1. Background
The health of a nation’s citizenry is largely dependent on the quality of health services rendered by its hospitals. Hospitals in developing countries, including Iran, face a number of challenges. Key among these challenges is the management of patients’ medical records and the overall hospital information. Healthcare information technology (HIT) has undergone significant developments in recent years and has revolutionized the delivery of healthcare services (1). The process of collecting and accessing health information is the most influential aspect in the health sector (2). Since receiving healthcare services is very important for society and is closely related to information, information and communication technology cannot be ignored in the provision of healthcare services, especially the use of management information systems (3). Hospital information systems (HIS) is a system that provides the process of collecting, storing, processing, retrieving, and displaying the information needed by hospital users (4). The main purpose of information systems in the health sector is to plan, make decisions, control, and provide preventive and curative health services (5), and to support hospital activities at all levels to provide better services to patients (6).
In general, some studies have shown the impact of using these systems in the healthcare system. For example, studies have shown that healthcare delivery systems have significant benefits such as reducing patient waiting times, shortening treatment processes, maximizing efficiency, increasing staff skills, reducing healthcare costs, reducing mortality rates by providing accurate and timely information, managing drug side effects, providing healthcare professionals with timely and accurate access to up-to-date patient information, reducing medical errors, managing optimal services, and improving care processes (7-13). Healthcare information quality is considered a very useful source of information that helps healthcare systems become smarter and increase the quality of services provided (14). Researchers have concluded that greater investment in HIT and health information and service quality can reduce medical errors, reduce operational costs, and increase the quality of healthcare processes and services, and that full implementation of HIT can save billions of dollars, reduce medication events, and lead to better doctor-patient communication (15-17).
The McLean et al. model provides a comprehensive understanding of information system success and is widely accepted as a comprehensive model for evaluating information systems in hospitals, and includes dimensions of system quality, information quality, service quality, usability, user satisfaction, and net benefits (18). In this model, system quality is an important part of the information system tasks that focus on the interaction between the user and the information system (19). The D&M model has been extensively applied in finance, education, and business management. More recently, the model has also been used in the medical and health fields. For example, Van Der Meijden et al. summarized the success determinants of clinical information systems for inpatients based on the D&M model. Yu et al. constructed an information system success model for electronic prescribing from the perspective of doctors and pharmacists. Other scholars have used the D&M model to evaluate electronic medical record systems and computerized physician order entry systems. System quality has the characteristics of availability at any time and place, hardware and software reliability, user-friendliness, user satisfaction, and net benefits (20). Information quality has characteristics such as information accuracy, information adequacy, information freshness, and information reliability, in which system quality and information quality have an important and significant impact on user satisfaction with the information system (20).
Service quality is based on what is to be provided and what is provided, in other words, its ability to provide accurate, timely, and relevant information. Service quality indicates the extent to which an information system is successful in providing value and contributing to organizational or individual goals (19, 21, 22). Intention to use is defined as the intention of users to use the system, and net benefits are defined as the extent to which the information system contributes to the success of individuals, organizations, and groups (20).
2. Objectives
The purpose of this study is to determine the success rate of the HIS in the educational and medical centers of Abadan University of Medical Sciences based on the modified DeLone and McLean model, which will be evaluated based on three criteria of system quality, information quality, and service quality, in order to determine the degree of compliance of the studied system with the three criteria of the desired model and investigate the success rate of the HIS in health centers of Abadan University of Medical Sciences based on the DeLone and McLean model.
3. Methods
This is a cross-sectional descriptive-analytical study conducted in 2024. The research population comprised all users of the patient information system in the educational and medical centers of Abadan University of Medical Sciences, from which 200 individuals were selected through stratified random sampling across different job categories (medicine, nursing, paraclinical unit staff, health information technology, pharmacy, and administration). Data were collected through a researcher-developed questionnaire based on the modified DeLone and McLean model, in accordance with the three criteria of system quality, information quality, and service quality. At the beginning of the questionnaire, the importance of the study and the research objectives were explained to the respondents. The first part of the questionnaire gathered demographic information of the respondents, including age, gender, education, job, work experience, computer skills, and working hours with the hospital and educational and medical center information system.
1. Inclusion criteria:
- The HIS users: Only individuals actively using the HIS at health centers of Abadan University of Medical Sciences.
- Staff members: Healthcare staff (doctors, nurses, administrators) directly involved with the HIS.
- Patients with data in HIS: Only patients whose data have been entered into the HIS.
- Based on DeLone and McLean model: Studies must evaluate HIS success based on DeLone and McLean criteria.
2. Exclusion criteria:
- Incomplete data: Users or patients with missing or incomplete data in HIS.
- Non-compliance with model: Participants whose data cannot be assessed based on the DeLone and McLean model.
- Inability to access HIS: Users unable to access or use the HIS due to technical issues.
- Refusal to participate: Participants who do not consent or refuse to take part in the study.
The second part includes 21 questions, divided into system quality (7 questions), information quality (7 questions), and service quality (7 questions), which were created on a five-point Likert scale with responses ranging from very high = 5, high = 4, medium = 3, low = 2, to very low = 1. According to the responses of the samples, the success rate of the information system was determined by calculating the average of the total points obtained (1 to 5). After receiving the code of ethics and permission from the university research council, explanations were provided to the users about the study's objectives and the confidentiality of their responses and opinions. After obtaining oral and informed consent, the questionnaire was completed by them. The inclusion criterion for the study was voluntary and informed consent and working with the HIS, while the exclusion criterion was non-cooperation in the study and incomplete completion of the questionnaire.
The validity of the questionnaire was evaluated by five experts, including three health information management experts and two medical informatics experts. Test-retest reliability (with a 10-day interval) was performed to determine the reliability of the questionnaire. Ten users were asked to answer the questionnaire again after ten days, and the reliability of the questionnaire was confirmed using a correlation coefficient of 86%. To obtain the opinions of the experts, the questionnaires were provided to them through in-person visits. SPSS 26 descriptive statistics software was used to analyze the data.
4. Results
In this study, 220 questionnaires were distributed among users, and after collection, 20 questionnaires that were not completely filled were eliminated, resulting in 200 questionnaires being analyzed. The largest number of users were undergraduates and were related to the nursing field. The results of the study showed that the highest percentage of respondents based on job categories were related to the nursing group (40%), while the lowest percentage was related to pharmacy employees (3%, Table 1).
| Demographic Characteristics | No. (%) |
|---|---|
| Sex | |
| Male | 120 (60) |
| Female | 80 (40) |
| Age group (y) | |
| 30 - 39 | 40 (20) |
| 40 - 49 | 110 (55) |
| 50 - 59 | 50 (25) |
| Education | |
| Postgraduate diploma | 8 (4) |
| Bachelor's degree | 140 (70) |
| Master's degree | 10 (5) |
| PhD | 2 (1) |
| Professional doctorate | 6 (3) |
| Specialization | 30 (15) |
| Sub specialization | 4 (2) |
| Occupation | |
| Physician | 40 (20) |
| Nurses | 80 (40) |
| HIT staff | 40 (20) |
| Paraclinical staff | 14 (7) |
| Pharmacy | 6 (3) |
| Administrative staff | 20 (10) |
Abbreviation: HIT, healthcare information technology.
The results of the study in the three criteria showed that, in the system quality criterion, the highest score was related to data integrity and exchangeability (3.87), while the lowest score was related to flexibility and customization (2.84, Table 2).
| Criteria and Related Cases | Mean ± SD |
|---|---|
| System quality | |
| Adaptability to upcoming needs of users | 3.28 ± 0.69 |
| Meeting of security and privacy requirement | 3.47 ± 0.75 |
| System reliability and free from error | 3.33 ± 0.88 |
| Integrity and interchange of information | 3.87 ± 0.74 |
| Usability and user-friendly of system | 3.33 ± 0.88 |
| Flexibility and customization | 2.84 ± 0.77 |
| Speed and response time | 3.43 ± 0.79 |
| Total | 3.36 ± 0.78 |
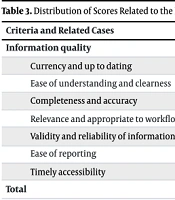
In the information quality criterion, the highest average score was related to the completeness and accuracy of information (3.33), while the lowest score was related to the ease of reporting (2.61, Table 3).
| Criteria and Related Cases | Mean ± SD |
|---|---|
| Information quality | |
| Currency and up to dating | 3.03 ± 0.69 |
| Ease of understanding and clearness | 3.27 ± 0.71 |
| Completeness and accuracy | 3.33 ± 0.88 |
| Relevance and appropriate to workflow | 2.91 ± 0.59 |
| Validity and reliability of information | 2.83 ± 0.68 |
| Ease of reporting | 2.61 ± 0.81 |
| Timely accessibility | 3.18 ± 0.73 |
| Total | 3.02 ± 0.73 |
In the service quality criterion, the highest score was related to reducing medical errors through reminders and alarms (3.47), while the lowest score was related to the system guide (2.14, Table 4).
| Criteria and Related Cases | Mean ± SD |
| Services quality | |
| Hardware and software proportion | 2.81 ± 0.81 |
| Improvement of workflow | 3.28 ± 0.77 |
| Information backup | 3.23 ± 0.79 |
| Reduce of errors through reminders and alerts | 3.47 ± 0.75 |
| System manual | 2.14 ± 0.66 |
| Support and maintenance | 2.88 ± 0.63 |
| Increase satisfaction and quality of healthcare | 3.15 ± 0.68 |
| Total | 2.99 ± 0.72 |
The results of the study showed that, based on the three criteria, the highest success rate of the HIS was related to system quality (3.36), while the lowest average was related to service quality (2.99). The overall success rate of the HIS in the educational and medical centers of Abadan University of Medical Sciences, based on the three criteria of system quality, information quality, and service quality of the DeLone and McLean model, was 3.12 (Table 5).
| Quality Dimensions | Mean ± SD | Total Mean ± SD |
|---|---|---|
| System quality | 3.36 ± 0.78 | 3.12 ± 0.74 |
| Information quality | 3.02 ± 0.73 | |
| Service quality | 2.99 ± 0.72 |
A one-sided sample test was used to determine whether the success rate of the information system was desirable in each of the criteria of system quality, information quality, and service quality. If at least 75% or a score of 3.75 out of 5 was achieved in each item, the situation was considered desirable; if a lower score was achieved, it was considered undesirable. Given P = 0.000 at an error level of α = 0.05, this assumption (H:μ > 3.75) was rejected. This means that none of the three criteria — system quality, information quality, and service quality — were at a desirable level.
5. Discussion
According to the studies conducted, the system quality dimension was the most important, with the dimensions of information quality and service quality following in rank. The results of the Zaied study in South African hospitals showed that information quality, system quality, and service quality were all at a desirable level (23), which was not in line with the findings of the present study. According to the results of the present study, there is a significant relationship between the two variables of information system quality and users' willingness to use the information system. This finding is consistent with the results of some previous studies (24-26). However, this finding is not consistent with some other studies (27-29). This indicates that to encourage organizations to continuously use the implemented information systems, the quality of the system in terms of ease of use, flexibility, and performance should receive the utmost attention.
In a study conducted by Alsalman et al. in Saudi Arabia in 2021, entitled "Surveying the Implementation of Hospital Information Systems in the Western Provinces", the results indicated that the implementation of the HIS had favorable conditions in terms of information quality, especially for functions related to electronic clinical documents and viewing the results of paraclinical and medical procedures (30). The study findings showed that in terms of overall satisfaction, users were relatively satisfied (3.12). The highest level of satisfaction (3.36) was in the system quality dimension, while the highest level of satisfaction in the information quality dimension was (3.02), and the lowest level of satisfaction (2.99) was in the service quality dimension of the system.
In the study by Hashemi Hassani et al., conducted in a cross-sectional descriptive manner to investigate users' views on factors affecting the data quality of the Iranian Electronic Health Record System (SEPAS) in hospitals under the jurisdiction of Mashhad University of Medical Sciences, the findings showed that the most important individual factor was user training in the field of data quality. The most important organizational factor was the integration and connection of the HIS with the civil registry, and among the technical factors, the quality of response of the support team received the highest score (31).
In a study conducted by Kabir et al. in 2022, entitled "User Satisfaction with the Quality of Health Information Software in Golestan Province", the findings indicated that the highest level of satisfaction was in the quality of support services, and the lowest level of satisfaction was in the overall satisfaction with the system. This level of satisfaction with the lean system in all dimensions was significantly related to gender, level of education, and levels of the health network (32).
Local and indigenous laws have a great impact on the design and evaluation of information systems, especially in the health sector. Therefore, it can be seen that software produced in one part of the world is used universally in other parts, but this is not the case with health information systems, where the culture of the community and local laws are effective in the design (33). The lack of feasibility studies and the lack of participation of end users in the design of systems is also one of the problems that exist in HIS, causing dissatisfaction and reluctance to use the systems in some cases. Therefore, by re-evaluating HIS, problems can be identified and used in redesigning the systems (34). Users of information systems will be satisfied when the designed system aligns with the requirements, expectations, and goals set (35). If the three criteria of system quality, information quality, and service quality are not considered in the design of systems, the information system will not be responsive to users and will gradually cause them to become disengaged and unmotivated, ultimately decreasing their technological literacy (36).
5.1. Conclusions
According to the results of this study, the HIS at Abadan University of Medical Sciences has been able to meet the satisfaction and expectations of users at an average level, which will ultimately lead to continued use. Therefore, information quality, system quality, service quality, user satisfaction with the system, and intention to use the system have impacted the success of the HIS, improving hospital performance. By properly applying these criteria in the HIS, the decision-making process will be better, ensuring the satisfaction of providers and recipients of hospital services, improving productivity, and ultimately net profit.
5.2. Limitations
One of the limitations of this study is the failure of hospital staff to complete some questionnaires and potential bias in self-reported data from healthcare center staff, as well as the impact of technical and infrastructure issues of HIS on the study results.