1. Background
Juvenile idiopathic arthritis (JIA) is a chronic autoimmune disease of unknown etiology, with onset before age 16 and lasting at least 6 weeks (1). Its prolonged course and potential systemic involvement, such as the liver, heart, spleen, and eyes, can seriously impair children’s physical and mental health (2). Although treatment typically involves biologics, glucocorticoids, and non-steroidal anti-inflammatory drugs, these therapies are not curative. Long-term use often leads to hormone dependence, growth suppression, and osteoporosis, especially in children lacking regular follow-up or adherence to rehabilitation, resulting in varied outcomes and a heavy burden on families (3, 4). Caregivers of children with JIA often experience significant stress due to disease relapses and the lack of a definitive cure. Their limited knowledge of JIA may also hinder effective treatment and nursing support (5). Thus, providing families with scientific, systematic health education is essential for improving disease management and patient outcomes (6). However, routine education in clinical settings is typically limited to verbal instructions or the distribution of educational pamphlets, which often lack personalization and fail to yield satisfactory results.
The Predisposing-Reinforcing-Enabling Constructs in Educational/Environmental Diagnosis and Evaluation (PRECEDE)-Policy, Regulatory, and Organizational Constructs in Educational and Environmental Development (PROCEED) model, developed by Lawrence W. Green in 1980, is a structured framework for health promotion. It integrates sociological, behavioral, and policy factors to design targeted interventions based on predisposing, enabling, and reinforcing elements (7, 8). This model has shown effectiveness in improving lifestyle behaviors in prediabetic adults and enhancing the postoperative quality of life in patients with gastric cancer (9, 10). Despite its broad application, the PRECEDE-PROCEED model has rarely been used in pediatric rheumatology, particularly in educating families of children with JIA. This represents a notable research gap. The present study is among the first to apply this model to JIA family education, aiming to evaluate its impact on disease knowledge, caregiving burden, and behavioral outcomes. This innovative approach may provide a replicable framework for improving family engagement and care quality in chronic pediatric diseases.
2. Objectives
Based on this, the present study investigated the effects of PRECEDE-PROCEED model-based family real-time health education on children with JIA.
3. Methods
3.1. Subjects
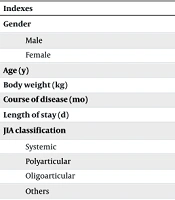
A total of 90 pediatric patients diagnosed with JIA and receiving treatment at our hospital from January 2023 to October 2024 were recruited for this study. The required sample size was calculated using G*Power 3.1 software based on a two-tailed test with an alpha level of 0.05, power (1-β) of 0.80, and an estimated moderate effect size (Cohen’s d = 0.6), yielding a minimum of 45 subjects per group. After obtaining informed consent, patients were sequentially numbered according to their admission order and randomly assigned in a 1:1 ratio to either a control group (routine nursing and routine health education) or a study group (routine nursing and PRECEDE-PROCEED model-based family real-time health education) using a random number table. Allocation was conducted by an independent researcher not involved in outcome assessment or data analysis. Outcome assessors and data analysts were blinded to group assignments to minimize potential bias. No significant differences were observed between the two groups in terms of gender, age, body weight, disease duration, length of stay, JIA classification, or family education level (P > 0.05, Table 1).
| Indexes | Study Group (N = 45) | Control Group (N = 45) | Statistical Value | P |
|---|---|---|---|---|
| Gender | χ2 = 0.729 | 0.393 | ||
| Male | 28 (62.22) | 24 (53.33) | ||
| Female | 17 (37.78) | 21 (46.67) | ||
| Age (y) | 10.32 ± 1.04 | 10.65 ± 1.02 | t = 1.520 | 0.132 |
| Body weight (kg) | 37.46 ± 3.23 | 38.07 ± 3.38 | t = 0.875 | 0.384 |
| Course of disease (mo) | 12.58 ± 1.15 | 12.82 ± 1.19 | t = 0.973 | 0.333 |
| Length of stay (d) | 11.77 ± 1.21 | 11.86 ± 1.03 | t = 0.380 | 0.705 |
| JIA classification | χ2 = 1.600 | 0.659 | ||
| Systemic | 11 (24.44) | 13 (28.89) | ||
| Polyarticular | 26 (57.78) | 28 (62.22) | ||
| Oligoarticular | 4 (8.89) | 2 (4.44) | ||
| Others | 4 (8.89) | 2 (4.44) | ||
| Family educational level | χ2 = 0.554 | 0.758 | ||
| Elementary school and below | 5 (11.11) | 6 (13.33) | ||
| Junior high school/technical secondary school/high school | 13 (28.89) | 10 (22.22) | ||
| Junior college and above | 27 (60.00) | 29 (64.44) |
Abbreviation: JIA, juvenile idiopathic arthritis.
a Values are expressed as No. (%) or
3.2. Inclusion and Exclusion Criteria
The inclusion criteria were as follows: (1) Children who met the diagnostic criteria for JIA established by the American College of Rheumatology (ACR) (11), (2) families providing signed consent and understanding the study content, (3) children and their families without cognitive, communication, or comprehension impairments, and able to cooperate with study procedures, and (4) children with relatively stable disease status and no recent treatment changes. The exclusion criteria were: (1) Children with severe organ dysfunction, malignant tumors, hematological or systemic immune diseases, or infectious diseases, (2) those experiencing acute infectious conditions requiring immediate hospitalization, (3) cases of arthritis with a clearly defined alternative etiology (such as rheumatic fever and autoimmune disorders), or (4) children with diagnosed neurological or psychiatric disorders.
Note: The treatment of enrolled children conformed to contemporary JIA management strategies as recommended by ACR guidelines, including the use of NSAIDs, DMARDs, and biologic agents (such as TNF inhibitors). Families of children receiving immunosuppressive or biologic therapies were also counseled regarding the timing and safety of age-appropriate vaccinations in accordance with pediatric immunization schedules and rheumatology consensus statements.
3.3. Methods for Control Group
Children in the control group received routine nursing care and standard health education. Routine nursing included the following components
3.3.1. Vital Sign Monitoring
Children’s vital signs were regularly assessed to detect potential complications. Given that JIA typically presents with remittent fever, with one to two peaks within 24 hours, sometimes accompanied by a rash, body temperature was measured every 4 hours, with an additional check 1 hour after antipyretic administration. Particular attention was paid to whether the rash subsided with defervescence, the presence of skin ulceration, or the emergence of new rashes.
3.3.2. Pain Management
As JIA is often associated with joint swelling, pain, and muscle soreness, pain relief was provided through physical or pharmacological methods based on physician recommendations. Caregivers were also encouraged to distract children using music, videos, or other engaging activities.
3.3.3. Monitoring of Potential Complications
Due to the possibility of systemic involvement in JIA, including elevated liver transaminase, pericardial effusion, pleural effusion, interstitial lung disease, acute respiratory distress syndrome, or meningitis, close monitoring of respiratory rate, skin integrity, bleeding signs, blood pressure, and mental status was performed. Risk assessments were documented promptly, and any abnormalities were reported immediately to physicians.
3.3.4. Psychological Support
Nurses responded to caregivers’ concerns in a timely manner and guided families in alleviating children’s anxiety through recreational activities and comforting strategies.
3.3.5. Dietary Guidance and Functional Rehabilitation
Families were encouraged to assist children in gradually resuming daily activities, including dressing, washing, and toileting, and to provide a bland, nutritious diet to support recovery. Clinical monitoring focused on complications related to both the disease and treatment side effects (such as hepatotoxicity, infections), especially in children receiving methotrexate or biologics.
Routine health education involved the distribution of department-issued brochures covering basic knowledge of JIA, conventional treatment options (such as NSAIDs, methotrexate), the role of biologics (such as etanercept, adalimumab), joint protection techniques, adverse event monitoring (such as injection site reactions, infection warning signs), and immunization guidance for immunocompromised children. Nurses conducted oral explanations and responded to families’ concerns regarding injection procedures and safety during immunosuppressive therapy.
3.4. Methods for Study Group
In addition to the aforementioned routine nursing care, the study group received family real-time health education based on the PRECEDE-PROCEED model. The specific measures of PRECEDE-PROCEED model-based family real-time health education were as follows
3.4.1. Behavior Diagnosis Stage (Predisposing-Reinforcing-Enabling Constructs in Educational/Environmental Diagnosis and Evaluation)
3.4.1.1. Sociological Assessment
The quality of life and needs of JIA children and their families were assessed through the PedsQL™ Family Impact Module and customized semi-structured interviews with caregivers. These tools captured the effects of JIA on learning ability, daily functioning, emotional well-being, and caregiver burden. Supplementary data were obtained from literature reviews to contextualize social support needs.
3.4.1.2. Epidemiological Assessment
Epidemiological features of JIA, including prevalence, disease subtypes, and risk factors, were identified through systematic literature reviews of national and international data. To assess modifiable risk behaviors within families, a structured Health Behavior Questionnaire was administered, collecting information on physical activity patterns, smoking exposure, parental education level, and dietary habits.
3.4.1.3. Behavioral and Environmental Assessment
A combination of Likert-scale surveys and structured interviews was used to evaluate living environments, health behaviors, treatment attitudes, and access to JIA-related resources. Family understanding of JIA management, including biologic therapy use and immunization protocols for immunosuppressed children, was assessed via a JIA-Specific Knowledge Questionnaire.
3.4.1.4. Educational and Ecological Assessment
Predisposing factors (such as knowledge of JIA, treatment beliefs, self-efficacy), enabling factors (such as availability of professional education, access to pediatric rheumatology services), and reinforcing factors (such as ongoing feedback and encouragement of healthy behavior) were evaluated using a modified PRECEDE survey framework, adapted to the JIA context. Responses were scored to identify priority areas for tailored intervention.
3.4.1.5. Administrative and Policy Assessment
A review of local and national JIA-related healthcare policies, immunization programs, and access to biologic therapies was conducted. Institutional capabilities for managing advanced therapies (such as subcutaneous biologics, long-term monitoring protocols) were assessed through hospital administrative records and interviews with clinical leadership.
3.4.2. Health Intervention Stage (Policy, Regulatory, and Organizational Constructs in Educational and Environmental Development)
In the health intervention stage (PROCEED), education was tailored to address the identified predisposing, enabling, and reinforcing factors
3.4.2.1. Education Addressing Predisposing Factors
At admission, nurses conducted one-on-one sessions with families, focusing on the etiology, clinical manifestations, and therapeutic regimens for JIA, in alignment with the CAR guidelines. Educational sessions incorporated PowerPoint presentations and videos, with each lecture covering a distinct theme (such as types of treatment including DMARDs and biologic agents, injection techniques, side effect management, and vaccine precautions). Families who missed lectures due to scheduling conflicts received individualized make-up education. Prior to discharge, families received a structured mind map of key JIA health education themes, with central topics including pharmacological management (such as methotrexate, TNF inhibitors), fever management, home-based physical therapy, skin care, and infection prevention (such as safe vaccination practices and early identification of infection signs) as the first-level branches. Each first-level branch was dispersed into 2 - 4 second-level branches, each of which continued to be dispersed into 2 - 4 third-level branches. Color-coded branches helped improve comprehension and retention. After discharge, continuous intervention was conducted through multiple channels: WeChat Mini Program, which provided weekly updates on JIA-related risk factors, home-based exercise routines, dressing and dietary guidance, and key aspects of home care; instructional exercise videos, which families were instructed to watch with the child and follow as appropriate; online discussion salons, where families were encouraged to share their experiences with exercise and home rehabilitation, and to raise questions that were addressed in real time; and tracking and supervision, involving daily reminder messages sent to families to prompt training and check-in activities.
3.4.2.2. Education Addressing Enabling Factors
Customized educational videos based on ACR guidelines and expert consensus on JIA treatment — including biologic injection techniques, infection control, and recommended pediatric vaccine schedules — were produced and distributed via official hospital WeChat accounts.
3.4.2.3. Education Addressing Reinforcing Factors
Unhealthy behaviors (such as poor compliance with injection schedules, fear of injections) were identified and corrected through weekly phone calls, outpatient follow-ups, and digital chat groups. Families were coached to support children emotionally by using storytelling, positive reinforcement, and structured routines. Progress was regularly acknowledged to build children's self-efficacy and engagement with treatment.
3.5. Evaluation of Outcomes
3.5.1. Family Mastery Degree of Disease Knowledge
Prior to the intervention and three months afterward, family members’ knowledge of JIA was evaluated using a self-developed JIA Health Knowledge Questionnaire designed by our department. The questionnaire covers four dimensions: Knowledge of JIA treatment, dietary precautions, medication safety, and daily rehabilitation exercises, with each domain scored on a scale of 0 to 25. A higher score indicates greater mastery of disease-related knowledge. The questionnaire was reviewed by experts to ensure content validity, and a pilot test showed good internal consistency, with a Cronbach's α coefficient of 0.856.
3.5.2. Family Perception of Disease Burden and Coping Styles
The Family Burden Scale of Disease (FBS) and the Medical Coping Modes Questionnaire (MCMQ) were used to evaluate family burden and coping styles, respectively, before and 3 months after the intervention. The FBS, originally developed by Pai and Kapur, has been widely translated into Chinese and validated in chronic disease studies (12). It contains 24 items across 6 dimensions, scored 0 - 2 (no burden to severe burden), with a total score range of 0 - 48. The Chinese version of the scale showed acceptable internal consistency with a Cronbach’s α of 0.86 (13). The MCMQ includes 20 items divided into three subscales: Facing (items 1, 2, 5, 10, 12, 15, 16, and 19), avoidance (items 3, 7, 8, 9, 11, 14, and 17), and yielding (items 4, 6, 13, 18, and 20), with each item scored 1 - 4 (8 items are scored in reverse). The Chinese version, translated and validated by Shen and Jiang, has shown acceptable construct validity and a Cronbach’s α ranging from 0.69 to 0.76 for the subscales (14).
3.5.3. Child Treatment Compliance
A hospital-developed Treatment Compliance Questionnaire was used to assess children’s adherence during nursing. It includes items such as whether the child cries during treatment, takes medication on time, and cooperates with each treatment session. The total score is 100. Based on the score, compliance was categorized as: Fully compliant (≥ 80), partially compliant (60 - 79), and non-compliant (< 60). The treatment compliance rate was calculated as: (Number of fully compliant + partially compliant cases)/Total number of cases × 100%. This questionnaire was evaluated through expert consultation for content validity. Based on responses from the study sample, the internal consistency was acceptable (Cronbach’s α = 0.80).
3.5.4. Child Self-esteem and Anxiety Levels
The Children Self-esteem Scale (CSES) and the screen for child anxiety related emotional disorders (SCARED) were used to assess children's self-esteem and anxiety, respectively, before and 3 months after the intervention (15, 16). The CSES consists of 21 items, scored 1 - 5 from strongly agree to strongly disagree, with a total score range of 21 - 105; higher scores indicate a higher self-esteem level. The Chinese version, translated and revised by Ji and Yu, has shown good psychometric properties with a Cronbach’s α of 0.80 (17). The SCARED, with 41 items across five subscales, including somatization panic (13 items), school phobia (4 items), social phobia (7 items), general anxiety disorder (9 items), and separation anxiety (8 items), is scored 0 - 2 for none to frequent. The total score ranges from 0 to 82, and the higher the score, the more severe the anxiety of children will be. The Chinese version, translated by Su et al. and tested in school-age children, demonstrated high reliability (Cronbach’s α = 0.89) and good construct validity (18).
3.6. Statistical Analysis
Statistical analyses were performed using SPSS 23.0 software. Measurement data were presented as mean ± standard deviation
4. Results
4.1. Family Mastery Degree of Disease Knowledge
After three months of intervention, scores in all four domains of the JIA Health Knowledge Questionnaire, including treatment knowledge, dietary precautions, medication safety, and daily rehabilitation exercise, increased significantly in both groups (P < 0.05). Moreover, post-intervention scores were significantly higher in the study group than in the control group (P < 0.05, Table 2).
| Groups | Knowledge of JIA Treatment | Dietary Precautions | Knowledge of Medication Safety | Daily Rehabilitation Exercise | ||||
|---|---|---|---|---|---|---|---|---|
| Before Intervention | After 3 mo of Intervention | Before Intervention | After 3 mo of Intervention | Before Intervention | After 3 mo of Intervention | Before Intervention | After 3 mo of Intervention | |
| Study (n = 45) | 8.37 ± 1.12 | 20.63 ± 2.34 b | 9.51 ± 1.28 | 21.72 ± 1.93 b | 7.49 ± 1.41 | 20.55 ± 2.68 b | 9.11 ± 1.62 | 22.78 ± 1.09 b |
| Control (n = 45) | 8.56 ± 1.09 | 15.69 ± 1.78 b | 9.46 ± 1.14 | 16.87 ± 2.35 b | 7.83 ± 1.45 | 16.49 ± 1.76 b | 9.27 ± 1.46 | 17.52 ± 2.68 b |
| t | 0.816 | 11.271 | 0.204 | 19.031 | 1.128 | 8.495 | 0.492 | 12.196 |
| P | 0.417 | < 0.001 | 0.839 | < 0.001 | 0.263 | < 0.001 | 0.624 | < 0.001 |
Abbreviation: JIA, juvenile idiopathic arthritis.
a Values are expressed as
b P < 0.05 vs. the same group before intervention.
4.2. Family Perception of Disease Burden and Coping Styles
After three months of intervention, both groups showed significant reductions in FBS scores as well as in the avoidance and yielding subscale scores of the MCMQ, accompanied by a significant increase in the facing subscale score (P < 0.05). Furthermore, compared to the control group, the study group exhibited significantly greater decreases in FBS score and in avoidance and yielding scores, along with a significantly higher increase in the facing score in the MCMQ (P < 0.05, Table 3).
| Groups | FBS Score | MCMQ Score | ||||||
|---|---|---|---|---|---|---|---|---|
| Facing | Avoidance | Yielding | ||||||
| Before Intervention | After 3 mo of Intervention | Before Intervention | After 3 mo of Intervention | Before Intervention | After 3 mo of Intervention | Before Intervention | After 3 mo of Intervention | |
| Study (n = 45) | 36.09 ± 2.62 | 15.51 ± 3.78 b | 15.51 ± 3.72 | 27.52 ± 2.79 b | 23.22 ± 1.75 | 11.34 ± 2.67 b | 16.71 ± 2.23 | 8.37 ± 1.02 b |
| Control (n = 45) | 35.51 ± 2.75 | 22.38 ± 3.95 b | 15.89 ± 3.64 | 21.28 ± 2.05 b | 22.97 ± 1.68 | 15.59 ± 3.06 b | 16.08 ± 2.14 | 12.64 ± 1.57 b |
| t | 1.024 | 8.429 | 0.490 | 12.091 | 0.691 | 7.020 | 1.367 | 15.299 |
| P | 0.309 | < 0.001 | 0.626 | < 0.001 | 0.491 | < 0.001 | 0.175 | < 0.001 |
Abbreviations: FBS, Family Burden Scale of Disease; MCMQ, Medical Coping Modes Questionnaire.
a Values are expressed as
b P < 0.05 vs. the same group before intervention.
4.3. Child Treatment Compliance
The treatment compliance rate was significantly higher in the study group compared to the control group (97.78% vs. 80.00%, P < 0.05). Overall, the study group demonstrated superior treatment compliance relative to the control group (P < 0.05, Table 4).
| Groups | Fully Compliant | Partially Compliant | Non-compliant | Compliance Rate |
|---|---|---|---|---|
| Study (n = 45) | 41 (91.11) | 3 (6.67) | 1 (2.22) | 44 (97.78) |
| Control (n = 45) | 23 (51.11) | 13 (28.89) | 9 (20.00) | 36 (80.00) |
| Z/χ2 | Z = 4.177 | χ2 = 7.200 | ||
| P | < 0.001 | 0.007 | ||
a Values are expressed as No. (%).
4.4. Child Self-esteem and Anxiety Levels
Following three months of intervention, both groups exhibited a significant increase in CSES scores and a decrease in SCARED scores compared to those before the intervention (P < 0.05). Moreover, the study group demonstrated significantly higher CSES scores and lower SCARED scores than the control group after the intervention (P < 0.05, Table 5).
Abbreviations: CSES, Children Self-esteem Scale; SCARED, screen for child anxiety related emotional disorders.
a Values are expressed as
b P < 0.05 vs. the same group before intervention.
5. Discussion
The JIA is one of the most common connective tissue diseases in childhood. Symptoms such as joint swelling and pain are often exacerbated during febrile episodes but typically subside as the fever resolves. Recurrent disease attacks may lead to joint ankylosis, which, if not managed properly through timely treatment and care, can significantly increase the risk of permanent joint damage in affected children. As the primary caregivers, families play a critical role in the daily management of JIA. Their level of knowledge and understanding of the disease directly influences the quality of care provided to the child. Therefore, it is essential to assess and address the health education needs of these families through structured, real-time health education. Routine health education is typically delivered through written materials or oral instruction. However, such approaches are often limited by their monotony, lack of interactivity, and failure to consider individual family differences. Consequently, the effectiveness of routine education is frequently suboptimal, highlighting the need for improved and more personalized health education models.
Li et al. applied routine health education and the PRECEDE-PROCEED model to 116 mothers of premature infants and found that those in the PRECEDE-PROCEED model group achieved significantly higher scores in nursing knowledge, caregiving skills, maternal self-efficacy, and self-competence compared to the routine health education group (19). Similarly, Arshad et al. employed the PRECEDE-PROCEED model to promote healthy eating habits among middle school girls. Their study demonstrated that the model effectively increased students' awareness of nutritious food and healthy lifestyles, positively influenced their attitudes toward balanced diets, and ultimately improved health-related behaviors through structured interventions including questionnaires, dietary assessments, and educational lectures (20). Consistent with these findings, the present study revealed that, compared to the control group, the study group showed significantly higher scores in disease knowledge and in the facing dimension of the MCMQ, along with significantly lower scores on the FBS and the avoidance and yielding dimensions of the MCMQ. These results suggest that family real-time health education based on the PRECEDE-PROCEED model offers clear advantages in improving disease-related knowledge, reducing perceived burden, and fostering more adaptive coping styles among families of JIA children. These benefits may be attributed to the structured design of the PRECEDE-PROCEED model, which includes two major phases: The PRECEDE phase focuses on evaluating the health knowledge, beliefs, attitudes, and behavioral patterns of JIA children and their families, while the PROCEED phase emphasizes the implementation of targeted interventions based on these assessments. This comprehensive approach addresses both individual behavioral determinants and external environmental factors, thereby enhancing family understanding of JIA and improving the quality of daily nursing care (21, 22). Health education serves as the core component of the PRECEDE-PROCEED model. In this study, family cognition and caregiving capacity were strengthened through multiple strategies: One-on-one health education sessions at admission, regular health lectures during hospitalization, pre-discharge intensive education on knowledge gaps using mind maps, and continuous post-discharge support via WeChat-based educational content and online Q&A salon activities (23, 24). Mind mapping, as a novel educational tool, effectively presents complex information in a structured and visually engaging format using colors, lines, images, and keywords. This approach clarifies hierarchical relationships among concepts and facilitates better comprehension and memory retention among family members. Consequently, the quality of health education is enhanced, and families experience reduced psychological burden in caring for their children (25, 26).
In the present study, the study group demonstrated higher treatment compliance and CSES scores, along with lower scores on the SCARED, compared with the control group following the intervention. These findings indicate that family real-time health education based on the PRECEDE-PROCEED model contributes to improved treatment adherence and self-esteem, as well as reduced anxiety, among children with JIA. This effect may be attributed to the model’s ability to enhance families’ understanding of the disease and improve their caregiving competencies. By equipping caregivers with better knowledge and practical skills, the model enables families to support the development of healthy behaviors in children, promote adherence to treatment regimens, and more effectively meet the children's daily care needs. This comprehensive support, in turn, helps alleviate psychological distress and fosters greater self-esteem in affected children (27).
5.1. Conclusions
In conclusion, family real-time health education based on the PRECEDE-PROCEED model can effectively enhance treatment compliance and self-esteem in children with JIA, improve disease-related knowledge among family members, reduce children’s anxiety and families’ perceived disease burden, and promote the adoption of positive coping strategies. These findings support the value of this model as a promising approach for clinical application and broader implementation in pediatric rheumatology interventions.
5.2. Strengths
This study is among the first to apply the PRECEDE-PROCEED model to family health education in children with JIA, offering a novel, theory-based framework in pediatric rheumatology. While the model has been used in other health contexts, its application in JIA remains limited, highlighting the innovation of this approach.
5.3. Limitations
Several limitations should be noted. First, the relatively small sample size may limit the statistical power, particularly in the context of multiple outcome comparisons. Second, the 3-month follow-up period may not be sufficient to evaluate the long-term sustainability of the intervention effects. Third, the study relied primarily on behavioral and psychological outcomes, without incorporating disease-specific clinical indicators such as JIA activity scores, which may constrain the clinical interpretability of the findings. Future studies with larger sample sizes, extended follow-up periods, and inclusion of objective clinical measures are needed to validate and strengthen the generalizability of these results.