the eyelid).
Nevertheless, the severity of the pathology varies depending on the age and immune status of the host (8, 17). Comedones are created whenever the preserved keratinous and sebum material close the follicle pore; comedones are thought to be more abundant in people with oily skin (large pores). Demodicosis raises the sebum secretion, making the skin greasier, which is a suitable situation for the expansion of comedones. As a result, it seems that the presence of Demodex raises the abundance of comedones (18).
Demodex infestation is reported to be up to 80% in people with healthy skin (19), with prevalence potentially increasing in elderly individuals (17). In Iran, studies on Demodex infestation have demonstrated prevalence rates ranging from 15.2% in healthy individuals to 68.3% in patients presenting with clinical manifestations (19, 20). The investigation of ectoparasite infestation and the examination of factors involved in their pathogenicity can contribute to the development of improved strategies for their control, reduction of treatment costs, and combating them in an environmental manner.
The methods used to sample Demodex spp. generally include hair epilation, skin scraping, skin pressurization, cellophane tape (CTP) method, skin biopsy, comedo extraction, standard skin surface biopsy, and so on.
2. Objectives
The primary objective of this study was to assess the prevalence of Demodex ectoparasite infestation among individuals presenting to the Comprehensive Health Center in East of Ahvaz, and to evaluate associated risk factors using two sampling methods: The CTP method (with gentle pressure) and skin pressurization in the year 2022 - 2023.
3. Methods
In this cross-sectional descriptive study, according to various studies, the prevalence of Demodex infestation was estimated at 38% (11), and assuming a margin of error of 0.02 with a 95% confidence level, a sample size of 225 male and female volunteers was randomly selected from individuals attending the Comprehensive Health Center in East of Ahvaz. The sample size was determined by using a single population proportion formula:
Signed consent forms were collected from the participants after the study was fully explained to them. Ethical permission was not required for this study because the skin pressurization and CTP methods were two non-invasive sampling techniques routinely used in etiological agent investigations. Confidentiality of the data was retained at all levels of the research. The study was conducted in accordance with the principles of the Declaration of Helsinki. Exclusion criteria included individuals who had received any topical or related treatments within the past month.
Each person was interviewed individually. The questionnaire was filled out by face-to-face interview. The information on age, gender, family address, telephone number, occupation, literacy level, skin type, skin disease, use of facial cleaner, use of cosmetics, sanitary ware sharing, and frequency of face-wash per day were collected in the study.
After completing the questionnaire, samples were collected from four facial regions (nose, cheek, chin, and forehead) using two methods: The CTP (scotch tape) method with very mild pressure and the skin pressurization method (pressure technique). Sampling was preferred particularly in areas with skin lesions. The patients’ faces were cleaned with alcohol or washed with warm water (to remove any residual cream or lotion) and allowed to air dry.
For the pressure technique, the skin in the specified areas (about 1 cm2) was compressed using the thumb, and the expressed sebum was collected onto a glass slide. Samples were placed directly on a clean slide, followed by the application of one or two drops of 10 - 20% potassium hydroxide solution [other materials that can be used include: Glycerin, lactophenol, liquid paraffin, or Hoyer solution for the permanent slides (20 mL of glycerin, 30 g of crystalline gum Arabic, 50 ml of distilled water, and 200 g of chloral hydrate)] for clearing. After placing a coverslip on the slide containing the sample, microscopic examination at magnifications of 4x, 10x, and 40x was performed for the presence of Demodex mites during two to three hours. Then, slides were coded. Each participant had four slides prepared.
For sampling using the CTP method (with slight pressure), all participants were instructed to apply pieces of transparent adhesive tape approximately 2 cm × 5 cm to the forehead, cheek, chin, and nose at night before bedtime. The tape was pressed gently to ensure better contact with the skin. The following morning, the tape strips were removed from the face and pressed onto microscope slides (one slide per sampled area, four slides per individual) for subsequent analysis. Lastly, the tapes were observed under an optical microscope.
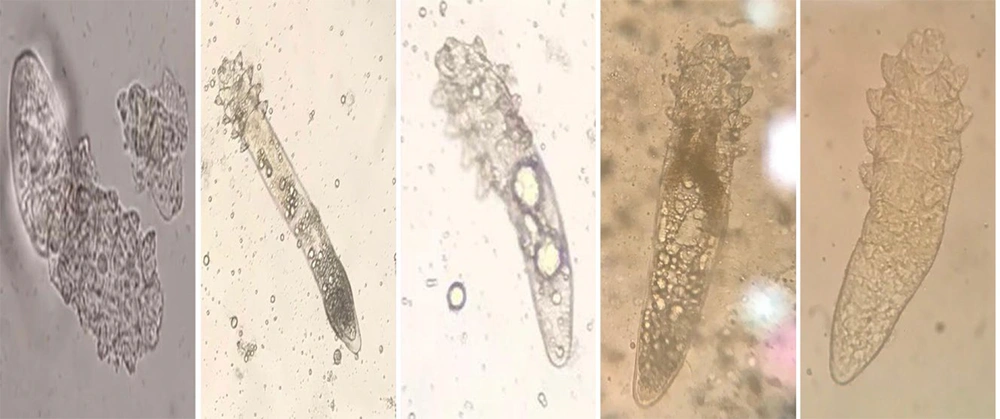
Positive samples were photographed, and identification of Demodex mites was performed by comparing their morphological characteristics and parameters described in the literature and standard references (21, 22). A positive diagnosis was made only after visualizing the Demodex mites (any of the developmental stages: Egg, larva, nymph, adult of D. folliculorum or D. brevis) under microscope magnification. The infestation intensity was classified based on the number of mites counted per individual across eight slides into three categories: Mild (1 - 8 mites/8 slides), moderate (9 - 18 mites/8 slides), and severe (19 or more mites/8 slides).
The research findings were analyzed using descriptive statistics (frequency and percentage) and analytical statistics with Fisher’s exact and chi-square tests in SPSS for Windows version 13.0 software (SPSS Inc., Chicago, IL, USA).
4. Results
In the study population of 225 randomly selected individuals, laboratory examinations and clinical assessments identified 129 cases of Demodex infestation, with a prevalence rate of 57.3%. All infested individuals were affected with D.folliculorum (Figure 1); D.brevis was not detected in this study. The gender distribution of infested cases was 50.3% female and 49.7% male, with no statistically significant difference between sexes (P = 0.59). The study included participants over 20 years of age, with the highest infestation rate among those aged 51 and above (46.5%). A significant difference in infestation rates was observed across age groups (P < 0.001).
Regarding education level, the majority of participants (56.5%) had a university education; similarly, 44.2% of infested individuals were university educated, but no significant difference in infestation prevalence was found based on education level (P = 0.06). Occupational status was also evaluated, with housewives showing the highest infestation rate (45.8%), and a significant difference in infestation among different occupations (P < 0.001). Skin types were categorized as dry, normal, and oily, with the highest infestation prevalence (40.4%) among individuals with oily skin, showing a significant difference (P < 0.001).
Among users and non-users of facial cleansing agents, infestation rates were 38% and 62%, respectively, indicating a significant difference (P < 0.001). Infestation rates among users and non-users of cosmetic products were 60.5% and 39.5%, respectively, with a significant difference (P < 0.001). Participants using personal versus shared hygiene products had infestation rates of 31.1% and 68.9%, respectively, with a statistically significant difference (P < 0.001). Frequency of facial washing was assessed, with 56.6% of infested individuals washing their face once daily, and a significant difference was observed compared to those washing two or more times daily (P < 0.001).
Individuals with acne and pimples represented the highest infestation among skin disease groups (46.5%), with significant differences in infestation rates among various skin disease patients (P < 0.001). Infestation severity, classified by mite count on eight slides, showed 72.1% of individuals with mild infestation; differences among mild, moderate, and severe infestation categories were statistically significant (P < 0.001, Table 1). The highest and lowest infestation rates by facial area were in the nose (50.2%) and chin (6.2%), respectively, with a significant difference among facial regions (P < 0.001). The difference in infestation rates between CTP (with slight pressure) and skin pressure methods (Figure 2) was also significant (P < 0.001, Table 2).
| Characteristics and Descriptions | Distribution | Prevalence of Demodex | Test | P-Value |
|---|---|---|---|---|
| Gender | Fisher exact | 0.59 | ||
| Male | 112 (49.7) | 68 (52.7) | ||
| Female | 113 (50.3) | 61 (47.3) | ||
| Age (y) | Chi-square | < 0.001 b | ||
| 20 - 35 | 63 (28.0) | 31 (24.0) | ||
| 36 - 51 | 99 (44.0) | 38 (29.5) | ||
| ≥ 51 | 63 (28.0) | 60 (46.5) | ||
| Literacy level | Chi-square | 0.06 | ||
| Under diploma | 65 (28.8) | 51 (39.5) | ||
| Diploma | 33 (14.7) | 21 (16.3) | ||
| Collegiate | 127 (56.5) | 57 (44.2) | ||
| Occupation | Chi-square | < 0.001 b | ||
| Housewife | 105 (46.7) | 59 (45.8) | ||
| Worker | 13 (5.8) | 10 (7.8) | ||
| Self-employment | 26 (11.6) | 8 (6.2) | ||
| Farmer | 14 (6.2) | 11 (8.5) | ||
| Unemployed | 13 (5.8) | 6 (4.6) | ||
| University student | 21 (9.3) | 14 (10.9) | ||
| Government employee | 30 (13.3) | 19 (14.7) | ||
| Other | 3 (1.3) | 2 (1.5) | ||
| Skin type | Chi-square | < 0.001 b | ||
| Dry | 54 (24.0) | 33 (25.5) | ||
| Neutral | 99 (44.0) | 44 (34.1) | ||
| Oily | 72 (32.0) | 52 (40.4) | ||
| Skin disease | Fisher exact | < 0.001 b | ||
| Yes | 180 (80.0) | 121 (93.8) | ||
| No | 45 (20.0) | 8 (6.2) | ||
| Use of facial cleaner | Fisher exact | < 0.001 b | ||
| Yes | 162 (72.0) | 80 (38.0) | ||
| No | 63 (28.0) | 49 (62.0) | ||
| Using cosmetics | Fisher exact | 0.01 b | ||
| Yes | 135 (60.0) | 78 (60.5) | ||
| No | 90 (40.0) | 51 (39.5) | ||
| Sharing sanitary ware | Fisher exact | 0.002 b | ||
| Shared | 153 (68.0) | 89 (68.9) | ||
| Unshared | 72 (32.0) | 40 (31.1) | ||
| Frequency of face-wash (d) | Chi-square | < 0.001 b | ||
| 1 | 81 (36.0) | 73 (56.6) | ||
| 2 | 108 (48.0) | 41 (31.8) | ||
| ≥ 3 | 36 (16.0) | 15 (11.6) | ||
| Skin disease | Chi-square | < 0.001 b | ||
| Acne and pimple | 89 (39.6) | 60 (46.5) | ||
| Dermatitis | 9 (4.0) | 6 (4.7) | ||
| Rosacea | 15 (6.6) | 13 (10.1) | ||
| Blepharitis | 13 (5.8) | 8 (6.2) | ||
| Redness | 23 (10.2) | 16 (12.4) | ||
| Itching | 18 (8.0) | 11 (8.5) | ||
| Flacking | 13 (5.8) | 7 (5.4) | ||
| None | 45 (20) | 8 (6.2) | ||
| Degree of infestation | Chi-square | < 0.001 b | ||
| Mild | - | 93 (72.1) | ||
| Moderate | - | 27 (20.9) | ||
| Severe | - | 9 (7.0) | ||
| Degree of infestation in people with skin disease | Chi-square | < 0.001 b | ||
| Mild | - | 66 (51.1) | ||
| Moderate | - | 34 (34.1) | ||
| Severe | - | 19 (4.7) |
a Values are expressed as No. (%).
b The difference was statistically significant.
| Characteristics and Description | Distribution | Prevalence of Demodex | Test | P-Value b |
|---|---|---|---|---|
| Checkpoint | Chi-square | < 0.001 | ||
| Nose | 225 (100) | 113 (50.2) | ||
| Cheek | 225 (100) | 22 (9.8) | ||
| Chin | 225 (100) | 14 (6.2) | ||
| Forehead | 225 (100) | 81 (36.0) | ||
| Detection method | Chi-square | < 0.001 | ||
| CTP with a slight squeezing | 225 (100) | 121 (53.8) | ||
| Skin pressurization | 225 (100) | 41 (18.2) |
Abbreviation: CTP, cellophane tape.
a Values are expressed as No. (%).
b The difference was statistically significant.
5. Discussion
In the present study, the overall prevalence of Demodex infestation in the study population was determined to be 57.3%. The detection rate of Demodex using the CTP method was 53.8%, while the skin squeezing method yielded a detection rate of 18.2%.
Demodex infestation is considered common. Other studies have shown that 10% to 80% of healthy individuals (without clinical cutaneous manifestations) may be infested with Demodex (5). In two large studies conducted in China, the detection rate was reported to be 67.6% among 756 university and school students (aged 13 to 22 years) using the CTP method, and 43% in 860 patients with dermatosis (aged 12 to 84 years) using the skin squeezing method (15, 23). In a study by Shokrani et al. on 100 college students in Khorramabad (western Iran), the overall prevalence of Demodex infestation was 55%. The detection rate by CTP method (52%) was significantly higher than that by the skin squeezing method (17%) (24). The CTP method is considered an appropriate and non-invasive technique for epidemiological studies. This method is designed based on the parasite’s biology, considering its movement and mating behavior at night.
All specimens found in this study were D.folliculorum. This is in agreement with other research where D. folliculorum was the most abundant species (4). It is completely feasible that D. folliculorum is more abundant in human skin; although, the fact that it lives in the hair follicles makes finding it simpler than D. brevis, which lives in the deeper sebaceous and meibomian glands. Therefore, it is not always feasible to detect D. brevis except when it creeps onto the skin level during the night.
In the present study, the prevalence of Demodex infestation among males was 52.7%, with no statistically significant difference compared to females. In several other studies, the association between gender and Demodex infestation was also found to be statistically insignificant (5, 25). However, in the study conducted by Shokrani et al., the prevalence of Demodex infestation was significantly higher in males (66%) than in females (44%) (24). This finding can be attributed to the higher number of sebaceous glands in males, which may favor Demodex proliferation (26).
The present study was conducted among individuals aged over 20 years. The highest prevalence of Demodex infestation was observed in the age group of 51 years and above (46.5%), and a statistically significant difference was found in the frequency of infestation among different age groups. Similarly, other studies have also demonstrated that the prevalence of Demodex infestation increases with age. Due to the low sebum secretion in children, the mite is rarely observed in this group (8, 27, 28). In another study, the prevalence of Demodex infestation was approximately 95% in individuals over 71 years old, 69% among those aged 31 to 50 years, and only 13% in children aged 3 to 15 years (29). Several studies have indicated that the highest prevalence of Demodex infestation occurs between the ages of 30 and 60 years (30). The findings of the present study are consistent with those of previous research.
In our results, 32.0% of the total study population had oily skin. Among the 129 individuals diagnosed with Demodex infestation, 44.4% had oily skin, and a statistically significant difference was observed compared to those with normal or dry skin. Since Demodex mites typically inhabit sebaceous glands or hair follicles, oily skin provides a favorable environment for their colonization and proliferation. This is because sebaceous glands can supply abundant nutrients necessary for the reproduction of Demodex (6). In the study by Shokrani et al., the highest prevalence of infestation was reported among individuals with oily skin (67.5%) (24). Similarly, in a study conducted by Zhao et al. in China, the highest rate of infestation (48.8%) was also found in participants with oily skin (23). The findings of the present study are consistent with those of previous research. Some studies have also reported a sensation of skin dryness in individuals with severe Demodex infestation, which is likely due to blockage of sebaceous gland ducts by the mites, resulting in reduced sebum secretion.
Despite ongoing debate regarding the pathogenic potential of Demodex species, various skin disorders have been reported in association with Demodex infestation, and alterations in the immune system are believed to play a role in the development of its pathogenic state. Acne vulgaris, rosacea, and seborrheic dermatitis are the main dermatological conditions in which this mite is thought to play a role in causing or exacerbation. Therefore, the diagnosis of demodicosis is important for the appropriate treatment of skin disorders (3, 8). In the present study, 46.5% of Demodex-positive individuals presented with concurrent acne or pustular skin lesions. Forton and Seys, in their clinical investigation, concluded that the frequency of Demodex infestation was considerably higher among patients presenting with skin and hair lesions in dermatology clinics compared to healthy individuals (31). Similarly, Moravvej et al. reported a significantly higher prevalence of Demodex mites in patients with acne rosacea (38.6%) compared to the control group (11). In a study conducted by Mohammadhedayati et al. among women in Ardabil, the prevalence of Demodex infestation in individuals with skin lesions (44%) was markedly higher than in healthy subjects (20%), and statistical analysis confirmed a significant association between Demodex infestation and the presence of cutaneous lesions (32). Therefore, the findings of the present study are consistent with those of previous research.
In some studies, researchers have reported a reduction in the prevalence of Demodex infestation following improvements in personal hygiene practices. In the present study, a significant association was observed between the rate of Demodex infestation and factors such as frequency of face washing, use of cleansing agents, and sharing of personal hygiene items. These findings were consistent with the results of several previous studies (33, 34).
To reduce the probability of Demodex spp. reproduction, the following control methods are recommended: Washing the face twice a day with a non-soap cleanser, abstaining from oily cleansers and greasy makeup, and exfoliating the face periodically to remove dead skin cells. Human demodicosis can be provisionally controlled with topical insecticidal creams, including crotamiton 10%, permethrin 5%, as well as with systemic or topical metronidazole. In severe cases, like those with HIV infection, oral ivermectin can be advised (6). Tea tree oil has been generally applied as topical therapy for human demodicosis. However, this agent is not miticidal below a dose of 50%. This dose of tea tree oil may be irritating. The most miticidal ingredient of tea tree oil, terpinen-4-ol, is available in commercial formulations such as Cliradex®. Once or twice applications of ivermectin 1% cream are very effective in eliminating or reducing the particular sleeves in connection with Demodex-induced blepharitis (35).
The limitations of this study are: (A) Because the volunteers were selected only from those referred to the East Ahvaz Comprehensive Health Center, the results of this study in Ahvaz County may not be representative of all parts of Iran or even Ahvaz; (B) The results of this study may be affected by unobserved confounding factors that require further investigation; (C) Sampling was obtained only from face skin, and other skin areas were not investigated and compared for Demodex mite presence; (D) Another limitation of the study was that it did not include people under the age of twenty.
5.1. Conclusions
Demodex infestation can cause ophthalmological and dermatological problems. This is the first research into prevalence and the relationship between risk factors and human Demodex in Ahvaz City. In this aspect, it will be useful to conduct more studies on demodicosis. This study indicated a higher prevalence of Demodex in men and people with oily skin. The prevalence and severity of Demodex spp. infestation was also significantly higher in people with acne than in healthy people. The CTP method is a convenient and easy method for conducting epidemiological studies.