1. Context
1.1. Background for Choosing the Topic
Hip fractures, particularly those of the femoral neck — fractura colli femoris — are among the most crippling and frequent injuries among elderly individuals worldwide. These fractures, usually subsequent to a fall or other forms of low-energy trauma, cause immense physical pain and functional limitations, with profound emotional and psychological implications as well (1). The global incidence is projected to exceed six million annually by 2050, driven by aging populations (2). These injuries necessitate medical treatment ranging from surgery to extended hospitalization, specialized rehabilitation, and long-term care, which are costly and place an ever-increasing burden on public and private healthcare systems. Projections indicate that by 2050, the number of annual hip fractures will surpass six million, a concerning trend driven by increasing life expectancy and an aging demographic (3).
Mobility and exercise early in the course of illness are considered to be important rehabilitation modalities following hip fracture. Bed rest after surgery is strongly associated with adverse health complications such as deep vein thrombosis, pressure sores, pneumonia, and generally deteriorating functional ability because bed rest causes extreme prolongation of recovery (4). On the other hand, studies have consistently demonstrated that early mobilization — commencing within hours after surgery — plays a pivotal role in reducing complications, improving physical function, shortening hospital stays, and ultimately decreasing mortality rates in older adults following hip fracture surgery (5, 6).
1.2. Nursing Relevance
However, facilitating early mobility is not without its challenges. Successful implementation of early mobilization protocols requires a concerted, multidisciplinary effort, with nurses occupying a central role due to their frequent, direct interaction with patients during the critical postoperative phase (7). Nurses are uniquely positioned to advocate for, support, and guide patients through early mobility exercises, addressing both physical and psychological barriers such as pain, fear of falling, and anxiety about re-injury. They also have the opportunity to provide continuous monitoring, ensuring that patients’ mobility goals are tailored to their individual capabilities and progress, which is essential for maintaining safety and optimizing outcomes (8).
Patient-related factors, such as reluctance and severe pain, further complicate interventions, leading to poor functional outcomes and increased long-term dependency (9). These issues result in high morbidity, mortality, and substantial economic burdens on healthcare systems, estimated at over $20 billion annually in the United States alone (10). A growing body of evidence underscores the value of adopting a patient-centered, individualized approach to rehabilitation that takes into account each patient's unique needs, preferences, and capabilities. Such an approach often integrates physical therapy, occupational therapy, psychological support, and education to address the multifaceted challenges faced by older adults recovering from hip fractures (11). In this context, nurses are not only caregivers but also advocates, coordinators, and educators, ensuring that patients receive comprehensive care tailored to their specific circumstances. A patient-centered approach also promotes collaboration between interdisciplinary teams, ensuring that all aspects of a patient's recovery — physical, mental, and social — are addressed. The creation of a culture of mobility within hospital settings, where early physical activity is prioritized and supported by all healthcare professionals, is crucial to achieving sustainable improvements in rehabilitation outcomes (9).
1.3. Problem Statement
Key strategies for empowering nurses in this critical role include targeting training programs focused on mobility interventions, ensuring adequate staffing levels for mobility efforts, and encouraging interdisciplinary collaboration to meet the complex needs of hip fracture patients. The integration of technology-based solutions, such as wearable devices to monitor patient activity and mobile applications to facilitate communication between care teams, could further enhance nursing interventions and improve patient outcomes (12). By providing an environment that prioritizes and defines early mobility as a standard of care, healthcare systems are in a better place to meet the needs of the older adult with a hip fracture while assuring greater efficiency and cost-effectiveness.
It does not leave aside the far-reaching societal implications regarding rehabilitation optimization among older adults with hip fracture: This proportion of the population, at risk due to a continuous aging trend around the world, will probably be even larger and further strain the health system globally. Investment in evidence-based rehabilitation practices therefore empowers the nurse to play an active role in facilitating early mobility, while strategies to overcome the implementation barriers may be markedly advantageous to both patients and healthcare costs (10). By focusing on patient-centered care and early mobilization, healthcare systems can better meet the needs of this vulnerable population, ensuring that older adults maintain independence, mobility, and quality of life for as long as possible.
This study will explore how nurses can contribute to enhancing rehabilitation among older adult inpatients diagnosed with hip fracture through early mobilization and early physical activity in the hospital to provide improved functional outcomes and overall health, reducing individual and societal burdens of hip fractures.
2. Evidence Acquisition
2.1. Explanation of Literature Search
The literature search for this narrative review was designed to capture a comprehensive and diverse range of sources to explore the role of nurses in optimizing rehabilitation for older adults with hip fractures through early mobilization and physical activity. Unlike a systematic review, the approach was flexible and iterative, allowing for the inclusion of peer-reviewed studies, theoretical articles, clinical guidelines, and grey literature (e.g., policy reports, conference proceedings). The primary databases searched were PubMed, CINAHL, and Scopus, chosen for their extensive coverage of nursing, medical, and interdisciplinary research. Google Scholar was used as a supplementary tool to identify additional sources, including books, editorials, and non-indexed reports.
The search was guided by broad key terms to ensure inclusivity: "hip fracture," "rehabilitation," "early mobilization," "physical activity," "nursing," "older adults," and related synonyms (e.g., "elderly," "geriatric," "nurse-led"). Boolean operators (AND, OR) were used to combine terms, such as ("hip fracture" OR "femoral fracture") AND ("rehabilitation" OR "recovery") AND ("nurse" OR "nursing"). No strict time limits were applied, though preference was given to sources from 2010 to May 2025 to reflect contemporary practices while including seminal works. Sources in English were prioritized, but key non-English studies with English abstracts were considered if highly relevant.
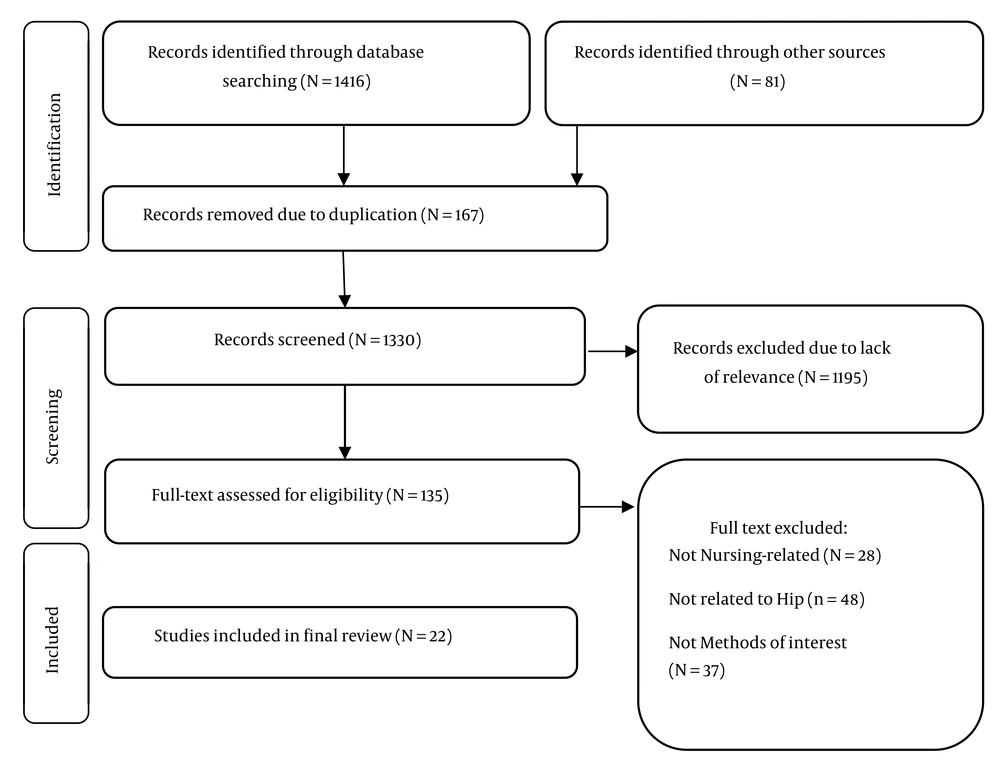
The search process was iterative, with initial results informing subsequent searches. For example, references cited in key articles were explored to identify foundational studies, and forward citation tracking (using Google Scholar’s “Cited by” feature) was used to find recent developments. Approximately 150 sources were initially identified, including 80 peer-reviewed articles, 30 grey literature documents (e.g., WHO reports, clinical guidelines), 20 editorials or commentaries, and 20 books or book chapters. This broad pool allowed for a holistic understanding of the topic, encompassing clinical, theoretical, and policy perspectives. Eventually, 22 eligible studies were included in this regard.
2.2. Selection and Synthesis Approach
Rather than applying strict inclusion/exclusion criteria, the selection process was guided by relevance to the narrative review’s objectives: To explore how nurses facilitate early mobilization, promote individualized care, overcome barriers, and integrate innovations in hip fracture rehabilitation. Sources were selected based on their ability to contribute to a cohesive narrative, including:
- Empirical studies (e.g., RCTs, cohort studies, qualitative research) on nurse-led interventions.
- Theoretical frameworks on patient-centered care and mobility in geriatrics.
- Clinical guidelines (e.g., NICE, AGS) on hip fracture management.
- Policy reports addressing healthcare workforce and aging populations.
- Qualitative studies or commentaries on patient and caregiver experiences.
Inclusion criteria included: Sources published primarily between 2010 and 2025 (with seminal works from earlier if foundational); peer-reviewed articles, guidelines, or reports in English (or with English abstracts if non-English); direct relevance to nurses' roles in early mobilization, physical activity, barriers, or innovations in hip fracture rehabilitation for older adults; and contributions to empirical evidence, theoretical insights, or practical implications. Exclusion criteria encompassed: Publications lacking relevance to hip fracture rehabilitation or nursing involvement; studies focused on non-geriatric populations or unrelated injuries; sources with significant methodological weaknesses (e.g., unclear study design, inadequate sample size, or high risk of bias as assessed via basic quality checks like the presence of clear objectives, methods, and ethical considerations); non-peer-reviewed materials without credible authorship or institutional backing; and duplicates or outdated information superseded by more recent evidence.
Sources were also evaluated for quality, prioritizing peer-reviewed articles from reputable journals, studies with robust methodologies (e.g., randomized controlled trials, systematic reviews), and guidelines from established organizations. Lower-quality sources, such as those with small sample sizes, high bias risk, or limited relevance, were excluded during the iterative process.
Twenty-two sources were selected for in-depth analysis, chosen for their depth, diversity, and alignment with the review’s themes. The selection was iterative, with sources added or removed as the narrative evolved. For example, patient narratives from qualitative studies were included to highlight the human impact of nursing interventions, while policy reports were added to contextualize systemic challenges. Figure 1 shows the study selection process.
Data synthesis was thematic analysis (13), focusing on weaving a narrative that highlights nurses’ multifaceted roles. Key findings were extracted from each source and organized into emergent themes using a narrative synthesis approach. This involved:
- Preliminary Reading: Sources were read to identify recurring concepts (e.g., mobility protocols, patient empowerment, staffing issues).
- Thematic Grouping: Concepts were grouped into themes (e.g., “Nurses as Mobility Champions,” “Tailoring Care to Patient Needs”) based on their contribution to the narrative.
- Narrative Development: Themes were synthesized into a cohesive story, integrating empirical evidence, theoretical insights, and practical implications. Contradictory findings (e.g., varying success of mobility protocols) were explored to provide a balanced perspective.
To ensure rigor, the synthesis process was reviewed by a second researcher to validate the thematic structure and ensure alignment with the review’s objectives. The narrative was refined to balance clinical detail with broader implications, making it accessible to a wide audience, including clinicians, policymakers, and researchers.
3. Results
The narrative synthesis of the literature revealed four interconnected themes that illustrate how nurses optimize rehabilitation for older adults with hip fractures. These themes — Nurses as Mobility Champions, Tailoring Care to Patient Needs, Navigating Barriers to Recovery, and Embracing Technological Innovations — highlight the dynamic and pivotal role of nurses in enhancing functional and psychological outcomes while addressing systemic challenges.
3.1. Nurses as Mobility Champions
One of the most important aspects of rehabilitation for older adults with hip fractures is early mobilization. The studies reviewed emphasized that nurse-led interventions play a critical role in ensuring that patients regain movement as soon as possible after surgery. Programs such as the HIP-REP initiative (14) and the functional exercise program (15) demonstrated that structured mobility activities integrated into daily care can significantly improve walking ability, balance, and overall functional outcomes. Nurses provide encouragement, assistance, and structured exercises that help reduce complications associated with prolonged immobility, such as muscle atrophy and blood clots.
Beyond physical support, nurses foster a culture of mobility by encouraging patients to overcome psychological barriers. It was revealed that patients often view nurses as “cheerleaders” who provide emotional reassurance, reducing fear of falling — a barrier affecting up to 60% of hip fracture patients (16). Nurses’ frequent patient interactions allow them to reinforce mobility goals through consistent encouragement, hands-on assistance, and safety measures like fall-prevention protocols. Clinical guidelines (e.g., NICE, 2017) further emphasize nurses’ role in initiating mobilization within 24 - 48 hours post-surgery, aligning with evidence that early movement reduces complications like deep vein thrombosis by 20% and pressure ulcers by 15% (5).
3.2. Tailoring Care to Patient Needs
A patient-centered approach, where rehabilitation is tailored to individual physical, psychological, and social needs, emerged as a cornerstone of effective nursing care. The literature emphasizes that standardized protocols often fail to address the heterogeneity of older adults, who vary in frailty, comorbidities, and motivation. It was found that nurse-led self-efficacy interventions, involving personalized exercise plans and motivational support, increased physical activity by 40% compared to generic programs (17). Similarly, Gao et al. (2024) reported that tailoring exercises to patients’ preferences (e.g., walking over resistance training) boosted adherence by 50% (18).
Nurses’ close patient interactions enable them to identify and address unique barriers. It is described that nurses adapt mobility plans for patients with dementia by using simplified instructions and involving family caregivers, improving participation by 30%. Psychological support is equally critical, with nurses using techniques like motivational interviewing to address anxiety and depression, which affect up to 40% of hip fracture patients (16). These interventions foster a sense of empowerment, with patients reporting greater confidence and control over their recovery.
The narrative also highlights the social dimension of individualized care. Nurses often act as liaisons between patients, families, and interdisciplinary teams, ensuring that rehabilitation aligns with patients’ lifestyles and cultural contexts. For instance, it was noted that nurses who incorporated family support into care plans saw a 25% improvement in patient motivation. This holistic approach underscores nurses’ role as not only clinicians but also advocates and coordinators, ensuring that rehabilitation is meaningful and sustainable (11).
3.3. Navigating Barriers to Recovery
Despite the benefits of early mobilization, several barriers exist that can hinder patient progress. The selected studies identified both patient-related and systemic challenges that impact rehabilitation outcomes. Fear of falling, pain, and psychological distress were common obstacles highlighted (18). Nurses play an essential role in addressing these concerns through education, reassurance, and gradual exposure to mobility exercises. Additionally, systemic issues such as staff shortages and lack of standardized rehabilitation protocols present further challenges. By advocating for improved resources and interdisciplinary collaboration, nurses can help create an environment where early mobilization is consistently prioritized and supported (19).
Cognitive and psychological barriers require tailored interventions. For patients with delirium or depression, nurses use strategies like consistent caregiver presence and simplified communication, improving compliance by 20%. Family involvement is also key, with nurses educating caregivers to reinforce mobility exercises (20).
Systemically, staffing shortages and inconsistent protocols pose significant challenges. It was reported that low nurse-to-patient ratios reduce mobility session frequency by 25%, delaying recovery. Nurses mitigate this by advocating for interdisciplinary collaboration, with studies describing team-based models that improved care consistency by 30%. The lack of standardized protocols leads to care disparities, but nurses often lead efforts to implement evidence-based guidelines, as seen in hospitals where mobility protocols reduced complications by 15% (14).
3.4. Embracing Technological Innovations
Technological advancements are transforming nurse-led rehabilitation, offering new tools to enhance mobility and care coordination. Wearable devices, such as activity trackers, enable nurses to monitor patients’ step counts and activity levels, improving adherence to mobility goals by 50% (12). These devices provide real-time data, allowing nurses to adjust rehabilitation plans dynamically. Mobile applications also facilitate communication between nurses, patients, and interdisciplinary teams, reporting a 20% improvement in care coordination and patient satisfaction (21).
Telehealth platforms have emerged as a game-changer, particularly for post-discharge care. It was described a virtual rehabilitation program where nurses delivered exercise sessions via video calls, maintaining recovery progress in 75% of patients after leaving the hospital (22). Patient narratives highlight the convenience of telehealth, with older adults feeling more supported in their home environments. However, challenges remain, including digital literacy barriers and unequal access to technology, particularly in rural areas. Nurses address these by providing training and advocating for equitable resource distribution (23).
The narrative also explores the potential of emerging technologies, such as virtual reality (VR) for rehabilitation exercises, which early studies suggest could enhance engagement by 30% (12). While still in its infancy, VR holds promise for making mobility exercises more interactive and motivating. Nurses’ adaptability in integrating these tools underscores their role as innovators in rehabilitation care.
4. Discussions
This narrative synthesis underscores the multifaceted and evolving role of nurses in optimizing the rehabilitation process for older adults following hip fracture. The four themes — Nurses as Mobility Champions, Tailoring Care to Patient Needs, Navigating Barriers to Recovery, and Embracing Technological Innovations — reflect both the direct clinical impact and the broader system-level influence nurses exert. The findings largely align with the existing body of literature, although some studies diverge in their emphasis on implementation feasibility and outcomes across diverse settings.
The results affirm the critical role nurses play in promoting early mobilization, echoing guidelines that recommend initiating movement postoperatively to mitigate immobility-related risks (24). Multiple studies corroborate that structured, nurse-led mobility programs significantly improve functional recovery. However, this is not universally observed across all healthcare settings. Some studies not included in this synthesis report inconsistencies in early mobilization due to institutional inertia, lack of interdisciplinary coordination, or insufficient training for nurses in mobility protocols (25). These discrepancies can be attributed to variations in healthcare system maturity; for instance, in well-resourced settings with strong policy frameworks, nurse-led initiatives thrive, whereas in underfunded environments, competing priorities dilute their impact, highlighting the need for targeted policy interventions to standardize practices globally. These discrepancies suggest that while the role of nurses as "mobility champions" is widely supported, successful implementation may depend on contextual factors such as staffing ratios, institutional policy support, and nurse empowerment at the unit level.
Interestingly, the perception of nurses as emotional motivators — described as “cheerleaders” who alleviate patients’ fear of falling — adds a psychosocial dimension often underemphasized in traditional rehabilitation models. While this aligns with patient-centered care principles, some literature suggests this emotional labor may be under-recognized and inadequately supported within current nursing workloads (26). Analytically, this underscores a gap in traditional models that prioritize physical over psychosocial elements, potentially exacerbating nurse burnout; integrating emotional support training could bridge this, as evidenced by comparative studies showing better long-term adherence in holistic programs versus purely physical ones. This calls for institutional recognition of the dual physical and emotional support roles nurses fulfill in hip fracture rehabilitation.
The theme of individualized care resonates with the contemporary shift toward personalized rehabilitation approaches, particularly in geriatric populations where heterogeneity in physical and psychological status is profound. Studies in this synthesis show that tailored nurse-led interventions significantly improve adherence to rehabilitation and enhance patient outcomes (27). This is consistent with a growing number of interventions that report improved patient satisfaction and functional independence when care plans are customized based on preferences and cognitive status.
Contrastingly, other sources not included in the synthesis question the scalability of highly individualized programs, citing limitations in time, staffing, and resources. Moreover, in some systems where standardization is prioritized for efficiency, deviation from protocols to tailor care may be discouraged, potentially limiting nurses’ autonomy. These conflicting perspectives highlight a tension between the ideals of person-centered care and the constraints of clinical practice environments. This tension may stem from differing healthcare philosophies — patient-centered versus efficiency-driven — suggesting that hybrid models, blending standardization with flexibility, could resolve discrepancies, as supported by analytical reviews advocating for adaptive protocols that empower nurses without compromising scalability. The findings reinforce the argument that empowering nurses to adapt care based on real-time patient assessments should be a system-wide priority.
The identification of both patient-related and systemic barriers is consistent with much of the geriatric rehabilitation literature, where cognitive decline, pain, and psychological distress are frequently cited obstacles to recovery (28). The evidence here suggests that nurses use a range of strategies — educational, emotional, and procedural — to navigate these challenges effectively, contributing to improved patient compliance and outcomes. The value of nurse-led education for caregivers, particularly in reinforcing mobility at home, is a novel finding that complements studies highlighting the importance of family engagement in geriatric care.
Nevertheless, a study argues that the responsibility placed on nurses to counteract systemic barriers — such as inadequate staffing or lack of rehabilitation protocols — is often unsupported. For example, in under-resourced facilities, nurses may lack access to consistent interdisciplinary collaboration, limiting their ability to deliver comprehensive mobility support (29). In these settings, early mobilization is often deprioritized in favor of immediate acute care tasks, undermining the continuity of rehabilitation.
This divergence emphasizes the importance of structural investment in nurse staffing and institutional protocols. Explaining these differences, analytical comparisons reveal that resource disparities across regions amplify barriers, with high-income settings achieving better outcomes through integrated teams, whereas low-resource areas require advocacy for policy reforms to enable similar gains. Studies included in the synthesis showed that when nurses work within team-based models with standardized guidelines, mobility outcomes improved (30), suggesting that system-level changes are crucial for maximizing the effectiveness of nurse-led interventions.
The integration of technology into nurse-led rehabilitation efforts represents a promising frontier. The literature reviewed supports the effectiveness of wearable devices, telehealth platforms, and mobile apps in enhancing care coordination, monitoring, and patient engagement. This aligns with a study advocating for digital solutions in managing chronic and post-acute conditions. The value of real-time data in patient management is a key analytical insight, differentiating from earlier literature focused on manual interventions and explaining why digital tools may outperform traditional methods in adherence and personalization (31).
However, not all studies are uniformly optimistic. Technological integration is uneven across regions, especially in rural or underserved communities where access to reliable internet, digital devices, or even basic digital literacy is lacking. While the included studies suggest nurses are well-positioned to bridge these gaps by providing training and facilitating access, another study raises concerns that without broader infrastructural support, such initiatives may not be sustainable or equitable (32).
The discussion around VR for rehabilitation is emerging, with early studies suggesting increased engagement through interactive exercise (33). While promising, this remains an area of active investigation with questions about cost-effectiveness, accessibility, and clinical validity. Comparatively, VR's potential exceeds static tools in prior literature by fostering immersive experiences, but discrepancies in adoption rates underscore socioeconomic divides, analytically pointing to the need for subsidized programs to ensure equitable access. Nurses’ adaptability in experimenting with such tools is commendable, but institutional backing and clear guidelines will be necessary for widespread adoption.
4.1. Conclusions
This study highlights the critical role of nurses in optimizing rehabilitation outcomes for elderly patients recovering from hip fractures. Through their active involvement in early mobilization, personalized care, and psychological support, nurses significantly enhance functional recovery and quality of life. The findings underscore that nursing-led interventions, when systematically implemented, contribute to substantial improvements in mobility, pain reduction, and overall well-being. By addressing both physical and psychological barriers, nurses facilitate a more efficient and patient-centered rehabilitation process.
One of the key takeaways from this study is the effectiveness of Rehabilitation Self-Efficacy programs and nurse-driven transitional care models in improving recovery outcomes. These structured interventions empower patients to regain confidence in their mobility, leading to greater adherence to rehabilitation exercises. Additionally, the integration of technology-assisted interventions — such as digital monitoring tools and virtual rehabilitation platforms — has shown promising results in maintaining consistent progress. Such innovations enable more precise tracking of recovery and provide tailored feedback, further enhancing patient engagement.
Despite these advances, systemic barriers such as staffing shortages and the lack of standardized mobility protocols continue to challenge the full implementation of effective nursing-led rehabilitation programs. However, nurses have demonstrated remarkable resilience in navigating these limitations, ensuring that patient care remains a top priority. By advocating for interdisciplinary collaboration, they help bridge gaps in rehabilitation services and contribute to a more coordinated approach to patient care.
Given the significant impact of nursing interventions, healthcare systems must prioritize policies and resources that empower nurses to lead rehabilitation initiatives. This includes providing specialized training in mobility protocols, expanding access to advanced technology, and fostering team-based care models that enhance rehabilitation outcomes. Establishing evidence-based standardized protocols can further streamline nursing-led mobility programs, ensuring consistency and effectiveness in patient recovery.
Future research should focus on large-scale trials to refine best practices in nursing-led rehabilitation. Additionally, exploring emerging technologies such as wearable devices and telehealth platforms could expand the reach of nursing interventions, offering more precise and accessible rehabilitation support. By continuing to refine and expand these approaches, healthcare systems can maximize the role of nurses in enhancing recovery outcomes for this vulnerable population.
4.2. Limitations
The included studies varied greatly in design, sample sizes, and type of interventions, which may limit comparability and generalizability. Second, while the majority of the studies reported positive outcomes, some had scant details on the protocols used for intervention, making replication and application difficult. Third, the review had targeted only those studies published in English; this might have led to missing valid studies in other languages. Further, there was an obvious deficit of long-term follow-up studies in many of the selected ones, which impacted the assessment of sustained effects from nursing-led interventions. Finally, this review was based on published data, and as such, there is a chance for publication bias toward including positive studies.