1. Background and Problem Statement
Malaria, caused by Plasmodium parasites, remains a major global health concern, especially affecting children and pregnant women in tropical and subtropical regions (1). According to the World Health Organization’s (WHO) 2023 World Malaria Report, malaria remains a significant burden, with 249 million cases and 608,000 deaths across 85 endemic countries in 2022 (2). Historically, malaria affected millions in Iran, but the 1951 anti-malaria campaign led to substantial reductions, and recent reports indicate a continuing decline (3, 4). By 2009, Iran had entered the pre-elimination phase, aiming to stop local transmission by 2025 (5). Iran has made remarkable progress in malaria control and is now in the pre-elimination phase, with a national goal to eliminate indigenous transmission by 2025 (6). However, this achievement is fragile. The country now faces a critical challenge: Imported malaria cases from endemic neighboring countries, primarily Afghanistan and Pakistan, threaten to undermine elimination efforts by potentially re-establishing local transmission where competent Anopheles vectors exist.
However, regional instability has influenced malaria dynamics. The recent political change in Afghanistan in 2021, coupled with ongoing economic insecurity, has prompted a significant influx of migrants and refugees into Iran, many originating from malaria-endemic regions within Afghanistan (7, 8). There is a steady flow of Afghan laborers into Iran, particularly young men seeking work, who often have limited access to healthcare and may carry asymptomatic malaria infections (7, 9). Migrants often settle in specific urban and peri-urban areas, creating focal points of potential transmission risk if local vectors are present (9). Qazvin Province, in northern Iran, hosts a significant Afghan refugee population on the city outskirts (10). Qazvin Province illustrates this vulnerability: A 2008 – 2023 retrospective study showed that all malaria cases were imported, predominantly from Afghanistan (9). This pattern reflects a national trend and underscores the need for targeted policies to prevent reintroduction.
2. Materials and Methods
2.1. Study Area and Data Collection
This study was conducted in Iran's Qazvin Province, a 15,821 km² area in the northwest, between 2008 and 2023. During this period, 41 imported malaria cases were identified. Blood samples were collected from patients at provincial Health Centers, and peripheral smears were prepared, stained with Giemsa, and examined by light microscopy for parasite detection. All cases were confirmed by laboratory diagnosis, with no reported fatalities. For each confirmed case, a comprehensive questionnaire was completed, documenting demographic and clinical details such as age, gender, occupation, nationality, parasite species, and the method of case detection (active or passive).
3. Policy Options and Implementation Strategies
We propose three complementary policy alternatives to address the challenge posed by imported malaria:
3.1. Option 1: Targeted Surveillance and Screening of High-Risk Populations
This entails the systematic identification and assessment of individuals exhibiting the highest susceptibility to imported malaria.
Activities: Implement obligatory screening protocols for migrants and returning travelers from endemic regions at designated border crossing points (11). Establish proactive case detection initiatives and community-based screening efforts in urban locales characterized by significant concentrations of Afghan laborers (12).
Advantages: Facilitates early detection and treatment, thereby averting severe disease progression and potential local outbreaks. Allocates limited resources efficiently to focus on the demographic contributing to the issue (13).
Disadvantages: Necessitates considerable investment in rapid diagnostic tests (RDTs) and trained healthcare personnel. Potential cultural barriers may hinder effective implementation (14, 15).
Acceptability: High, as it is directly aligned with the national elimination objective and provides a pragmatic, focused methodology (16, 17).
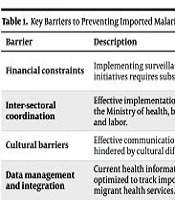
The key barriers and recommended implementation strategies are summarized in Table 1.
| Barrier | Description | Implementation Strategies |
|---|---|---|
| Financial constraints | Implementing surveillance, screening, and cross-border initiatives requires substantial investment. | Mobilize resources through the national health budget, and apply for grants from global health initiatives (e.g., the global fund). Pilot programs in high-risk provinces can demonstrate cost-effectiveness. |
| Inter-sectoral coordination | Effective implementation requires coordination between the Ministry of health, border security, foreign affairs, and labor. | Establish a national malaria elimination taskforce with representation from all key ministries to ensure coordinated policy and action. |
| Cultural barriers | Effective communication with Afghan populations is hindered by cultural differences. | Employ cultural mediators. |
| Data management and integration | Current health information systems may not be optimized to track imported cases and link them to migrant health services. | Strengthen the health management information system to include variables on nationality, travel history, and cross-border movement for malaria cases. |
3.2. Option 2: Enhanced Border Health Initiatives and Cross-Border Collaboration
This alternative emphasizes inter-country cooperation aimed at mitigating the influx of infected individuals while synchronizing control efforts.
Activities: Augment health assessments and health education initiatives at formal border checkpoints. Establish collaborative surveillance, data-sharing agreements, and coordinated response plans in conjunction with the health authorities of Afghanistan and Pakistan (18, 19).
Advantages: Addresses the issue at its origin. Promotes regional collaboration, which is critical for sustained elimination efforts in the area (20).
Disadvantages: Logistically and politically intricate, necessitating high-level diplomatic engagement and ongoing commitment from all involved parties (21).
Acceptability: Moderate to high within the health sector; however, successful implementation is contingent upon broader foreign policy frameworks and bilateral relations (21, 22).
3.3. Option 3: Community-Based Health Education and Engagement Within At-Risk Demographics
This seeks to enhance knowledge and promote protective behaviors among migrant communities.
Activities: Develop and disseminate culturally tailored educational resources regarding malaria symptoms, prevention strategies, and the imperative of seeking timely treatment (23). Train and deploy community health workers (CHWs) sourced from within these populations (24).
Advantages: Empowers communities, fosters trust in the healthcare system, and has the potential to enhance case detection and reporting. Complements screening initiatives effectively (25).
Disadvantages: Requires time to cultivate trust and establish effective communication channels. Outcomes may prove challenging to quantify in the short term (26, 27).
Acceptability: High, as it represents a foundational public health practice that can be integrated with other primary healthcare services for migrants (28, 29).
4. Policy Recommendations
Substantial progress toward malaria elimination has been made in Iran. However, it faces a serious challenge from imported cases, particularly from neighboring endemic countries such as Afghanistan and Pakistan. To sustain these gains and achieve the 2025 elimination target, the country must implement targeted interventions, including:
Systematic screening programs should be implemented for returning travelers and migrants from endemic regions at official border crossings. The use of RDTs should be expanded for timely case detection, especially among Afghan laborers residing in peri-urban areas. Collaboration agreements should be established or enhanced with the health ministries of Afghanistan and Pakistan for data sharing and coordinated outbreak response planning. Capacity for health monitoring at borders should be increased, and education should be provided to crossing travelers. Educational content (e.g., brochures, videos) should be developed and distributed in languages common among migrant communities (such as Dari and Pashto) about malaria symptoms and the importance of prompt treatment. The CHWs should be recruited, trained, and deployed from within these communities to increase effectiveness and build trust. The Health Management Information System (HMIS) should be upgraded to effectively track imported cases by including variables such as nationality, travel history, and linkage to migrant health services. Data from different sectors (health, border security) should be integrated for better analysis of disease importation patterns. Dedicated and sustained funding should be allocated within the national health budget for malaria elimination activities. Technical and financial assistance should be secured by applying for grants from international bodies such as the Global Fund to Fight AIDS, Tuberculosis and Malaria. These recommendations align with the barriers and strategies highlighted in Table 1.
5. Discussion
Iran has successfully interrupted local malaria transmission, yet the persistent influx of imported cases, primarily among young Afghan male laborers, presents a critical vulnerability. To safeguard elimination achievements and meet the 2025 target, Iran must shift from broad national measures to targeted, practical interventions. These include implementing mandatory screening at borders and in-migrant communities using RDTs, enhancing cross-border collaboration for joint surveillance and outbreak response with Afghanistan and Pakistan, and scaling up culturally adapted community health education delivered by trained CHWs. The sustained success of these measures depends on strong inter-sectoral coordination, dedicated national funding, and support from international partners. With committed political and financial backing, Iran can prevent the re-establishment of malaria and achieve its elimination goal.