Dear Editor,
In an era marked by rapid epidemiological transitions and systemic challenges, the concept of the “triple burden of disease” — encompassing communicable diseases, non-communicable diseases (NCDs), and diseases linked to environmental and social change — demands renewed attention (1). While originally applied to low- and middle-income countries, this framework is increasingly relevant across all health systems globally. The burden now strains multidisciplinary healthcare teams who are at the frontline of navigating complexity and inequity.
Understanding the Triple Burden in a Globalized Context
The triple burden of disease — communicable diseases, NCDs, and environmental challenges — places increasing pressure on global health systems (1). Alongside infectious diseases like tuberculosis and HIV/AIDS, NCDs such as heart disease, diabetes, cancer, and psychiatric disorders (e.g., depression, anxiety) are rising (2). Climate change adds further strain, contributing to both physical illness and mental health impacts, including grief, trauma, and anxiety (3). These burdens often intersect, particularly in vulnerable populations with limited access to healthcare. For example, disaster-affected communities may face gaps in both chronic and mental health care. Addressing these interconnected threats requires integrated, multidisciplinary strategies that promote equitable, person-centered, and holistic health responses.
Multidisciplinary Collaboration as a Critical Strategy
Effectively addressing the triple burden of disease requires collaboration across disciplines and systems (1). Physicians, nurses, midwives, public health practitioners, mental health professionals, and environmental experts must work together to deliver integrated care. Nurses and midwives serve as vital links between clinical systems and communities, especially in disaster-prone or underserved areas (4). Public health teams contribute by addressing social determinants and promoting mental health. Importantly, training primary care providers in psychological first aid enhances preparedness and response to climate-related trauma (2), as well as in conflict and war-related disasters where psychological needs are immediate and pervasive (5). Multidisciplinary teams that emphasize task-sharing, mental health integration, and culturally responsive care have demonstrated improved outcomes in chronic disease management, disaster recovery, and mental health service delivery (6).
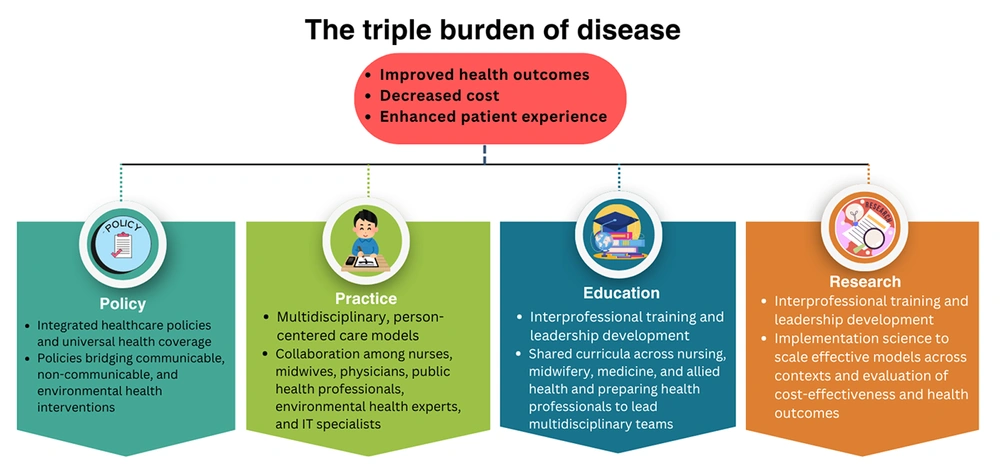
As shown in Figure 1, tackling the triple burden of disease requires coordinated action across four interconnected domains — policy, practice, education, and research. Policies that integrate communicable, non-communicable, mental health, and environmental health priorities set the foundation for equitable access to care. In practice, multidisciplinary, person-centered models bring together diverse professionals to deliver comprehensive services. Education builds interprofessional skills and leadership capacity, while research ensures that interventions are evidence-based, scalable, and responsive to emerging challenges. Collectively, these strategies drive improved health outcomes, lower costs, and enhance patient experiences.
Strengthening Systems Through Education and Policy
Strengthening health systems requires strategic investment in both education and policy reform. Educational curricula should promote interprofessional collaboration, systems thinking, and mental health integration across clinical and public health training. Training primary care providers to screen for depression and anxiety, offer psychological first aid, and respond effectively in crisis situations is critical — especially in disaster-prone and low-resource settings. Continuing education must address innovations like telehealth and climate-resilient care delivery. Policymakers should prioritize universal health coverage, mental health integration, and nurse-led models (4). Embedding mental health into primary care fosters person-centered, equitable systems that serve diverse and vulnerable populations (7).
Ethical Deployment of Technology
Technology can enhance access to care, coordination, and mental health support through tools such as telehealth and electronic health records. However, it may also widen disparities in underserved communities due to digital illiteracy and limited infrastructure. Ethical deployment requires balancing innovation with equity — ensuring data privacy, informed consent, and accessibility (8). Mental health tools, including remote counseling and screening, should be culturally appropriate and integrated into primary care. Multidisciplinary teams must assess technology's impact on vulnerable populations to promote just, person-centered care.
Planetary Health and Environmental Justice
Environmental threats like climate change and pollution impact both physical and mental health, increasing risks of anxiety, trauma, and displacement-related stress. Healthcare systems must adopt sustainable practices and integrate mental health into climate resilience efforts (9). Nurses can lead by incorporating environmental and psychosocial screening, supporting affected communities, and promoting climate-conscious, trauma-informed care.
Key Principles and Strategies of the Triple Burden of Disease Management
Clinical Practice
Integrated clinical practice should address coexisting communicable, non-communicable, and mental health conditions. Primary care providers play a key role in early detection through joint screening for chronic illnesses and psychiatric disorders. Multidisciplinary teams — including nurses, midwives, and mental health professionals — are essential for delivering person-centered care (4). Psychological first aid equips providers to support those affected by climate-related or conflict-related trauma (5). Evidence-based protocols, digital tools like telehealth, and continuing education improve care quality and continuity (10), especially in low-resource or disaster-prone settings (11).
Public Health Prevention
Public health strategies must address infectious, chronic, and mental health conditions simultaneously (12). This includes sustaining high vaccination coverage, promoting healthy lifestyles, and implementing tobacco and alcohol control (13). Community health workers can provide culturally relevant education and identify psychosocial needs, especially after climate-related events. Integrated surveillance systems should monitor disease trends and mental health impacts (14). Mental health promotion — through stigma reduction, early screening, and community resilience programs — is essential. Collaborations across sectors, including One Health approaches, can strengthen capacity to respond to environmental, zoonotic, and behavioral health challenges (15).
Health Policy and Systems
Health policy strategies to address the triple burden of disease should prioritize universal health coverage, ensuring equitable access to essential services without financial hardship (7). Achieving this requires robust primary health care systems, the expansion of rural clinics, and the full integration of communicable, non-communicable, and mental health services. Investments in system capacity, mental health workforce development, and fair resource distribution are critical. Public health laws — such as tobacco taxation, alcohol regulation, and advertising restrictions — must be reinforced by policies promoting early detection and psychological support. Integrating climate resilience and mental health into national planning and international cooperation is vital for achieving sustainable development goals.
Conclusions
The triple burden of disease is a complex public health challenge requiring integrated, multidisciplinary responses. Addressing communicable, non-communicable, and environmental health threats must include mental health as a core component — particularly given rising psychiatric disorders and climate-related trauma. Frontline healthcare providers are essential in delivering person-centered, trauma-informed care. Achieving resilient, equitable health systems demands sustained investment, policy reform, and interprofessional collaboration that bridges physical and mental health services, advances community engagement, and supports population well-being across diverse and vulnerable contexts.