1. Background
Obsessive-compulsive disorder (OCD) is a chronic psychiatric condition characterized by intrusive thoughts and repetitive behaviors aimed at alleviating anxiety. While its psychological and neurobiological mechanisms have been extensively studied, less is known about its potential influence on urinary habits (1, 2). Emerging evidence suggests that psychiatric disorders may influence bladder function through behavioral, neurological, and autonomic pathways, yet the association between OCD and voiding patterns remains largely unexplored (3, 4).
Infrequent voiding, defined as urinating fewer than three times per day, is a common urinary habit observed in children and adolescents and may be associated with various behavioral and psychological factors (1, 5). It is associated with increased bladder capacity, incomplete emptying, and heightened risk of urinary tract complications (4). Although the phenomenon has been primarily investigated in pediatric populations and individuals with neurogenic bladder, adult presentations linked to psychiatric conditions remain poorly characterized (3).
Previous research has shown a high prevalence of bowel and bladder dysfunction among children with OCD, particularly linked to compulsive behaviors and emotional comorbidities (6). Adult studies similarly report increased odds of OCD in patients with overactive bladder and other lower urinary tract symptoms (LUTS) (4), suggesting that OCD can influence bladder function. Unlike prior studies, which focused mainly on urgency, incontinence, or adult populations, our study specifically examined infrequent voiding in children and found that those with infrequent voiding exhibited significantly higher OCD symptom severity. These findings provide direct evidence that OCD may contribute to infrequent voiding, highlighting a relatively underexplored aspect of pediatric bladder dysfunction.
Understanding the relationship between OCD and infrequent voiding is clinically significant, as altered micturition may predispose individuals to urinary stasis, infections, and decreased quality of life. Furthermore, elucidating this association could provide insight into the broader psychosomatic impact of OCD, highlighting the need for integrated psychiatric and urological assessment (7).
2. Objectives
The present study aims to investigate the potential link between OCD severity and infrequent voiding, thereby providing insights into the behavioral manifestations of OCD, specifically its association with urinary habits.
3. Methods
3.1. Study Design and Setting
This case-control study was conducted at the Pediatric Clinic of Amir Kabir Hospital, Arak, Iran, between 2012 and 2013. The study included girls aged 5 - 17 years with infrequent voiding and an age- and demographically-matched control group without infrequent voiding. In this study, infrequent voiding was operationally defined as voiding fewer than 3 times during waking hours per 24-hour period, based on commonly used pediatric bladder function criteria. Participants were recruited via convenience sampling, with controls matched to cases by age (±1 year) and demographics. The sample size was 76 per group (total 152), based on the FOA Children’s Obsessive-Compulsive Questionnaire (FOA-COCQ)’s validated age range (5 - 17 years). Only girls were included to reduce heterogeneity, as urinary behavior and OCD symptom presentation differ by gender.
3.2. Sample Size
The sample size was calculated for a two-sided test comparing two independent groups (cases and controls) with α = 0.05 and 80% power (β = 0.20). Based on prior studies reporting a ~25% difference in moderate to severe OCD prevalence among pediatric populations (8), 76 participants per group (total 152 girls) were required to detect significant differences in FOA-COCQ scores and odds ratios (ORs).
3.3. Inclusion and Exclusion Criteria
The inclusion criteria encompassed girls aged 5 - 17 years diagnosed with infrequent voiding, without congenital or structural anomalies of the kidneys or urinary tract, chronic medical conditions, neurological or psychiatric disorders, or intellectual disability. Participants were additionally screened for common behavioral or psychological comorbidities — such as constipation (Rome III criteria), anxiety disorders, and attention-deficit/hyperactivity disorder (ADHD) — through clinical interview and medical record review. Only girls without these comorbidities and with parental consent were included, ensuring that observed associations reflected OCD-related mechanisms rather than secondary effects of other conditions.
Exclusion criteria included structural abnormalities of the kidneys or urinary tract, chronic medical conditions, lack of parental consent, and clinically diagnosed constipation, anxiety disorders, ADHD, or other psychiatric or behavioral comorbidities, as these could influence both infrequent voiding and OCD symptoms.
3.4. Assessment of Obsessive-Compulsive Disorder
Obsessive-compulsive disorder symptoms were assessed using the FOA-COCQ, developed by FOA et al. in 2010, which is based on adult versions of the FOA Questionnaire (1998, 2002) and designed for children aged 5 - 17 years. The questionnaire consists of 21 items across six subscales: Doubting and checking (5 items), obsessive thoughts (4 items), hoarding (3 items), washing (3 items), ordering (3 items), and neutralizing (3 items).
Items are rated on a 3-point Likert scale (0 = never, 1 = sometimes, 2 = always), yielding total scores from 0 to 42, with higher scores indicating greater OCD severity (0 - 10: none; 11 - 20: mild; 21 - 30: moderate; 31 - 42: severe). The FOA-COCQ demonstrates good reliability (Cronbach’s α = 0.85; test-retest = 0.77), with subscale reliabilities of 0.81 - 0.88 (internal consistency) and 0.68 - 0.89 (test-retest), and has established concurrent and discriminant validity.
To ensure cultural and linguistic appropriateness, the FOA-COCQ was translated into Persian using standard forward-backward translation by two bilingual experts, with discrepancies resolved by a third reviewer. A pilot study in 30 Iranian girls aged 5 - 17 years demonstrated good internal consistency (Cronbach’s α = 0.83; subscales 0.78 - 0.87) and acceptable test-retest reliability (ICC = 0.75). Confirmatory factor analysis supported the original six-factor structure (CFI = 0.92, RMSEA = 0.07), indicating that the Persian FOA-COCQ is reliable and valid for Iranian children. To confirm OCD diagnosis, children who screened positive on the FOA Questionnaire were referred to a supervising psychiatrist for a structured interview based on DSM-IV-TR criteria.
3.5. Cultural Adaptation and Validation
The FOA-COCQ was translated into Persian using a standard forward-backward translation process. Two bilingual experts independently translated the original English questionnaire into Persian, and a third expert back-translated it into English. Discrepancies were resolved by consensus.
A pilot validation study on 30 Iranian girls aged 5 - 17 years demonstrated good internal consistency (Cronbach’s alpha = 0.83 total; subscales 0.78 - 0.87) and acceptable test-retest reliability (ICC = 0.75). Confirmatory factor analysis supported the original six-factor structure (CFI = 0.92, RMSEA = 0.07), indicating the Persian version is reliable and valid.
3.6. Data Collection
Data were collected using structured methods to ensure consistency. Demographic information (age, grade, and relevant characteristics) and clinical history were obtained from medical records. Urinary behavior was assessed via clinical interviews with participants and parents. Obsessive-compulsive symptoms were measured using the Persian FOA-COCQ, recording total and subscale scores for each participant. All data were entered into a structured database for analysis.
3.7. Statistical Analysis
Descriptive Statistics: Participant characteristics, including age, demographic variables, and FOA-COCQ scores, were summarized using means ± standard deviations (SD), medians, ranges, and frequencies (%), as appropriate. The Shapiro-Wilk test was used to assess normality of continuous variables. Because most variables were non-normally distributed, non-parametric methods were applied for group comparisons.
Group comparisons: Differences between girls with infrequent voiding (cases) and healthy controls were assessed using the Mann-Whitney U test for continuous variables (e.g., FOA total scores, subscale scores) and chi-square tests for categorical variables (e.g., OCD severity categories: none, mild, moderate, severe).
Controlling for confounding: To estimate the association between infrequent voiding and OCD severity while controlling for potential confounders, binary logistic regression was performed. In this model, infrequent voiding status (case vs. control) was the dependent variable, and OCD severity categories (FOA-COCQ total score: none, mild, moderate, severe) were the primary independent variable. Age and other demographic variables were included as covariates to adjust for potential confounding effects.
Subgroup analyses: To further explore the relationship, subgroup analyses were conducted within each OCD severity category to examine whether the odds of infrequent voiding differed across severity levels. Odds ratios with 95% CIs were reported for all regression analyses.
Effect size and power: The sample size (76 per group, total 152) was calculated to detect a clinically meaningful difference in moderate-to-severe OCD symptom prevalence between cases and controls, with 80% power and a significance level of α = 0.05, based on prior pediatric OCD studies.
Software and significance: All statistical analyses were conducted using IBM SPSS Statistics, Version 26.0. A two-sided P-value < 0.05 was considered statistically significant.
3.8. Ethical Considerations
Informed consent was obtained from parents or legal guardians for girls under 12 years, and from both participants and parents for those aged 12 years and older. The study adhered to the Declaration of Helsinki and the ethical guidelines of the Research Ethics Committee of Arak University of Medical Sciences (Ethical code: IR.ARAKMU.REC.92.148.5).
4. Results
4.1. Demographic Characteristics
A total of 152 cases participated in the study, including 76 children diagnosed with infrequent voiding and 76 healthy controls. The normality of age data was assessed using the Shapiro-Wilk test and indicated a non-normal distribution (P < 0.05), so age comparisons were performed using the Mann-Whitney U test. The mean age in the case group was 8.13 ± 1.39 years, while the mean age in the control group was 8.19 ± 2.03 years (P = 0.816, Mann - Whitney U) (Table 1). No statistically significant difference in age was observed between the groups, confirming proper matching of participants.
Abbreviation: OCD: obsessive-compulsive disorder
a Values are expresses as mean ± SD.
b Girls diagnosed with infrequent voiding and positive for obsessive-compulsive symptoms.
c Age- and demographically-matched girls without infrequent voiding.
4.2. FOA Total Scores
FOA total scores were also tested for normality using the Shapiro-Wilk test, and data were found to be non-normally distributed (P < 0.05). Consequently, group comparisons were conducted using the Mann-Whitney U test. Total FOA scores indicated a significantly higher prevalence of OCD among children with infrequent voiding. In the case group, 32 children (42.1%) had no OCD, 24 (31.6%) had mild symptoms, 20 (26.3%) had moderate symptoms, and none exhibited severe symptoms. In the control group, 40 children (52.6%) had no OCD, 34 (44.7%) had mild symptoms, and only 2 children (2.6%) had moderate or severe symptoms (P = 0.001, chi-square test) (Table 2).
a Values are expresses as N (%).
b The table shows the frequency and percentage of girls in each FOA-COCQ severity category in the case and control groups.
c None, mild, moderate, severe: Levels of OCD symptom severity according to FOA-COCQ total score: 0 - 10 (none), 11 - 20 (mild), 21 - 30 (moderate), 31 - 42 (severe).
d FOA: FOA Children’s Obsessive-Compulsive Questionnaire.
All children who scored in the mild, moderate, or severe range on the FOA-COCQ (n = 80) were referred for a structured DSM-IV-TR psychiatric interview by a supervising psychiatrist. Of these, 38 children in the case group and 2 children in the control group were confirmed to meet DSM-IV-TR criteria for OCD. No participants were excluded after the psychiatric evaluation.
4.3. FOA Subscale Scores
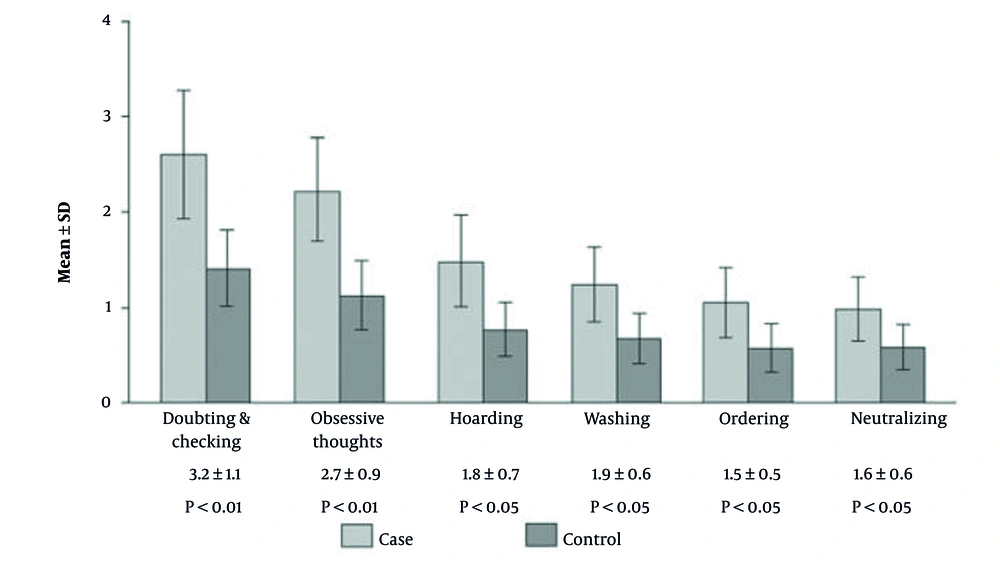
Subscale scores were also non-normally distributed (Shapiro-Wilk P < 0.05), so Mann-Whitney U tests were used for comparisons. The mean scores (± SD) for each OCD subscale in both the case and control groups are presented. The case group exhibited significantly higher mean scores across all subscales compared to controls. The largest differences were observed for doubting and checking (3.2 ± 1.1 vs. 1.8 ± 0.9; P < 0.01) and obsessive thoughts (2.7 ± 0.9 vs. 1.5 ± 0.7; P < 0.01). Significant but smaller differences were also found for hoarding, washing, ordering, and neutralizing (all P < 0.05), indicating that individuals in the case group experienced more severe symptoms across all dimensions of obsessive-compulsive tendencies (Table 3 and Figure 1).
| Subscale | Case | Control | P-Value c |
|---|---|---|---|
| Doubting and checking | 3.2 ± 1.1 | 1.8 ± 0.9 | < 0.01 |
| Obsessive thoughts | 2.7 ± 0.9 | 1.5 ± 0.7 | < 0.01 |
| Hoarding | 1.8 ± 0.7 | 0.9 ± 0.5 | < 0.05 |
| Washing | 1.9 ± 0.6 | 1.2 ± 0.5 | < 0.05 |
| Ordering | 1.5 ± 0.5 | 1.0 ± 0.4 | < 0.05 |
| Neutralizing | 1.6 ± 0.6 | 1.0 ± 0.5 | < 0.05 |
a Values are expressed as mean score ± SD
b Scores are based on the FOA Children’s Obsessive-Compulsive Questionnaire subscales.
c Statistical significance of difference between case and control groups using Mann-Whitney U test. Higher scores indicate more severe symptoms.
Analysis of the Six FOA subscales revealed significantly higher scores in children with infrequent voiding across all domains bar chart comparing the mean FOA Children’s Obsessive-Compulsive Questionnaire (FOA-COCQ) subscale scores between girls with infrequent voiding (case) and healthy controls. FOA Children’s Obsessive-Compulsive Questionnaire subscales: doubting and checking, obsessive thoughts, hoarding, washing, ordering, neutralizing. Error bars: Standard deviation. Higher scores indicate greater severity of obsessive-compulsive symptoms.
4.4. Multiple Logistic Regression Analysis
To account for potential confounding, a multiple logistic regression model was performed with infrequent voiding as the dependent variable and OCD severity as the primary independent variable, adjusting for age.
Adjusted Odds Ratios (AORs) indicated that girls with moderate OCD were 3.0 times more likely to have infrequent voiding compared to girls without OCD (AOR = 3.0; 95% CI: 1.5 - 5.8; P = 0.002).
Girls with severe OCD (n = 1 in controls) could not be reliably analyzed due to small numbers, but were included in descriptive analyses.
No significant association was observed for mild OCD after adjustment (AOR = 1.3; 95% CI: 0.7 - 2.3; P = 0.42).
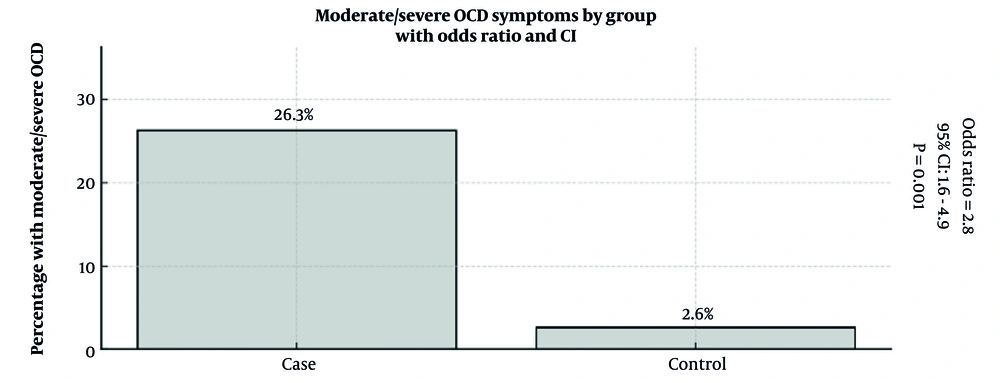
4.5. Odds Ratio Analysis
Binary logistic regression was performed to estimate the odds of infrequent voiding according to OCD severity. Children with moderate OCD symptoms had a significantly higher odds of infrequent voiding compared to children with no OCD (OR = 3.1; 95% CI: 1.5 - 6.4; P = 0.002). Girls with mild OCD showed a non-significant trend toward increased odds (OR = 1.4; 95% CI: 0.7 - 2.8; P = 0.33).
Subgroup analysis by OCD severity showed a progressive increase in the prevalence of infrequent voiding: 10% in children with no OCD, 21% in mild OCD, and 45% in moderate OCD. No participants had severe OCD. These results support a dose-response relationship between OCD symptom severity and the likelihood of infrequent voiding.
To assess the strength of association between infrequent voiding and OCD, ORs were calculated. Girls with moderate OCD symptoms had an adjusted odds ratio (AOR) of 3.0 (95% CI: 1.5 - 5.8; P = 0.002) for exhibiting infrequent voiding compared to girls without OCD, after adjusting for age. This indicates that, independent of age, moderate OCD severity is significantly associated with higher odds of infrequent voiding (Table 4 and Figure 2).
| Group | Moderate/Severe OCD | OR | 95% CI | P-Value |
|---|---|---|---|---|
| Case | 20 | 2.8 | 1.6–4.9 | 0.001 |
| Control | 2 | - | - | - |
Abbreviations: OCD, obsessive-compulsive disorder; OR, odds ratio; CI, confidence interval.
a The table shows the odds of having moderate-to-severe obsessive-compulsive disorder symptoms in girls with infrequent voiding compared to controls.
The strength of association between infrequent voiding and moderate to severe obsessive-compulsive disorder symptoms was evaluated using ORs. An OR > 1 indicates higher odds of moderate-to-severe obsessive-compulsive disorder symptoms in the case group. (Abbreviations: OR, Odds ratio from binary logistic regression; 95% CI, 95% confidence interval).
5. Discussion
This study focused exclusively on female participants to reduce heterogeneity. Urinary habits and voiding patterns differ between boys and girls, and OCD prevalence and symptom presentation may also vary by gender. Restricting the sample to girls allowed us to better isolate the association between OCD severity and infrequent voiding. Future studies should examine whether similar associations occur in boys to assess generalizability.
The FOA-COCQ was chosen for its age-appropriate design (5 - 17 years), comprehensive coverage of six OCD domains (doubting and checking, obsessive thoughts, hoarding, washing, ordering, neutralizing), and strong psychometric properties. As a self-report tool, it is practical for larger samples and repeated measures, facilitating reliable assessment of OCD symptoms.
Our findings align with prior research linking OCD and somatic behaviors in children. Girls with infrequent voiding had higher FOA total and subscale scores, and moderate OCD symptoms were more prevalent in the case group. Logistic regression confirmed that moderate OCD severity was associated with higher odds of infrequent voiding, suggesting a dose-response relationship.
Overall, the study emphasizes the importance of assessing obsessive-compulsive symptoms in pediatric patients with infrequent voiding and demonstrates methodological rigor through the use of a validated instrument and a homogenous study population.
Research exploring the association between infrequent voiding and OCD remains limited. Existing studies have identified links between infrequent voiding and various psychiatric conditions, including anxiety disorders (8), as well as psychological stress (6). Notably, one investigation reported that individuals with infrequent voiding exhibited significantly higher anxiety scores compared to control participants (8).
Previous research has demonstrated associations between LUTS and OCD in various populations. For instance, in adult women, persistent LUTS correlated with heightened OCD risk, particularly bladder outlet obstruction (OR 4.43) (4). Pediatric case series also document children initially treated for urological symptoms who were subsequently diagnosed with OCD, revealing underlying obsessive fears around incontinence and resultant voiding behaviors (7). Furthermore, behavioral treatment of OCD in children has been shown to resolve concurrent voiding dysfunction (9).
The elevated FOA subscale scores across domains suggest that children with infrequent voiding may exhibit comprehensive obsessive - compulsive traits. This aligns with studies reporting comorbidity of bowel and bladder dysfunction in children receiving evaluation for OCD, where more than 30% screened positive for significant bowel and bladder dysfunction symptoms, with a higher prevalence in females (10).
Studies involving adults, particularly women, with overactive bladder suggest that there may be a connection between bladder dysfunction and obsessive-compulsive tendencies (11). For instance, women with overactive bladder were found to exhibit higher levels of obsessive behaviors, such as repetitive checking, compared to controls. These findings highlight the potential interplay between urinary disorders and psychiatric symptoms. In adults, particularly women, overactive bladder has been examined in relation to obsessive-compulsive symptoms. Evidence indicates that women experiencing overactive bladder report higher levels of obsessive behaviors, such as repeated checking, compared to individuals without overactive bladder (12). The severity of these obsessive traits appears to correlate with the intensity of overactive bladder symptoms, implying that urinary disorders may be accompanied by certain psychiatric tendencies (13).
Further research focusing on chronic LUTS has shown that individuals with OCD may experience more voiding phase problems, implying a possible association between certain urinary abnormalities and obsessive-compulsive behaviors (14). These findings suggest that clinicians should consider evaluating psychiatric symptoms when managing patients with LUTS (10). Further studies investigating chronic LUTS have noted that individuals with OCD tend to experience more voiding phase difficulties than those without OCD. These findings suggest a possible association between urinary dysfunction and obsessive-compulsive behaviors, indicating that psychological assessment may be valuable when treating patients with LUTS (4).
In pediatric populations, bladder and bowel dysfunction often co-occur, with overactive bladder being the most frequently reported condition. Overactive bladder is characterized by urgency and increased voiding frequency, sometimes accompanied by incontinence, and may be associated with behavioral and psychological issues (9). Bladder and bowel dysfunction frequently co-occur in pediatric populations, with overactive bladder being the most commonly reported urinary condition (7).
Several neurobiological mechanisms may explain the association between obsessive-compulsive symptoms and infrequent voiding in girls. Stress-related neuropeptides, such as corticotropin-releasing factor in Barrington’s nucleus, can modulate bladder function, with elevated corticotropin-releasing factor leading to urinary retention in animal studies (13, 14). Human neuroimaging shows that brain regions including the anterior cingulate cortex, medial prefrontal cortex, insula, and periaqueductal gray control voiding timing and appropriateness (14). In OCD, abnormal cortico-striatal-thalamic-cortical activity may disrupt inhibitory control over these pathways, resulting in voluntary urinary withholding, which may explain the higher prevalence of infrequent voiding in girls with elevated OCD severity.
The findings should be interpreted cautiously. The study included only girls aged 5 - 17 years from a single pediatric clinic in Arak, Iran, using a convenience sample, limiting generalizability to boys, younger children, or other settings. Cultural, environmental, and healthcare differences may further restrict extrapolation.
Other limitations include the cross-sectional, case-control design, which precludes causal inferences, and unmeasured confounders such as parental education, occupation, socioeconomic status, and comorbidities like anxiety, ADHD, or constipation.
Future studies should use larger, more diverse populations and longitudinal designs to clarify the relationship between infrequent voiding and OCD symptoms. Exploring underlying neurobiological, psychological, and environmental mechanisms may further explain this association. Research could also assess early interventions for girls with both urinary irregularities and OCD traits, and examine gender, age-specific patterns, and co-occurring conditions to inform targeted prevention and treatment strategies.
5.1. Conclusions
Infrequent voiding in children may serve as an important behavioral marker for identifying those at increased risk of obsessive-compulsive tendencies. Clinicians and caregivers should monitor urinary habits as part of routine pediatric assessments, particularly in children who exhibit signs of compulsive or anxiety-related behaviors. Early recognition of infrequent voiding can facilitate timely psychological evaluation and intervention, including behavioral strategies or therapy aimed at managing obsessive-compulsive symptoms. Future research and clinical practice should consider integrating urinary behavior monitoring into comprehensive child mental health assessments to support prevention and early intervention strategies.