1. Background
Developmental dysplasia of the hip (DDH) spans from acetabular immaturity to dislocation and, without early management, leads to pain, gait limitation, and early osteoarthritis. The optimal window for non-operative correction is early infancy; universal ultrasound screening is therefore a public-health priority (1, 2).
Reported DDH incidence varies internationally due to genetic, cultural, and programmatic factors. Turkey has implemented universal infant hip ultrasonography (US) screening for over a decade; however, province-level performance data from the southeastern region are sparse, limiting the ability to optimize local implementation. This study analyzes a large real-world cohort from Batman province to provide actionable metrics on incidence, risk-factor mix, laterality, and treatment patterns within a universal program.
The global incidence of DDH varies substantially depending on geographic, ethnic, and genetic factors. Reported rates range from 1.5% to 2% in Europe, whereas in Turkey, studies have shown an incidence between 1% and 1.5% (1, 3). Such variations are also influenced by differences in neonatal care practices, cultural habits (e.g., swaddling), and the availability of routine screening programs.
Multiple risk factors have been identified for DDH, including female sex, positive family history, firstborn status, breech presentation, oligohydramnios, multiple pregnancy, and Caucasian ethnicity (4). Clinically, the diagnosis is often suggested by signs such as limitation in hip abduction, asymmetrical skin folds, limb-length discrepancy, and the presence of Ortolani and Barlow signs during physical examination (4, 5). However, physical examination alone may fail to detect many early-stage or subclinical cases.
Ultrasonographic examination of the hips, particularly using the Graf method, is the gold standard for early detection of DDH in infants younger than six months, when the femoral head is not yet ossified (3). The US is non-invasive, reproducible, and allows for classification of hip morphology, enabling early diagnosis and conservative treatment. It is most effective when applied during the first 4 - 12 weeks of life, a critical window for successful intervention.
Recognizing the importance of early diagnosis, the Turkish Ministry of Health implemented a mandatory national hip US screening program in 2012, aimed at detecting DDH before clinical symptoms emerge. While this initiative has improved early detection and reduced the rate of late diagnosis, regional differences in implementation, population characteristics, and healthcare access continue to affect outcomes.
Despite nationwide efforts, DDH remains a notable pediatric orthopedic issue in Turkey. There is a need for region-specific data to evaluate the effectiveness of screening programs and inform national health policy. Therefore, the aim of this study was to assess the incidence and characteristics of DDH based on a large-scale screening cohort in Turkey, and to contribute reliable, population-based data to the existing literature. Beyond confirming known risk markers (e.g., female sex, primiparity, breech), we characterize treatment patterns and laterality at the population level and outline program implications for quality improvement.
2. Objectives
This study aims to determine the incidence of DDH in southeastern Turkey and to assess the clinical outcomes of a large-scale, population-based ultrasound screening program conducted in Batman province. Additionally, the study seeks to identify associated risk factors contributing to the development of DDH.
3. Methods
3.1. Study Design and Setting
Retrospective, single-province cohort covering all infants who underwent universal hip US screening as part of the national DDH program in Batman province between 1 January 2022 and 31 December 2023 at state hospitals.
3.2. Study Population, Eligibility, and Indications
- Indication: Universal screening of all infants aged 3 - 12 weeks, regardless of risk factors.
- Inclusion: First available ultrasound (Graf method) for each infant within the study window.
- Exclusion: Duplicate examinations; records missing essential variables (sex, Graf type, laterality).
- Participant flow: During the study period, 20,241 hip US examinations were performed. After removing 9,451 duplicate examinations, 10,790 unique infants remained. Of these, 151 infants were excluded due to missing essential variables (sex, Graf type, laterality), leaving 10,639 infants for analysis.
3.3. Ultrasound Technique and Classification
Standard coronal planes were obtained and classified per Graf: Type 1 (normal), type 2a (physiologically immature, followed and re-imaged), type 2b/2c/D (dysplastic), and type 3 - 4 (dislocated). Type 2a hips that normalized on follow-up were not counted as incident DDH.
3.4. Variables and Definitions
- Demographics and perinatal factors: Sex, firstborn status, breech presentation, oligohydramnios, multiple gestation, family history. Laterality and initial management (Pavlik vs. closed reduction) were recorded.
- Prenatal information: Fetal presentation (vertex/breech) was abstracted from obstetric documentation where available. Maternal infections (e.g., TORCH), medication exposures, and associated neonatal anomalies (e.g., torticollis, clubfoot) were not systematically captured.
- Combined risk-factor burden: Composite variables ≥ 1 risk factor and ≥ 2 risk factors were computed in the complete-case subset.
3.5. Statistical Analysis
Categorical variables are presented as No. (%). Associations between DDH (yes/no) and risk factors were tested using Pearson’s chi-square and Fisher’s exact test (if any expected cell < 5). For 2 × 2 tables, odds ratios (ORs) with 95% confidence intervals (CIs) were calculated (Haldane-Anscombe correction applied when needed). Two-sided P < 0.05 was considered statistically significant. Analyses were performed in IBM SPSS 26. Comparisons used complete-case denominators.
4. Results
A total of 10,639 infants underwent routine bilateral hip US screening between January 2022 and December 2023. The mean age at screening ranged between the 2nd and 8th weeks of life. Of the screened infants, 5,414 (50.9%) were male and 5,225 (49.1%) were female.
4.1. Distribution by Graf Classification
Initial US findings based on the Graf classification are presented in Table 1. The majority of infants (n = 9,450, 88.8%) had type 1 hips, considered normal. After follow-up of type 2a, 616 infants (5.8%) met DDH criteria (≥ type 2b). The remaining cases were distributed as follows: Type 2a: 551 infants (5.2%), type 2b: 391 infants (3.7%), type 2c: 155 infants (1.5%), type D: 65 infants (0.6%), and type 3: 27 infants (0.2%)
| Graph Classes | Results of Cases |
|---|---|
| Type 1 | 9450 (88.8) |
| Type 2a | 551 (5.2) |
| Type 2b | 391 (3.7) |
| Type 2c | 155 (1.5) |
| Type 2d | 65 (0.6) |
| Type 3 | 27 (0.2) |
a Values are expressed as No. (%).
b Descriptive distribution; hypothesis testing not applicable.
Overall, 1,189 infants (11.1%) had hips classified as Graf Type 2a or higher at the initial screening. On follow-up US, the hip structure normalized in 573 cases (48.2%), whereas 616 infants (51.8%) continued to show pathological findings and were subsequently diagnosed with DDH, as shown in Table 2.
4.2. Characteristics of Infants Diagnosed with Developmental Dysplasia of the Hip
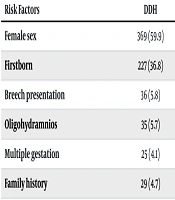
Among DDH infants (n = 616), 59.9% were female; 54.5% had bilateral involvement. 93.7% received a Pavlik harness; 6.3% underwent closed reduction. Clinical and demographic features of infants diagnosed with DDH (n = 616) are presented in Table 3. Of these:
- 369 (59.9%) were female.
- 247 (40.1%) were male.
| Variables | Values |
|---|---|
| Total cases | |
| Normal | 10023 (94.2) |
| Pathological | 616 (5.8) |
| Gender | |
| Male | 247 (40.1) |
| Girl | 369 (59.9) |
| Treatment | |
| Pavlik bandage | 577 (93.7) |
| Closed reduction | 39 (6.3) |
| Localization | |
| Bilateral | 336 (54.5) |
| Unilateral | 280 (45.5) |
| Family history | |
| Yes | 29 (4.7) |
| No | 429 (69.6) |
| Unknown | 158 (25.7) |
| First child | |
| Yes | 227 (36.8) |
| No | 389 (63.2) |
| Breech thrust | |
| Yes | 36 (5.8) |
| No | 580 (94.2) |
| Multiple pregnancy | |
| Yes | 25 (4.1) |
| No | 591 (95.9) |
| Oligohydramnios in pregnancy | |
| Yes | 35 (5.7) |
| No | 283 (45.9) |
| Unknown | 298 (48.4) |
a Values are expressed as No. (%).
b Descriptive distribution; hypothesis testing not applicable
In terms of hip involvement:
- Bilateral DDH was identified in 336 infants (54.5%).
- Unilateral involvement was noted in 280 infants (45.5%).
4.3. Treatment Methods
Among infants with DDH:
- 577 cases (93.7%) were treated conservatively with a Pavlik harness.
- 39 infants (6.3%) underwent closed reduction.
4.4. Associated Risk Factors
Complete-case comparisons (Table 4) showed that female sex was significantly associated with DDH (59.9% vs. 48.5%; OR: 1.59, 95% CI: 1.35 - 1.88; P = 3.4 × 10-8). Primiparity was less frequent in DDH than in non-DDH (36.8% vs. 42.8%; OR: 0.78, 95% CI: 0.66 - 0.92; P = 3.5 × 10-3). Breech presentation was not significantly associated with DDH (5.8% vs. 7.6%; OR: 0.76, 95% CI: 0.54 - 1.07; P = 0.115). Oligohydramnios (5.7% vs. 0.9%; OR: 6.36, 95% CI: 4.28 - 9.46; P = 1.6 × 10-25), multiple gestation (4.1% vs. 0.1%; OR: 35.29, 95% CI: 17.64 - 70.59; P = 7.0 × 10-23), and family history (4.7% vs. 0.1%; OR: 54.97, 95% CI: 25.90 - 116.66; P = 6.9 × 10-29) showed strong associations with DDH.
| Risk Factors | DDH | No DDH | OR (95% CI) | P-Value | Test |
|---|---|---|---|---|---|
| Female sex | 369 (59.9) | 4856 (48.5) | 1.59 (1.35 - 1.88) | 3.4 × 10-8 | Pearson χ2 |
| Firstborn | 227 (36.8) | 4294 (42.8) | 0.78 (0.66 - 0.92) | 3.5 × 10-3 | Pearson χ2 |
| Breech presentation | 36 (5.8) | 758 (7.6) | 0.76 (0.54 - 1.07) | 0.115 | Pearson χ2 |
| Oligohydramnios | 35 (5.7) | 94 (0.9) | 6.36 (4.28 - 9.46) | 1.6 × 10-25 | Pearson χ2 |
| Multiple gestation | 25 (4.1) | 12 (0.1) | 35.29 (17.64 - 70.59) | 7.0 × 10-23 | Fisher exact |
| Family history | 29 (4.7) | 9 (0.1) | 54.97 (25.90 - 116.66) | 6.9 × 10-29 | Fisher exact |
Abbreviation: DDH, developmental dysplasia of the hip; OR, odds ratio; CI, confidence interval.
a P-values reflect comparisons with the non DDH group (complete case denominators).
b Fisher’s exact test was used when any expected count < 5.
c Two-sided P < 0.05 considered significant.
Given the very small numbers of non-DDH infants with multiple gestation or a positive family history, these large ORs should be interpreted with caution. The multifactorial nature of DDH supports the role of targeted screening in high-risk populations.
5. Discussion
To the best of our knowledge, this study represents one of the largest single-province screening cohorts for DDH published in Turkey to date. With over 10,000 infants evaluated, our findings offer strong insight into the prevalence and risk factors associated with DDH and support the generalizability of previously reported national data.
In this province-wide universal screening cohort (n = 10,639), the incidence of DDH was 5.8%. In complete-case comparisons (Table 4), female sex was significantly associated with DDH (OR: 1.59, 95% CI: 1.35 - 1.88; P = 3.4 × 10-8), while primiparity was less frequent among DDH cases (OR: 0.78, 95% CI: 0.66 - 0.92; P = 3.5 × 10-3). Breech presentation was not significantly associated (OR: 0.76, 95% CI: 0.54 - 1.07; P = 0.115). By contrast, oligohydramnios (OR: 6.36, 95% CI: 4.28 - 9.46; P = 1.6 × 10-25), multiple gestation (OR: 35.29, 95% CI: 17.64 - 70.59; P = 7.0 × 10-23), and family history (OR: 54.97, 95% CI: 25.90 - 116.66; P = 6.9 × 10-29) showed strong positive associations with DDH. Given the very small numbers of non-DDH infants with multiple gestation or a positive family history, these large ORs should be interpreted with caution (potential under-recording outside the DDH group).
Reported DDH incidence in Turkey varies widely (0.3 - 17%), reflecting differences in sample size, screening timing, inclusion criteria, and operator experience (6-9). Examples include high incidence in small cohorts [e.g., 17% in 188 infants (6)] and lower rates in other regions or sampling frames [e.g., 0.3% in 258 infants (8)]. Our rate (5.8% from 10,639 infants) falls within this range and may be more representative at the population/program level due to the large denominator. From a public-health standpoint, national estimates suggest a substantial annual burden (4), underscoring the value of early detection programs.
Our findings confirm the well-described association between female sex and DDH in Turkish cohorts and elsewhere (10-12). Prior series have reported female predominance with varying magnitude (e.g., risk ratios from ~3.6:1 to higher) (10-12); our OR (1.59) likely reflects the influence of universal screening, which can attenuate relative differences observed in selective or clinic-based samples.
Two observations diverged from traditional teaching: We did not detect a positive association for breech (where many studies do report higher risk) (13); and primiparity showed an inverse association (whereas several reports — e.g., Aydin et al.— describe enrichment among cases) (14). These discrepancies may relate to local obstetric patterns, program-level follow-up of physiologically immature hips (Graf 2a), and/or differential documentation of perinatal factors in routine records (i.e., under-recording in non-DDH vs. DDH groups). In contrast, the strong association we observed for oligohydramnios is consistent with the mechanistic link of restricted fetal mobility documented previously (15). Likewise, the signal for family history accords with a heritable contribution to DDH susceptibility (16-21), though the effect size in our dataset was amplified by sparse non-DDH positives.
At the service-delivery level, these results argue for reinforcing structured capture of perinatal variables (family history, plurality, oligohydramnios) across all infants, not only those with abnormal sonography; periodic data-quality audits can reduce differential documentation. The high proportion managed non-operatively (93.7% Pavlik harness) supports the effectiveness of early detection and aligns with prior experience (6, 10). Maintaining recall pathways and standardized follow-up for Graf Type 2a hips remains critical to minimizing late-presenting DDH.
5.1. Conclusions
Province-wide universal infant hip US identified a 5.8% incidence of DDH and enabled timely, predominantly nonoperative management. These findings corroborate established risk factors and support ongoing program optimization, including comprehensive capture of perinatal variables to refine risk-stratified care.
While physical examination alone may fail to detect subtle cases of DDH, hip US using the Graf method enables timely and accurate diagnosis during the critical early postnatal period. Early identification allows for conservative management with a high success rate, primarily through non-invasive methods such as Pavlik harness application.
Delayed diagnosis, by contrast, may necessitate prolonged and more invasive treatment approaches, including surgical intervention. Such delays can lead to increased emotional stress for families, as well as long-term financial and functional burdens on healthcare systems and society as a whole.
Given these implications, DDH should be approached as a preventable public health concern. Healthcare professionals — especially family physicians, pediatricians, and orthopedic specialists — play a central role in the recognition of risk factors and the implementation of early screening protocols.
Overall, our findings reinforce the importance of maintaining and enhancing national-level ultrasound-based screening programs for DDH. Broader integration of standardized protocols and ongoing clinician training will contribute to improved musculoskeletal outcomes and quality of life in the pediatric population.
5.2. Limitations
This study has several limitations. First, its retrospective, registry-based design within a single province (rather than a national sample) may limit generalizability and does not allow causal inference. Second, completeness of several perinatal covariates was suboptimal: Family history, plurality (multiple gestation), oligohydramnios, and breech presentation were not uniformly recorded across all infants, and maternal infections (e.g., TORCH), medication exposures during pregnancy, and associated neonatal anomalies (e.g., torticollis, clubfoot) were not systematically captured. Consequently, comparative analyses used complete-case denominators, and some risk factors had very small non-DDH positive counts, leading to imprecision; Fisher’s exact test was applied when expected cell counts were < 5. Third, prenatal data on fetal presentation were not available for all pregnancies. Fourth, ultrasound examinations were performed in routine clinical care without centralized image review or interobserver-reliability assessment, and we did not evaluate newer or automated/AI-assisted diagnostic approaches. Finally, we did not assess radiographic confirmation or longer-term outcome.