1. Background
Choosing a preferred method of delivery is a crucial decision made prior to labor, as it significantly impacts the health of both the mother and the newborn. Childbirth generally occurs through one of three main approaches: Vaginal delivery (VD), assisted VD, and cesarean section (CS). Assisted VD — also known as operative VD — includes techniques such as vacuum extraction and the use of forceps (1). Reports of severe complications, such as subgaleal hematoma and intracranial hemorrhage associated with operative VD, have led to a decline in the use of this method in the USA and worldwide (2). The VD — also referred to as natural or normal delivery — is a less medically interventionist approach to childbirth (3). Selecting the method of childbirth is a vital decision that has a profound impact on both maternal and neonatal health outcomes. The VD, especially in full-term pregnancies, is typically viewed as the safest and least invasive option, associated with the lowest rates of mortality and complications for both mother and baby. However, the global prevalence of CS has risen steadily in recent decades, prompting concerns about its potential overuse, related health risks, and the financial burden it places on healthcare systems (4).
Although VD is often the safest approach, certain maternal or fetal complications arising before or during labor may require alternative methods. The CS is one such option — a surgical procedure that involves incisions in both the abdomen (laparotomy) and uterus (hysterotomy) to deliver the baby. While insufficient use of CS has been associated with higher rates of maternal and perinatal mortality and morbidity, excessive reliance on the procedure has not demonstrated added benefits and may, in fact, pose additional risks (5). Since 1985, the World Health Organization (WHO) has recommended an ideal national CS rate of 10% to 15%, regardless of the region (6). Initiatives aimed at curbing the overuse of SCs have included changes to hospital policies and culture, efforts to reshape healthcare providers’ attitudes and practices, and educational campaigns to inform women about the advantages of vaginal birth. Despite these strategies, success has been limited. For instance, in the United States, the rate of cesarean deliveries increased from 26.1% in 2002 to roughly 31 - 32% by 2019 (7, 8). This global pattern is not confined to the United States; rising CS rates are evident worldwide. Generally, CS incidence tends to be higher in developed nations compared to developing regions. For example, rates range from as low as 2% in parts of Africa to as high as 50 - 60% in the Dominican Republic and certain areas of Latin America (9).
A wide range of studies from various countries, including Iran, have examined the sociodemographic and clinical determinants influencing CS preference. Frequently cited predictors include maternal age, educational attainment, urban residency, and obstetric history. In Iran, smaller-scale investigations have identified links between CS preference and factors such as higher maternal education, first-time pregnancy (primiparity), and physician recommendations. However, many of these studies were confined to specific hospitals or regions and often involved limited sample sizes, restricting their generalizability.
Despite the substantial body of research, Iran lacks large-scale, nationwide, population-based studies that simultaneously assess a broad spectrum of maternal, neonatal, and contextual variables. Most existing studies either fall short of national representation or do not employ multivariate analyses capable of disentangling the independent effects of each factor. Furthermore, there is limited evidence on how combinations of variables — such as maternal education and geographic location — interact to shape delivery method preferences.
The present study addresses these gaps by analyzing data from nearly 1.5 million births registered in Iran between April 2015 and April 2016. This represents one of the largest population-based analyses on this topic both nationally and internationally. The innovation of this study lies in:
- Its national scope, using data from the Iranian birth registration system
- Its multidimensional analysis incorporating both maternal and neonatal factors through advanced multivariate logistic regression modeling
- Its ability to stratify CS preferences by detailed educational levels (including mothers holding a doctoral degree), gestational age, and rural vs. urban residence
2. Objectives
The present study aimed to examine the influence of various sociodemographic factors on the preference for CS as a mode of delivery among pregnant women.
3. Methods
3.1. Design and Participants
The present study aimed to examine delivery methods and their associated factors among pregnant women in Iran. To achieve this, we conducted a retrospective, census-based analysis using national maternal and neonatal data from the Iranian birth registration system, covering the period from April 2015 to April 2016. The study included all live births recorded during this timeframe, while deliveries resulting in stillbirth were excluded. Due to the population-wide scope of the dataset, no sample size calculation was necessary. Data were collected from all provinces across the country.
Maternal demographic variables assessed included age, educational attainment, place of residence, consanguinity, and medical history (including diabetes, hypertension, heart disease, anemia, and preeclampsia). Obstetric factors such as gravidity, abortion history, number of abortions, and delivery method were also evaluated. Neonatal characteristics analyzed comprised birth weight, gestational age, and sex.
3.2. Statistical Analysis
This retrospective descriptive study examined and compared mothers and neonates who underwent CS or VD, using key sociodemographic variables previously identified. A logistic regression model was employed to assess the influence of these factors on delivery method preference and to explore their interrelationships. Data analysis was conducted using SPSS version 23.
The chi-square test was applied to evaluate associations between delivery type and variables such as parental occupation, education level, and place of residence. Multivariate analysis was performed using logistic regression to identify factors independently associated with delivery method. Initially, univariate analysis was used to detect statistically significant variables, which were then included as independent predictors in the multivariate model. The dependent variable was mode of delivery, categorized as CS or VD, with a significance threshold set at P < 0.05 for all univariate tests.
To ensure a comprehensive understanding of childbirth experiences, the study included women regardless of their delivery history — encompassing both first-time mothers and those with prior CS or VD. This inclusive design supports the development of targeted interventions that reflect the diverse needs, preferences, and cultural beliefs of women across different childbirth scenarios.
4. Results
Based on data from Civil Registry Organization, a total of 1,528,053 births were documented in Iran between April 2015 and April 2016. After excluding 36,170 cases due to home births or incomplete records, the final study population included 1,491,883 women. Among these, 49.9% delivered via CS, while 50.1% underwent VD. As shown in Table 1, there was a negative correlation between maternal age and the selection of VD. As the mother’s age increased, the odds of choosing CS decreased by 15.5% (P < 0.05). Delivery type was also found to be significantly associated with educational attainment. Women with higher levels of education were more chance to undergo CS. Notably, for each incremental increase in educational level, the odds of electing a CS rose substantially (P < 0.05). “For example, mothers holding a doctoral degree were 6.57 times more chance to choose a CS compared to those who were illiterate (odds ratio = 6.57; 95% confidence interval: 6.34 - 6.08). On the other side, the demographic characteristics are presented in Table 1.
| Variables | No. (%) |
|---|---|
| Mothers’ age (y) | 28.97 ± 5.94 (29, 25.33) b |
| < 20 | 97005 (6.50) |
| 20 - 25 | 324562 (21.75) |
| 25 - 30 | 465806 (31.23) |
| 30 - 35 | 382500 (25.64) |
| 35 - 40 | 176327 (11.82) |
| 40 - 45 | 40027 (2.68) |
| 45 - 50 | 5047 (0.34) |
| Missing | 609 (0.04) |
| Mothers' educational level | |
| Elementary | 284006 (19) |
| Middle | 347168 (23) |
| High | 433252 (29) |
| Graduate-master | 340572 (23) |
| PhD | 4460 (0.003) |
| Missing | 82425 (6) |
| Living place | |
| Rural | 371006 (25) |
| Urban | 1120877 (75) |
| Delivery type | |
| CS | 744217 (49.88) |
| Vaginal | 747317 (50.1) |
| Missing | 349 (0.02) |
| Parental relativity | |
| Yes | 316672 (21) |
| No | 1175211 (79) |
| Gender | |
| Male | 768782 (52) |
| Female | 722416 (48) |
| Bisexual | 685 (0.1) |
| GA (wk) | 38.34 ± 1.99 (39, 38.39) b |
| < 28 | 10657 (0.71) |
| 28 - 32 | 11284 (0.75) |
| 33 -37 | 92218 (6.2) |
| > 37 | 1377411 (92.32) |
| Missing | 295 (0.02) |
| BW (g) | 3156.98 ± 535.27 (3200, 2900.3500) b |
| < 1000 | 11552 (0.78) |
| 1000 - 1500 | 8732 (0.0.59) |
| 1500 - 2500 | 85400 (5.72) |
| > 2500 | 1385953 (92.89) |
| Missing | 246 (0.02) |
Abbreviation: CS, cesarean section; GA, gestational age; BW, birth weight.
a Values are expressed as No. (%) or mean ± SD.
b Numeric variables are expressed as mean ± SD.
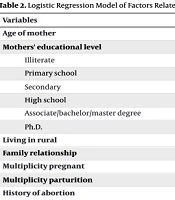
Our findings indicated that women residing in rural areas had approximately half the odds of undergoing CS compared to their urban counterparts, a difference that was statistically significant (P = 0.01). Logistic regression analysis further revealed that neonatal complications such as asphyxia (OR = 0.808; 95% CI: 0.656 - 0.995) and the need for resuscitation (OR = 0.684; 95% CI: 0.676 - 0.692) occurred less frequently among CS deliveries. Conversely, Apgar scores at one minute were higher in neonates delivered via CS (OR = 1.06; 95% CI: 1.055 - 1.064). However, certain neonatal complications were more prevalent following CS, including respiratory distress syndrome (RDS) (OR = 1.64; 95% CI: 1.25 - 2.17), meconium aspiration syndrome (OR = 5.47; 95% CI: 2.29 - 13.07), and air leak syndrome (OR = 1.67; 95% CI: 0.397 - 6.94). Additionally, maternal pregnancy complications were associated with a reduced chance of CS delivery. Multivariable analysis (Table 2) demonstrated a statistically significant decrease in the odds of undergoing CS at lower gestational ages, particularly in pregnancies less than 28 weeks (OR = 3.98; 95% CI: 3.794 - 4.176).
| Variables | B | SE | Wald | P-Value | Odds Ratio | CI |
|---|---|---|---|---|---|---|
| Age of mother | -0.17 | 0.03 | 40.77 | 0.000 | 0.85 | 0.80 - 0.89 |
| Mothers' educational level | -0.28 | 0.01 | 37417 | 0.000 | 0.76 | 0.76 - 0.77 |
| Illiterate | -1.04 | 0.04 | 13.9 | 0.000 | 0.87 | 0.80 - 0.94 |
| Primary school | 0.43 | 0.02 | 689.12 | 0.000 | 1.54 | 1.49 - 1.59 |
| Secondary | 0.97 | 0.02 | 3550 | 0.000 | 2.63 | 2.55 - 2.75 |
| High school | 1.38 | 0.02 | 7097 | 0.000 | 3.99 | 3.86 - 4.01 |
| Associate/bachelor/master degree | 1.67 | 0.02 | 10193 | 0.000 | 5.30 | 5.13 - 5.48 |
| Ph.D. | 1.88 | 0.02 | 11414 | 0.000 | 6.57 | 6.08 - 6.34 |
| Living in rural | 0.01 | 0.01 | 0.443 | 0.011 | 0.47 | 0.47 - 0.48 |
| Family relationship | 0.401 | 0.01 | 10221.98 | 0.000 | 1.50 | 1.49 - 1.51 |
| Multiplicity pregnant | -0.22 | 0.01 | 1100.8 | 0.000 | 1.034 | 1.03 - 1.04 |
| Multiplicity parturition | 0.38 | 0.01 | 2596.12 | 0.000 | 1.12 | 1.12 - 1.13 |
| History of abortion | 0.08 | 0.01 | 72.58 | 0.000 | 0.73 | 0.72 - 0.73 |
| Asphyxia | -0.21 | 0.11 | 4.027 | 0.045 | 0.81 | 0.66 - 0.99 |
| Hydrops fetalis | 0.06 | 0.08 | 0.48 | 0.487 | 1.06 | 0.90 - 1.24 |
| Apgar score | ||||||
| Apgar mint 1 | 0.06 | 0.01 | 650.1 | 0.000 | 1.06 | 1.056 - 1.06 |
| Apgar mint 5 | -1.07 | 1.19 | 0.81 | 0.369 | 0.34 | 0.03 - 3.52 |
| Sex | 0.05 | 0.01 | 211.3 | 0.000 | 1.05 | 1.04 - 1.05 |
| Need to resuscitation | -0.38 | 0.01 | 3904.00 | 0.000 | 0.68 | 0.68 - 0.69 |
| Maternal risk factors | ||||||
| Chronic hypertension | -0.57 | 0.02 | 1061 | 0.000 | 0.45 | 0.43 - 0.46 |
| Diabetes | -0.62 | 0.01 | 2938 | 0.000 | 0.42 | 0.41 - 0.43 |
| Preeclampsia or eclampsia | -0.52 | 0.02 | 1290 | 0.000 | 0.51 | 0.49 - 0.52 |
| Heart diseases | -0.32 | 0.02 | 181.56 | 0.000 | 0.60 | 0.58 - 0.63 |
| Thyroid | -0.73 | 0.01 | 5349 | 0.000 | 0.43 | 0.43 - 0.44 |
| Anemia | -0.11 | 0.03 | 19.02 | 0.000 | 0.82 | 0.78 - 0.86 |
| HIV | -0.78 | 0.15 | 26.06 | 0.000 | 0.37 | 0.28 - 0.49 |
| Syphilis | -0.51 | 0.19 | 7.45 | 0.006 | 0.60 | 0.42 - 0.87 |
| RDS | 0.03 | 0.16 | 0.04 | 0.000 | 1.64 | 1.25 - 2.17 |
| Pulmonary hemorrhage | -0.25 | 0.58 | 0.19 | 0.44 | 1.49 | 0.53 - 4.32 |
| Meconium aspiration syndrome | 0.53 | 0.46 | 1.35 | 0.000 | 5.47 | 2.29 - 13.07 |
| Air leak syndrome | 0.26 | 0.82 | 0.10 | 0.480 | 1.67 | 0.397 - 6.94 |
| Gestational age (wk) | ||||||
| > 28 | -1.77 | 0.03 | 3243 | 0.000 | 3.98 | 3.80 - 4.18 |
| 28 - 32 | -1.85 | 0.03 | 5328 | 0.000 | 0.68 | 0.66 - 0.71 |
| 33 - 36 | -1.38 | 0.02 | 3195 | 0.000 | 0.63 | 0.62 - 0.64 |
Abbreviation: RDS, respiratory distress syndrome.
5. Discussion
Given the potential risks and financial burden associated with CS, ongoing investigation into the underlying causes and epidemiologic drivers of its high utilization is essential. This study seeks to explore maternal and neonatal sociodemographic factors influencing delivery preferences by analyzing comprehensive data from Iran’s national birth registration system spanning April 2015 to April 2016. A systematic review previously conducted in Iran reported a CS prevalence of 48%, which is consistent with the 49.9% rate observed in our study (10). Interestingly, the analysis revealed that older maternal age was linked to reduced odds of undergoing CS, which contrasts with findings from other studies that typically associate advanced maternal age with increased CS rates. This discrepancy may reflect unique aspects of clinical practice in Iran or suggest that older mothers, having had prior vaginal deliveries, are more likely to continue with non-surgical birth methods (11). Our data were derived from a national registry, which included all deliveries rather than a hospital-based or selected sample. Therefore, the influence of clinical decision protocols and resource availability may differ from studies conducted in tertiary centers where CS is more frequently indicated. In many regions of Iran, women with pregnancy complications are closely monitored during pregnancy and often managed through timely medical interventions, possibly reducing emergency CS indications.
Our findings indicate that higher maternal education — especially among women holding a doctoral degree was strongly associated with an increased likelihood of choosing CS, aligning with trends reported in previous research. This may reflect the fact that more educated women often have greater access to health information and may seek greater autonomy and control over their childbirth experience (12, 13). Our study indicates that highly educated mothers were 6.57 times more likely to undergo CS compared to illiterate mothers. Additionally, residing in rural areas — as opposed to cities — was associated with a statistically significant reduction in the likelihood of CS (OR = 0.528, P = 0.01).
The worldwide increase in CS rates has been extensively reported, yet the factors driving this trend are multifaceted and vary across different cultural and healthcare contexts. The findings from our study contribute to this ongoing discourse by highlighting how sociodemographic variables — such as maternal education, age, and place of residence — may influence delivery preferences and help explain the rising prevalence of CS. The strong association between higher maternal education and increased CS preference — particularly among mothers holding a doctoral degree — suggests that education may empower women to make more autonomous decisions regarding childbirth, often favoring CS for perceived safety, convenience, or control over timing. This pattern mirrors global observations where educated women in both high- and middle-income countries exhibit higher CS rates (14, 15). Likewise, residing in urban areas was associated with a higher likelihood of CS. This trend may be attributed to greater availability of surgical infrastructure, institutional practices that favor medicalized childbirth, and distinct dynamics between patients and healthcare providers in urban settings (16). Although our study found that older maternal age was associated with lower odds of CS — contrary to global trends — this discrepancy may be explained by Iran-specific factors such as multiparity and clinical practices that prioritize VD in older mothers with previous successful births (17). Taken together, these findings suggest that shifts in maternal demographics, healthcare access, and cultural attitudes toward childbirth are key contributors to the worldwide escalation in CS rates.
Our analysis did not reveal a significant association between CS preference and a history of pregnancy or prior delivery. This finding contrasts with research from Pakistan, which indicated that women delivering their first child via CS were more likely to opt for the same method in subsequent pregnancies. Such differences may reflect variations in clinical guidelines, cultural attitudes, or healthcare provider practices across settings (18).
Notably, our study found that pregnancy complications were associated with a significantly reduced likelihood of CS, a finding that diverges from much of the existing literature. Previous research has commonly linked CS preference to medical conditions such as chronic hypertension, cardiac disease, pulmonary disorders, and other high-risk factors. This unexpected result may reflect differences in clinical decision-making, patient preferences, or healthcare resource allocation within the Iranian context (19).
Based on our results, CS appears to be a more suitable delivery method in cases of fetal distress and the need for resuscitation, which aligns with prior research showing an increased likelihood of CS under these conditions (20, 21). Additionally, a cross-sectional study conducted in Iran identified prior CS and fetal distress as two of the most frequently cited obstetrical-medical reasons contributing to elevated CS rates. These findings underscore the role of clinical history and emergent fetal conditions in shaping delivery decisions (11). Supporting Yeganegi et al.’s findings, which showed a higher risk of respiratory problems in neonates were born via CS (22), our study also identified an increased risk of RDS and air leak syndrome in CS deliveries. Osman et al. found that CS — particularly elective procedures — are linked to higher rates of pneumothorax (23). Furthermore, the increased incidence of meconium-stained amniotic fluid and meconium aspiration syndrome in CS deliveries (24) supports the observed rise in air leak syndrome in these cases.
While our findings highlight descriptive associations between sociodemographic factors and CS preference, it is crucial to explore the underlying mechanisms driving these patterns. The strong correlation between higher maternal education and CS preference may reflect not only greater autonomy and access to health information, but also evolving perceptions of childbirth risk and expectations. Educated women may be more receptive to medical narratives that portray CS as a safer or more controlled option — particularly in contexts where VD is viewed as unpredictable or painful. This underscores the need for targeted antenatal counseling that promotes informed decision-making through balanced, evidence-based communication.
Conversely, the lower likelihood of CS among rural residents may be influenced by limited access to surgical services, prevailing cultural norms favoring natural birth, and systemic resource constraints that prioritize VD unless medically necessary. This disparity raises important equity concerns, as rural women may encounter obstacles in accessing CS when clinically indicated. Addressing these gaps requires strengthening referral pathways and expanding surgical capacity in underserved regions to ensure that all women receive appropriate, timely, and safe obstetric care.
The unexpected inverse relationship between older maternal age and CS observed in our cohort — contrary to global trends — may be attributed to multiparity and a history of vaginal deliveries, which often reduce the clinical need for surgical intervention. However, this finding also prompts critical reflection on local obstetric practices and whether age-related risks are being appropriately evaluated. It underscores the need for clearer clinical guidelines that integrate maternal age with parity and medical history to support more individualized and evidence-based decisions regarding delivery mode. Finally, the counterintuitive observation that pregnancy complications were linked to lower rates of CS challenges conventional assumptions about clinical decision-making. This finding may be indicative of underreporting of complications, delays in their recognition, or systemic barriers that hinder timely surgical intervention. Such issues underscore the urgent need for enhanced prenatal screening protocols, standardized documentation practices, and targeted clinical training to ensure that maternal complications are accurately identified and managed using the most appropriate and safest delivery method. Taken together, these findings underscore the multifaceted nature of CS trends, shaped by an intricate interplay of maternal education, healthcare access, clinical norms, and patient expectations. Effectively addressing these drivers’ calls for coordinated public health strategies that integrate provider training, culturally sensitive and patient-centered counseling, and systemic reforms. Such efforts are essential to promote the judicious and equitable use of CS — ensuring that surgical delivery is reserved for medically necessary cases while empowering women to make informed choices about their childbirth experience.
5.1. Conclusions
The study highlights the significant influence of academic achievement on childbirth choices in Iran. Women with higher educational levels — especially mothers holding a doctoral degree — were substantially more inclined to opt for cesarean delivery, suggesting that education impacts both health awareness and access to specialized medical options.
Cesarean births were associated with improved immediate neonatal outcomes, including higher Apgar scores, yet also carried increased risks for complications such as RDS and meconium aspiration. The likelihood of undergoing a CS was notably higher among urban women, who were often more educated, compared to their rural counterparts. These findings suggest that sociodemographic factors — particularly maternal education and urban residence — exert a stronger influence on CS preference than clinical indications alone. To address the prevalence of non-medically indicated CS, targeted educational initiatives and policy reforms are essential, especially within urban and highly educated populations. Such interventions should promote informed decision-making, balanced risk communication, and equitable access to appropriate delivery options.
5.2. Limitations
This study has several limitations that warrant consideration. Notably, the data analyzed reflect a specific period and may not fully capture shifts in maternal preferences or healthcare practices that have occurred since. Conducting a more recent study would allow for the evaluation of changes in delivery method preferences in relation to evolving sociodemographic, medical, and policy-related variables. Comparative analysis with updated data would enhance the generalizability of our findings and support more robust conclusions.