1. Background
Tuberculosis (TB) remains one of the world’s most formidable public health challenges. According to the World Health Organization (WHO), an estimated 10.6 million people developed TB in 2021, resulting in 1.6 million deaths — making it the leading cause of mortality from a single infectious agent (1). Despite remarkable progress in diagnostics and therapeutics, TB continues to exert a disproportionate burden in low- and middle-income countries (LMICs), where limited infrastructure, delayed case detection, and constrained access to advanced technologies sustain high transmission and mortality rates (2, 3). Pakistan ranks among the top five high-burden countries, with an estimated incidence of 265 cases per 100,000 population annually (4). Persistent challenges such as underreporting, poverty, and rising multidrug-resistant tuberculosis (MDR-TB) further complicate national control efforts (5). These factors underscore the pressing need for rapid, accurate, and accessible diagnostic strategies to ensure early detection and effective management.
A variety of diagnostic modalities are currently employed for TB detection, each with distinct advantages and limitations. Sputum smear microscopy remains a simple and inexpensive frontline tool, yet its sensitivity is low in patients with minimal bacterial loads or extrapulmonary disease (6). Culture techniques, though recognized as the diagnostic gold standard, are time-consuming and require biosafety facilities that are rarely available in resource-limited environments (7). Molecular assays such as GeneXpert MTB/RIF have substantially improved diagnostic accuracy and resistance profiling but remain dependent on costly reagents, uninterrupted power supply, and trained personnel (8).
Imaging constitutes a cornerstone of TB detection and disease monitoring. Chest X-ray (CXR) is widely used in both clinical and public health programs owing to its affordability and portability. However, its diagnostic value is hampered by poor specificity, since radiographic findings — such as patchy infiltrates, nodular opacities, or cavities — may mimic other pulmonary conditions (9). High-resolution computed tomography (HRCT) offers substantially higher spatial resolution and contrast differentiation, enabling visualization of early parenchymal lesions, tree-in-bud patterns, and small cavities that often escape CXR detection (10). From a physical perspective, HRCT acquires thin-slice volumetric data with high-frequency reconstruction algorithms, whereas conventional radiography compresses three-dimensional structures into a single two-dimensional projection — accounting for HRCT’s superior lesion delineation. Recent comparative studies also emphasize that HRCT more accurately characterizes lung damage severity between drug-sensitive and drug-resistant TB cases and supports improved clinical decision-making through enhanced lesion quantification.
Beyond imaging, immunological assays such as the interferon-gamma release assays (IGRAs) — including QuantiFERON-TB Gold and T-SPOT.TB — measure T-cell reactivity to Mycobacterium TB-specific antigens, providing valuable information for latent TB infection detection (11). However, their inability to distinguish latent from active disease, coupled with variable sensitivity in immunocompromised patients, limits their use as stand-alone diagnostics (12). Serological tests, though explored in some contexts, have yielded inconsistent and often suboptimal performance (13).
Given the complexity of TB pathogenesis and the diverse diagnostic landscape, a multimodal approach that integrates imaging, molecular, and immunological data is increasingly advocated to improve detection accuracy in high-burden regions (14). The HRCT, in particular, has gained prominence for its capacity to detect subtle pulmonary changes correlating with immunological test results and early bacteriological conversion. Moreover, contemporary advances, including hybrid deep-learning models for chest imaging, reinforce the value of high-resolution modalities in achieving earlier and more precise detection.
2. Objectives
Accordingly, the present study aims to comprehensively evaluate the diagnostic performance of HRCT, CXR, and immunological assays (QuantiFERON-TB Gold and T-SPOT.TB), emphasizing sensitivity, specificity, predictive values, and inter-method agreement. By comparing these modalities within a high-burden population, this study provides robust evidence of each tool’s diagnostic contribution and clarifies the potential of HRCT to enhance early case finding, guide clinical management, and strengthen national TB surveillance frameworks.
3. Methods
3.1. Study Design and Setting
This retrospective, observational study was conducted at the Islamabad Diagnostic Center, Pakistan, between January 2021 and December 2023. Patient records were reviewed to compare the diagnostic performance of immunological and radiological modalities used for TB detection. The study specifically evaluated whether HRCT or CXR provided additional diagnostic value among individuals with positive interferon-gamma release assay (IGRA) results but normal CXR findings. The study protocol was approved by the institutional ethics review board, and patient confidentiality was strictly maintained.
3.2. Study Population and Inclusion Criteria
Medical records of patients aged > 18 years who underwent TB serology, IGRA testing (QuantiFERON-TB Gold or T-SPOT.TB), and radiological assessment (CXR ± HRCT) within the same diagnostic episode were included. Patients with incomplete records, prior anti-TB therapy, or concurrent pulmonary infections (e.g., bacterial pneumonia, COVID-19) were excluded.
3.3. Diagnostic Modalities
3.3.1. Immunological and Serological Tests
The QuantiFERON-TB Gold (Qiagen, Germany) and T-SPOT.TB IGRA (Oxford Immunotec, UK) assays were performed according to manufacturer instructions. Both tests measure interferon-γ release following stimulation of peripheral blood lymphocytes with Mycobacterium TB-specific antigens (ESAT-6 and CFP-10). Results were interpreted as positive, negative, or indeterminate per established cut-off values. Serological testing for TB antibodies was carried out using the TB IgG/IgM ELISA kit (manufacturer, country). All test results were retrieved from the hospital laboratory information system.
3.3.2. Imaging Techniques
- Chest X-ray: Chest radiographs were obtained using a digital radiography system (Siemens Ysio Max, Siemens Healthineers, Germany) in the postero-anterior projection with standard exposure parameters (100 - 120 kVp, 3 - 5 mAs, 180 cm focal distance).
Underlying physics: Conventional radiography generates images by passing a broad X-ray beam through the thorax, where tissues of varying densities attenuate photons to different degrees. The resulting two-dimensional projection represents the cumulative absorption pattern recorded on a flat detector. This superimposition of anatomical structures limits visualization of small lesions or early parenchymal changes.
- High-resolution computed tomography: All HRCT scans were performed using a 128-slice multi-detector CT scanner (GE Revolution Evo, GE Healthcare, USA) without intravenous contrast. Scanning parameters included 120 kVp, 100 - 150 mAs, 1.25 mm collimation, 0.625 mm reconstruction interval, and a matrix of 512 × 512. Images were reconstructed using a high-spatial-frequency (bone) algorithm for lung parenchyma evaluation.
Underlying physics: The HRCT acquires multiple thin-slice axial images by rotating an X-ray tube and detector array around the patient, measuring differential attenuation of X-rays in cross-sectional planes. The resulting volumetric dataset undergoes filtered back-projection or iterative reconstruction, yielding isotropic voxels that enable fine delineation of pulmonary microarchitecture, including bronchioles and interstitial structures, with much greater spatial resolution than conventional CXR.
3.3.3. Image Interpretation
All CXR and HRCT images were independently reviewed by two consultant radiologists (each with more than 10 years of thoracic imaging experience) blinded to clinical and laboratory data. Discrepancies were resolved by consensus. Radiological findings were categorized as follows:
- Active TB: Presence of cavitation, centrilobular nodules, tree-in-bud pattern, consolidation, or miliary nodules
- Healed/inactive TB: Fibrotic scarring, calcified nodules, or pleural thickening
- Normal/non-specific: No parenchymal abnormalities
3.4. Data Analysis and Concordance Evaluation
The diagnostic performance of HRCT, CXR, IGRA, and serology was assessed using standard statistical metrics: Sensitivity, specificity, positive predictive value (PPV), and negative predictive value (NPV). Concordance between imaging findings and IGRA results was calculated using Cohen’s κ coefficient. Continuous variables were expressed as mean ± standard deviation (SD), and categorical variables as frequencies and percentages. Statistical analyses were performed using SPSS version 25.0 (IBM Corp., USA), with P < 0.05 considered statistically significant.
3.5. Ethical Considerations
This study adhered to the principles of the Declaration of Helsinki. Institutional ethical approval was obtained under reference No. IDCERC20250613. As the analysis was retrospective and de-identified, the requirement for informed consent was waived.
4. Results
The study cohort was analyzed to compare TB detection across HRCT, CXR, and immunological assays (QuantiFERON-TB Gold and T-SPOT.TB).
4.1. Demographic Characteristics
Demographic analysis revealed that HRCT tended to detect TB-positive individuals who were older than those identified by CXR. The mean age of HRCT-positive cases was 44.9 years (median 45; range 6 - 77), compared with 36.1 years (median 34; range 1 - 90) among CXR-positive cases. This age difference was statistically significant (independent t-test, P < 0.05), suggesting that HRCT offers enhanced sensitivity in older populations, likely due to its ability to visualize subtle parenchymal and fibrotic changes not evident on plain radiography. Gender distribution was similar across modalities: HRCT detected 52.4% males and 47.6% females, whereas CXR detected 62.8% males and 37.2% females; these differences were not statistically significant (χ2 test, P > 0.05).
4.2. Performance of Serological and Immunological Tests
Among all diagnostic modalities, serology demonstrated 42.3% positivity. However, only 33.7% of serology-positive individuals showed radiographic abnormalities on CXR, while 50.2% exhibited HRCT-detectable lesions. Therefore, HRCT identified additional pathology in nearly one-fifth of serology-positive patients who appeared normal on X-ray.
The T-SPOT.TB IGRA yielded the highest positivity rate (48.1%) among immunological assays. Of these, 41.6% showed abnormalities on CXR, whereas 58.3% demonstrated HRCT-confirmed lesions. Similarly, QuantiFERON-TB Gold detected infection in 46.7% of patients, with 39.2% showing CXR findings and 56.9% showing HRCT findings. These results consistently indicated that HRCT detected a larger burden of TB-related abnormalities than CXR across all immunological subgroups.
Agreement analysis supported this trend: Concordance between HRCT and IGRA results was moderate (κ = 0.53), while that between CXR and IGRA was lower (κ = 0.39). Hence, HRCT findings aligned more closely with immune-based assays, demonstrating stronger diagnostic complementarity.
4.3. Comparative Diagnostic Accuracy
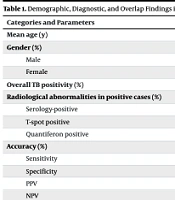
A comparative analysis of the three principal modalities revealed distinctive performance profiles. The HRCT showed a detection rate of 44.4%, sensitivity of 80%, and specificity of 85%, with a PPV of 78% and NPV of 86%. These results indicate reliable exclusion of TB in HRCT-negative patients and minimal false negatives. The CXR achieved a higher crude detection rate of 55.6%, with sensitivity of 85% and specificity of 80%. However, its PPV (82%) and NPV (83%) suggested a greater tendency for false positives relative to HRCT. The IGRA assays (combined QuantiFERON and T-SPOT) exhibited a detection rate of 44.4%, sensitivity of 75%, specificity of 78%, PPV of 70%, and NPV of 80%, highlighting their limited diagnostic precision when used independently (Table 1).
| Categories and Parameters | HRCT | X-ray | IGRA (T-Spot/Quantiferon) |
|---|---|---|---|
| Mean age (y) | 44.9 (6 - 77) | 36.1 (1 - 90) | - |
| Gender (%) | |||
| Male | 52.4 | 62.8 | - |
| Female | 47.6 | 37.2 | - |
| Overall TB positivity (%) | 44.4 | 55.6 | 44.4 (48.1/46.7) |
| Radiological abnormalities in positive cases (%) | |||
| Serology-positive | 50.2 | 33.7 | - |
| T-spot positive | 58.3 | 41.6 | 48.1 |
| Quantiferon positive | 56.9 | 39.2 | 46.7 |
| Accuracy (%) | |||
| Sensitivity | 80 | 85 | 75 |
| Specificity | 85 | 80 | 78 |
| PPV | 78 | 82 | 70 |
| NPV | 86 | 83 | 80 |
| κ | 0.53 (moderate) | 0.39 (weak) | - |
| Detection overlap (%) | |||
| Detected by all three | 27.8 | 27.8 | 27.8 |
| Detected by method alone | 16.7 | 13.9 | 0 |
| Dual overlap with HRCT | - | 27.8 | 44.4 |
| Dual overlap with X-ray | 27.8 | - | 27.8 |
Abbreviations: HRCT, high-resolution computed tomography; IGRA, interferon-gamma release assay; TB, tuberculosis; PPV, positive predictive value; NPV, negative predictive value; κ, kappa.
4.4. Overlap and Concordance of Diagnostic Modalities
Analysis of detection overlap provided further insights into modality complementarity. Among all TB-positive individuals, 27.8% were identified concurrently by HRCT, CXR, and IGRA. HRCT alone uniquely identified 16.7% of TB cases that would otherwise have been missed, while CXR alone detected 13.9%. Interestingly, IGRA alone did not identify any TB-positive case without radiological abnormalities, reinforcing the necessity of imaging confirmation for immunological results.
Dual-modality overlap was most pronounced between HRCT and IGRA (44.4%), demonstrating their synergistic diagnostic potential. Overlaps between HRCT and CXR and CXR and IGRA were equal at 27.8% each. Notably, among IGRA-positive but radiographically normal cases, HRCT also failed to detect abnormalities, indicating limited incremental value in this subgroup. Thus, HRCT’s diagnostic advantage appears strongest in patients with existing radiological suspicion rather than in immunologically positive but radiologically silent presentations.
Collectively, these findings highlight HRCT’s superior ability to identify subtle and age-related pulmonary lesions, its higher specificity, and stronger agreement with IGRA results. While HRCT enhances diagnostic certainty and aids early case detection, its marginal benefit in IGRA-positive yet X-ray-normal individuals suggests selective application for optimal cost-effectiveness. Therefore, HRCT stands out as a powerful adjunct to CXR and immunological assays, offering a refined and evidence-based approach for strengthening TB surveillance and diagnostic precision in high-burden settings.
5. Discussion
This study provides critical insights into the comparative diagnostic efficiencies of HRCT, CXR, and IGRAs in TB detection. The findings reaffirm the central role of CXR as an effective and accessible primary screening tool, detecting the highest number of TB cases, consistent with previous global studies emphasizing its practicality in large-scale surveillance programs (8, 9). However, HRCT demonstrated added diagnostic value in patients with inconclusive or subtle radiographic findings, showing higher sensitivity in detecting parenchymal abnormalities such as nodules, cavitations, and peribronchial thickening that may be overlooked on conventional radiography. These results are in agreement with recent comparative imaging studies, which report that HRCT provides superior lesion characterization and improved detection of both drug-sensitive and drug-resistant TB forms (15).
Although IGRA results correlated moderately with imaging findings, they lacked sufficient diagnostic power as standalone tests. The combined use of HRCT and IGRA significantly improved diagnostic accuracy, supporting the concept of multimodal integration in TB diagnosis. Similar conclusions have been reported by Aziz et al. (16), who showed that advanced imaging models — including hybrid deep-learning approaches applied to CXR — enhanced TB detection precision, underscoring the importance of imaging-based confirmation alongside immunological testing. The present study further establishes that while HRCT and IGRA complement each other diagnostically, imaging remains indispensable for confirming disease activity and extent.
In the present cohort, HRCT demonstrated higher sensitivity than CXR in detecting subtle pulmonary involvement and fibrotic lesions, particularly among older patients. The mean age of HRCT-positive individuals (44.9 years) was significantly higher than that of CXR-positive cases (36.1 years), implying that age-related parenchymal changes and fibrotic remodeling may be better visualized with HRCT. Similar findings have been reported in South African and Indian studies, where elderly TB patients exhibited more fibrotic and fewer cavitary lesions — patterns often missed by plain radiography (10-14, 17). These observations suggest that HRCT is particularly valuable for differentiating reactivation or chronic disease patterns in older populations, whereas CXR remains adequate for younger patients presenting with acute, cavitary lesions.
Gender distribution in this study did not significantly differ across modalities, though a higher proportion of males (62.8%) were diagnosed via CXR. This pattern reflects known epidemiological trends in TB, where male predominance is attributed to greater occupational exposure, smoking prevalence, and healthcare-seeking disparities, as observed in Bangladesh, Indonesia, and other endemic regions (6, 7). These demographic insights reinforce the importance of considering both biological and social determinants in TB control strategies.
The overlap analysis revealed that only 27.8% of TB-positive cases were detected concurrently by HRCT, CXR, and IGRA, indicating that each modality captures distinct diagnostic dimensions. The highest dual concordance (44.4%) was observed between HRCT and IGRA, highlighting their synergistic diagnostic potential when applied together. However, HRCT failed to provide additional diagnostic benefit in IGRA-positive but radiographically normal individuals, suggesting that its use should be reserved for cases with clinical suspicion or equivocal CXR findings. This aligns with evidence from multiple high-burden regions showing that HRCT’s incremental yield is greatest in patients with non-specific radiographic abnormalities or discordant laboratory results (18, 19).
In resource-limited settings, cost and accessibility remain critical determinants of diagnostic selection. The CXR, with its affordability and high detection rate (55.6% in this study), continues to serve as the cornerstone of TB screening. Nonetheless, CXR lacks specificity, as its features can overlap with other pulmonary diseases such as pneumonia, chronic obstructive pulmonary disease (COPD), and interstitial lung disease. The HRCT, by contrast, offers higher specificity and structural detail, allowing confident differentiation of active TB from other lung pathologies, an advantage also noted in studies examining antimicrobial resistance patterns and their radiologic manifestations.
The moderate concordance between imaging and IGRA findings (κ = 0.53 for HRCT and κ = 0.39 for CXR) underscores that while immunological assays can support diagnostic decision-making, they cannot replace imaging. The T-SPOT.TB IGRA showed the highest positivity rate (48.1%) and strongest correlation with radiological evidence, consistent with prior studies from China and Japan reporting similar sensitivities (around 80 - 85%) but limited specificity for active TB. These results collectively support the selective use of IGRA as a complementary test to confirm infection in clinically suspected or radiologically positive cases, rather than as a screening tool in asymptomatic populations.
The current findings parallel global research trends emphasizing tiered diagnostic algorithms, starting with CXR for screening, followed by HRCT for inconclusive cases, and IGRA for immunological confirmation. This approach balances diagnostic accuracy with cost-effectiveness, particularly in high-burden countries such as Pakistan, India, and Ethiopia, where resource constraints necessitate rational test utilization (17). Moreover, the integration of artificial intelligence (AI)-based image analysis offers a promising avenue for improving diagnostic throughput, minimizing observer variability, and extending access to expert-level interpretation in remote areas (16).
The study highlights the importance of a multimodal diagnostic framework in TB detection. The CXR should remain the first-line screening method due to its widespread availability, while HRCT should be employed selectively for patients with inconclusive findings or suspected extrapulmonary involvement. The IGRA testing, though valuable, should be interpreted in conjunction with radiological and clinical data. Future research should focus on developing cost-effectiveness models to evaluate HRCT deployment in different healthcare settings and explore the use of AI-enhanced image analysis to improve detection sensitivity without escalating costs. Additionally, longitudinal studies are warranted to assess the prognostic implications of HRCT findings in predicting treatment response and relapse in high-burden populations.
5.1. Conclusions
This study underscores the critical importance of combining radiological and immunological approaches for accurate TB detection. Chest X-ray remains the most practical and cost-effective primary screening tool, particularly suitable for large-scale public health programs. The HRCT serves as a valuable confirmatory modality in cases with inconclusive or atypical radiographic findings, offering superior visualization of subtle parenchymal changes. Among immunological tests, the T-SPOT.TB IGRA enhances diagnostic confidence but lacks sufficient specificity to function as a standalone diagnostic method. Together, these findings support a multimodal diagnostic strategy that leverages the complementary strengths of imaging and immunological assays. Future research should focus on developing integrated diagnostic algorithms that combine these modalities, potentially augmented by AI and cost-effectiveness analyses, to improve early detection, clinical decision-making, and patient outcomes in TB-endemic regions.