1. Background
Hepatitis is the widespread inflammation of liver parenchyma cells, possibly due to infectious or non-infectious factors (1). Viral hepatitis is mostly caused by hepatotropic viruses named A, B, C, D, and E (2). In acute hepatitis A, humans are the only known reservoir of this virus. It is usually a self-limiting disease, with a wide spectrum of clinical symptoms that occur in some cases with fulminant hepatitis and never become chronic. Its infection causes permanent immunity and can be prevented with vaccines (3). It belongs to the genus of hepatoviruses, is part of the Picornaviridae family, and is a mononucleotide RNA virus with a diameter of 27 nm. The four genotypes of hepatitis A virus (HAV) in humans described so far all belong to a single serotype (4). This virus remains stable at medium temperature and low pH, but it becomes inactive due to high temperature and chloroform (5). It has spread worldwide, and an estimated 1.4 million people get this infection every year. Outbreaks of hepatitis A can occur among different populations, such as outbreaks due to contaminated water or food in mass travel to areas with poor sanitary conditions, among health system workers, and among homeless people (6, 7). The classical symptoms of this hepatitis are less common in young patients and may be asymptomatic in children, especially those under 5 years. In general, the occurrence of disease symptoms in children younger than 6 years is not common (8). Finding the HAV antibody (IgM), which is commonly found at the beginning of signs and peaks in the severe or early stages of the illness, allows for a diagnosis of the ailment (9). Serum IgM in individuals with chronic hepatitis may be falsely positive or reflect symptomatic infection with hepatitis A within the last six months (this is more likely in younger children than in older children or adults) (10). It can also be a sign of long-term persistence of IgM in the absence of medical signs. Serum IgG antibodies appear early in the recovery period of the disease, can be detected for decades, and are a sign of lifelong immunity against this virus (11). In essence, vaccination serves as the fundamental approach to preventing hepatitis A. Using hygienic food and water and following the principles of personal hygiene is the best way to combat this hepatitis (12). With an estimated population of close to 4.5 million, Khuzestan province is a tropical zone in southwestern Iran (Census 2009). The Khuzestan region is adjacent to Iraq and several Arabian nations near the Persian Gulf, encompassing land, rivers, and seas. The main source of knowledge concerning HAV disease in Khuzestan has been obtained from prevalence studies conducted with thalassemic and hemodialysis patients and among groups of intravenous drug users (IDUs). The incidence of HAV in this region's population has not been evaluated. This paper provides an overview of the current knowledge regarding the prevalence of HAV viruses in the Khuzestan region. It includes several aspects such as specific vocations, behaviors, environmental risk factors, and pathways of transmission.
2. Objectives
This study aims to investigate the prevalence of hepatitis A in Khuzestan province over 10 years.
3. Methods
3.1. Sampling
This study was conducted on files related to hepatitis A disease diagnosed in the health centers of Khuzestan province (information registered in the Deputy Health Department's Non-communicable Diseases Unit) between 2013 and 2023. The number of samples, type of health treatment centers, different urban and rural areas, age, gender, history of contact with infected animals, place of residence, occupation, economic status, education, and other relevant factors were recorded. Serum samples were tested for hepatitis B and C using commercial kits. Hepatitis A was detected via an ELISA for IgM antibodies and a Nested RT-PCR method. Viral RNA was extracted and converted to cDNA using reverse transcriptase. The cDNA was then amplified through two rounds of PCR with specific primers to detect the viral genome. The study complies with all criteria and confirms informed consent. This research followed ethical criteria and acquired informed consent from individuals. The Research Ethics Committee of Ahvaz University of Medical Sciences approved this article with the particular number IR.AJUMS.REC.1402.146.
3.2. Statistical Analysis
The collected data were entered into Excel software, and then the coding of the variables was done. SPSS version 22 software was used for data analysis. To describe the variables, the mean and standard deviation for quantitative variables and the frequency and percentage for qualitative variables were used. Then this information was analyzed by a vital statistics expert, and according to the descriptive nature of the study, descriptive statistics such as the minimum rate, maximum rate, average, and relative frequency were used to present the results of the study. The t-test was used to compare means, and the chi-square test was used to compare proportions.
4. Results and Discussion
Acute viral hepatitis A is one of the major health problems transmitted to humans through the fecal-oral route in unsanitary conditions and, in a few cases, leads to acute liver failure and death. Its manifestation may be isolated or occur in a cluster or outbreak. By consuming contaminated food or water, outbreaks or epidemics can be transmitted from a common source, and simultaneously, by consuming contaminated food, vegetables, fruits, and drinking water, the infection can spread from an infected person to healthy individuals over a long period (13).
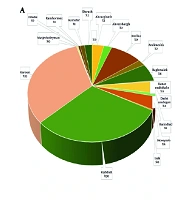
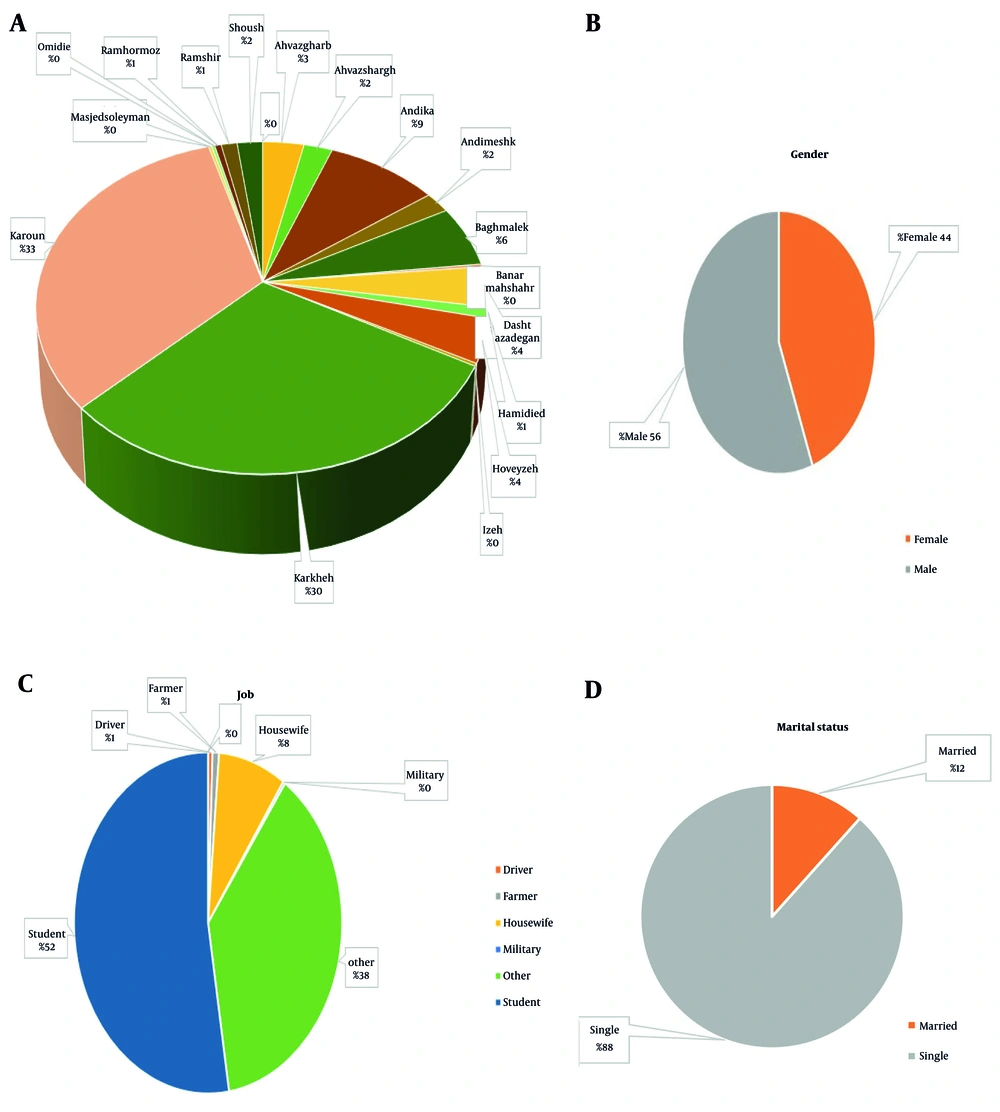
The results of the present study showed that a total of 379 people from the population of Khuzestan province were infected with hepatitis A in 2023. The lowest rate of infection (one person) was related to the cities of Bandar Mahshahr, Izeh, Masjid Suleiman, and Omidiyeh. Most cases of hepatitis A infection were related to the cities of Karun, Karkheh, Endika, Baghmolek, Ahvazgharb, and Dasht Azadegan, with 124 (32.7%), 113 (29.8%), 35 (9.2%), 23 (6.1%), 13 (3.4%), and 15 (4%) cases, respectively (Figure 1A). In terms of gender, 168 (44%) patients were female and 211 (56%) were male (Figure 1B); therefore, the number of men with hepatitis A was greater than the number of women. Most of the people who had hepatitis were students. The number of students with hepatitis was 199, which constituted 52% of the infected (Figure 1C); this means that more than half of the patients were students. Thirty-one people (8.2%) of hepatitis A patients were housewives. There were three, two, and one people infected with hepatitis A among farmers, drivers, and military personnel, respectively. A total of 143 people (37.7%) were infected with hepatitis A. However, the least affected were military occupations (1%), drivers (2%), and farmers (3%). Among the 379 people with hepatitis A, those who lived in rural areas had a higher prevalence than urban residents. One hundred ten people (29%) were urban residents, while 268 people (71%) were rural (Figure 1F). Hepatitis A is a health-related disease, and factors related to economic and social conditions, such as the level of sanitation, access to safe drinking water, and sanitation facilities, play a significant role in its spread. In general, rural communities are more at risk due to poorer sanitation and lower incomes (14).
The findings of this study showed that single people are more likely to get hepatitis A than married people, with 355 people (88%) being single and 44 people (12%) being married (Figure 1D). Independent individuals, especially young adults, are considerably more prone to living in communal environments, such as dormitories or shared accommodations, hence heightening the risk of transmission by intimate contact. Moreover, some research indicates that specific sexual activities prevalent among single individuals may elevate the risk of infection. The hepatitis B virus (HBV) and HAV and are found in bodily fluids, including sperm and vaginal secretions, and can be transmitted through unprotected sexual intercourse, particularly in the presence of tiny cuts or wounds. Engaging in anal sex and having several sexual partners increases the risk. Hepatitis A may also be transmitted by fecal-oral contact, which occurs during specific sexual behaviors (15). Conversely, married persons typically reside in more stable, less communal settings, which may reduce the likelihood of exposure (16).
Studying sexual orientation and high-risk behaviors during academic years, particularly during adolescence and puberty, establishes a scientific foundation for increased vulnerability to hepatitis virus infection. This phase, defined by physiological and psychological transformations, frequently involves exploration and a propensity to transcend limits, potentially resulting in unprotected sexual behavior and multiple partners. Lack of knowledge about hepatitis transmission mechanisms and the importance of safe sexual practices, such as proper condom usage, or the hepatitis vaccine, which offers long-term immunity, significantly increases the risk of infection among this demographic. Long-term infection poses a risk of serious complications, including cirrhosis and liver cancer, in the future (17). The HBV infection is a well-known sexually transmitted infection. Since men who have sex with men (MSM) often have several sexual partners, it is more common among them. Anal intercourse can be more harmful than vaginal intercourse, thereby elevating the danger of blood exposure. The incidence of HBV infection is especially high among individuals who have several sexual partners or encounter sex workers (18).
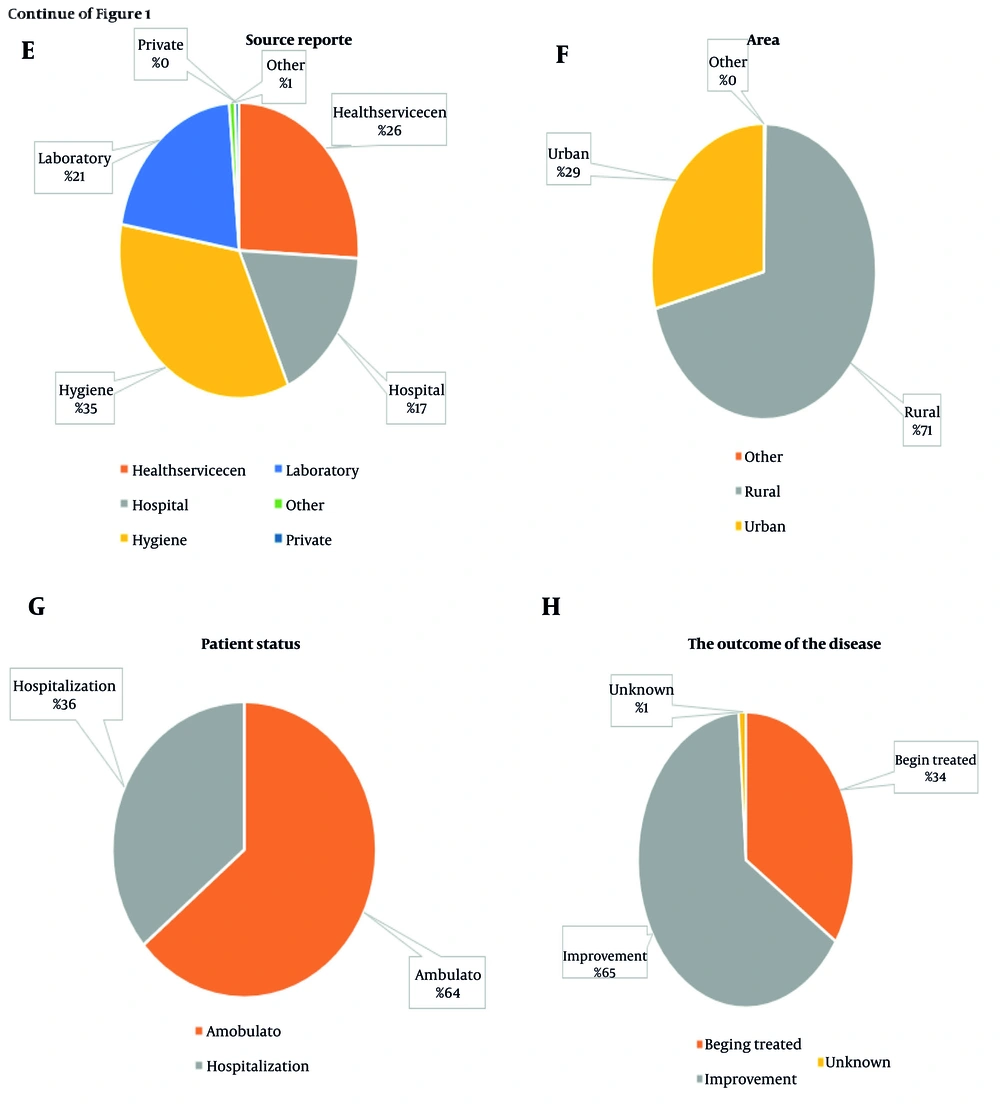
The centers that reported the results of the hepatitis A test include health service networks for 98 people (26%), hospitals for 66 people (17%), health centers for 131 people (35%), and laboratories for 79 people (20%, Figure 1E). Out of a total of 379 people with hepatitis A, 137 people (36%) were hospitalized, and the remaining 242 people (64%) were treated on an outpatient basis (Figure 1G). Out of a total of 379 people with hepatitis A who had been referred to healthcare centers and hospitals, 130 (34%) of them returned and were treated. However, the other 245 people (65%) recovered and did not return to the hospital (Figure 1H). The largest number of unmarried people with hepatitis was observed in Karun (n = 107) and Karkheh (n = 96), and the largest number of married people with hepatitis A was also related to these two cities (n = 17, Figure 1I). The findings of this study showed that the highest number of recovered people was from Karkheh city (n = 113, Figure 1J). The highest number of repeated referrals for retreatment also belonged to the city of Karun (21 people). After Karun (26.9%), Indika (3.2%), and Ahvaz Sharq (1.3%) had the most repeated visits to the hospital (Figure 1L). Most patients who were discharged as outpatients belonged to the cities of Karun (24%), Karkheh (21%), and Andika (5%, Figure 1K). The highest rate of hospitalization was related to the cities of Karun and Karkheh (8.7%) and Andika and Baghmalek (4.2%).
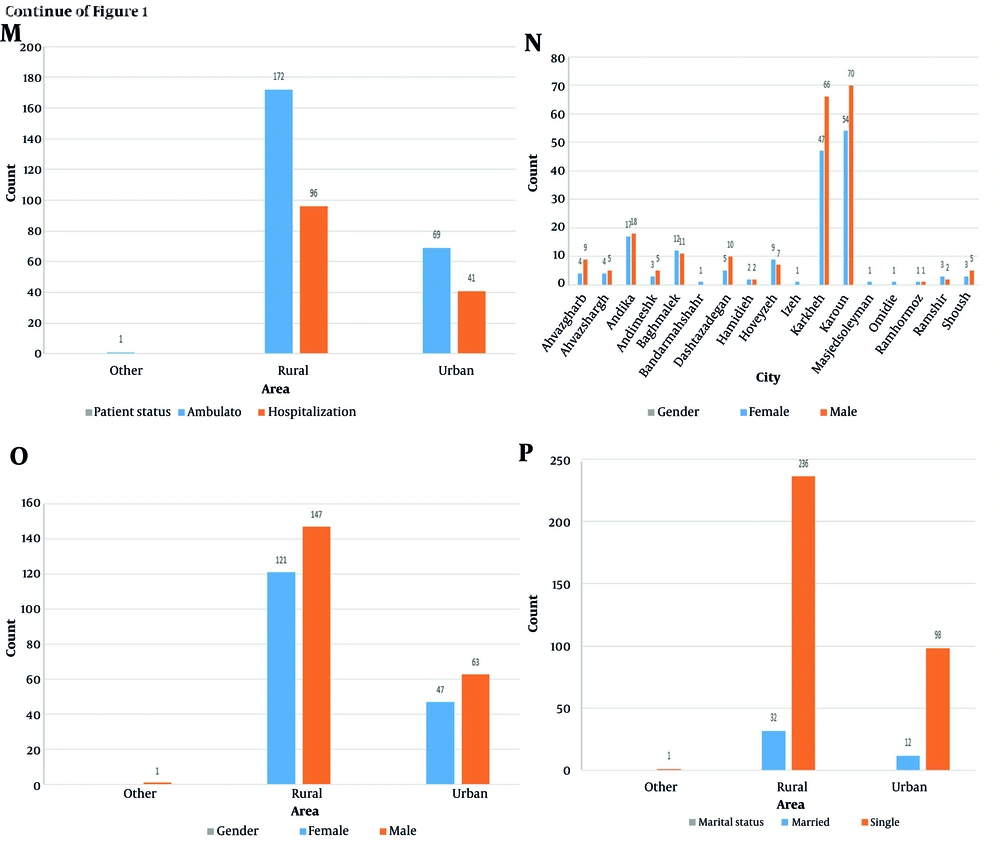
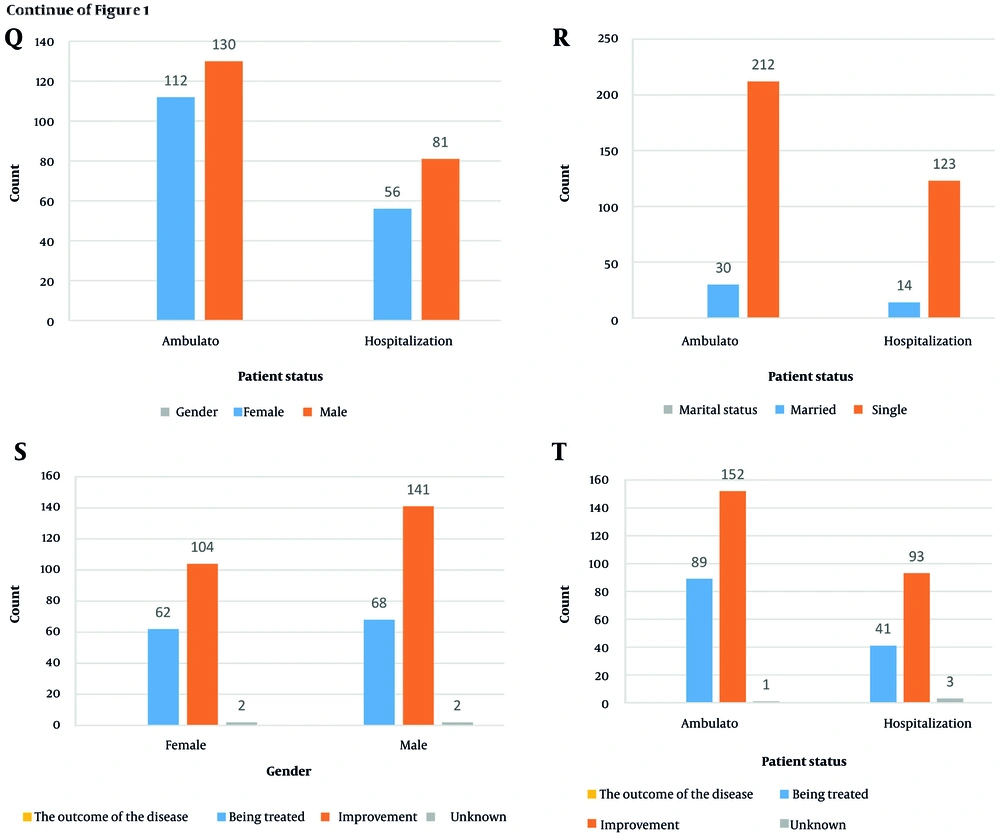
The number of people who recovered after being referred to the hospital in urban areas was equal to the number of people who were referred again (15%). While in rural areas, the number of people who have returned (50%) is almost 2.5 times that of people who have recovered (20%). Forty-five percent of rural people were visited on an outpatient basis, while 18% of urban residents (Figure 1M). Thirty-six percent of the people who were hospitalized were 25% of rural residents, and 11% of urban residents. The highest number of men with hepatitis A belonged to the cities of Karun (n = 70) and Karkheh (n = 66) (Figure 1N). The highest number of infected women belonged to the cities of Karun (n = 54) and Karkheh (n = 47), respectively (Figure 1O). The number of rural men (n = 147) with hepatitis A is greater than the number of urban men (n = 63). Similarly, the number of rural women with hepatitis A (n = 121) exceeds the number of urban women (n = 47). Sixty-two percent of those infected with hepatitis A were single and lived in rural areas, while 25% of them lived in cities (Figure 1P). Eight percent of hepatitis A sufferers are married and rural, but 5% of them are urban. The number of people who were visited as outpatients was 242, with 112 being women and 130 being men (Figure 1Q). The rest of the patients (n = 137) who were hospitalized included 56 women and 81 men. It should be mentioned that 30 people were married and 212 people were single (Figure 1R). Among the 137 hospitalized patients, 123 were single, and the rest (14) were married.
The findings showed that of the 245 people who were treated the first time, 141 were men and 104 were women. However, from the population of 130 people who had repeated treatment, 68 were men and 62 were women (Figure 1S). Among the population of 241 people who were visited as outpatients, 89 people were treated again, and 152 people achieved complete recovery at the first visit. Among the hospitalized population, 41 people were re-treated, but 93 people achieved complete recovery (Figure 1T).
According to the research conducted, the authors found that the cities of Andika, Karkheh, and Karun have a very low health status, and the consumption of contaminated food and water may cause the people of these cities to contract hepatitis A. As the findings of this study show, the highest rate of hepatitis A in Khuzestan province is related to these cities; the three cities of Karun, Karkheh, and Andika include 33%, 30%, and 9% of all hepatitis A patients, respectively. In the report by Ghasemian et al., between November 2014 and January 2015, 9 patients were hospitalized with the diagnosis of acute hepatitis A, of which 7 patients were infected after returning from the collective Arbaeen pilgrimage in Iraq, with the possibility of contamination due to contaminated food or water. After returning, two more people were infected through family contact, and after hospitalization, all of them were discharged with recovery and without complications. Their age range was 19 to 49 years (2 of them were women and the rest were men) (19).
In the September 2019 US CDC Incidence and Mortality Weekly Report, during 1971 - 2017 in 18 states in areas that used unsanitary groundwater, there were 32 outbreaks with 857 cases of acute hepatitis with no deaths or fulminant hepatitis. However, by vaccinating children after 12 months of age since 1996 and monitoring the health of drinking water and health education from 2009 to 2017, there were no other outbreaks of this waterborne disease (13).
Flooding devastates potable water infrastructure and sewage disposal systems. This results in the pollution of potable water sources with sewage and pathogens, including the HAV. Consequently, the danger of waterborne infections, such as hepatitis A, escalates significantly. Inadequate sanitation, particularly in highly populated regions or locations with restricted access to clean water, significantly contributes to the transmission of hepatitis A. Poor handwashing after using the toilet and during food preparation and serving might spread the virus. In summary, in the studied locations, floods provide a conducive environment for the transmission of hepatitis A by compromising sanitation infrastructure. Simultaneously, inadequate personal and public hygiene in these regions promotes the transmission of the virus (20, 21). In two studies conducted in Montreal and Vancouver, Canada, on street children and adolescents, the rates were 4.7% and 6.3%, respectively (22, 23). Unprotected sex is a major route of transmission of HAV and, to a lesser extent, HBV. Students are often exploring their sexuality and may engage in behaviors that increase the risk of exposure to the virus. Living in crowded, closed spaces, such as dormitories, can facilitate the spread of hepatitis. In the present study, there are boarding schools and gifted schools, and students use dormitories; this could be one of the possible reasons for the incidence of hepatitis. While hepatitis is not usually transmitted through casual contact, living in proximity can increase the likelihood of transmission through shared equipment or high-risk behaviors (18).
Many studies have shown that students often have inadequate knowledge about hepatitis, including how it is transmitted and how to prevent it. This can lead to a false sense of security and a failure to take appropriate precautions (24). Another reason why students are more likely to contract hepatitis A in many countries is that universal childhood vaccination programs for hepatitis may not have been completed by some students, or they may be from groups not included in these programs (25). In another study of homeless people in Sydney, Australia, 47% of study participants were HAV-positive (26). In a study in Brazil, the prevalence of antibodies against hepatitis A in street children was 80 - 92.2% (27). In a study conducted by Ataei et al. in Isfahan province, the overall prevalence of HAV positivity was 8.33%, which was estimated to be 10.63% in people aged 6 - 19 years in the province (28). Since the city of Isfahan has purified and hygienic water, it is unlikely that polluted water is the cause of this drastic difference in the level of infection. Considering that most of these children lived in large families (5 people or more) and had a low level of education, the poor health conditions in their families may be the reason for the high prevalence of hepatitis A infection in this group. This indicates the need to educate and inform such families about the importance of observing personal hygiene and the ways of disease transmission. In this study, about 16% of children were involved in sexual relations (29).
In three studies on street youth in Montreal, Canada, 25.7%, 99.3%, and 27.7% were sexually active, and in the first and last cases, they engaged in sex for a living (30).
4.1. Conclusions
The current study, a descriptive study, focused on the prevalence of hepatitis A in Khuzestan province. From 2013 to 2023, the total incidence of hepatitis was reported in healthcare centers. According to the reports obtained, the rate of hepatitis A infection in cities with poor health status, such as Karun, Karkheh, and Indika, was much higher than in other cities in the province. Among the other factors involved in contracting this disease, young age was significant; most of the infected were students. The findings of this study showed that villagers are more at risk than urban dwellers due to a lack of access to safe drinking water. The study also revealed that men suffer from this disease more than women, and singles more than married people. Many factors contribute to the incidence of this disease, but the most important ones are young age (students), poor health conditions, and limited access to safe drinking water.
It is suggested that, in addition to providing safe, sanitary water, special training should be given to people (especially young people) to prevent contracting this disease. Furthermore, vaccination must be completed to effectively combat this disease. The results highlight the critical necessity for a comprehensive public health strategy in Khuzestan province. Prioritizing rural water infrastructure to enable universal access to safe drinking water is essential. Concurrent implementation of targeted school-based vaccination and hygiene education programs is crucial to safeguard at-risk children and disrupt the transmission cycle.
4.2. Potential Reporting Bias
4.2.1. Asymptomatic Cases
Hepatitis A typically goes undiagnosed in youngsters. Asymptomatic cases are unlikely to seek medical attention, and hence, they are not recorded. This leads to a significant underreporting of the population's true infection rate.
4.2.2. Limited Healthcare Access
The study uses data from patients diagnosed at hospitals, clinics, or labs. Remote rural populations with limited access to these institutions may not have been diagnosed, underrepresenting their cases. Given the study's result that rural communities had a greater disease prevalence, this is important.
4.2.3. Socioeconomic Factors
Low-income individuals at higher risk for hepatitis A may be less likely to seek or afford medical care. This may lead to underreporting and bias the study's results, underestimating the disease's burden in vulnerable groups.
4.2.4. Incomplete Follow-up Data
The study found that 65% of patients never returned to the hospital. The cause is unknown. They may have recovered or not been able to afford follow-up care. This biases recovery and complications statistics, potentially underestimating the illness's severity or long-term implications.