1. Context
Palliative care is an all-encompassing, multi-faceted strategy in medical practice, primarily intended to enhance the quality of life of individuals facing serious illnesses and to assist their families through the reduction of physical, emotional, social, and spiritual distress (1). Although this type of care has traditionally been associated with patients with cancer or terminal chronic illnesses, in recent years, its importance and necessity in intensive care unit (ICU) settings have received increasing attention (2, 3).
The ICU settings are recognized for their focus on delivering intensive, technology-driven interventions to critically ill patients. However, for patients with poor prognoses — particularly those whose likelihood of discharge with an acceptable quality of life is low due to disease severity, multiple comorbidities, or functional impairment — an exclusive emphasis on life-saving treatment may lead to prolonged suffering, increased caregiving burden, and severe psychological stress for families (4). In such circumstances, integrating palliative care principles into ICU management can facilitate more informed decision-making, optimize symptom control, and improve the experience of both patients and their families (5, 6). In this context, Albert Schweitzer emphasized that the primary responsibility of ICU healthcare staff is to alleviate patients’ pain and suffering rather than to cure them, as suffering and pain can, for humanity, be worse than death itself (7).
Evidence has shown that the implementation of palliative care in the ICU is associated with multiple positive outcomes, including a reduction in unnecessary length of stay, improved family satisfaction, decreased use of non-beneficial end-of-life interventions, and optimization of healthcare resource utilization (8, 9). In this context, the results of a systematic review by Metaxa et al., which examined palliative care interventions in ICU patients, demonstrated that both integrative and consultative models of palliative care in the ICU can yield positive outcomes, particularly in reducing length of stay and increasing decisions related to treatment limitation (10).
Nevertheless, considerable barriers — such as insufficient specialized training of ICU staff in palliative care principles, ethical concerns related to treatment limitation, cultural differences in attitudes toward death, and the lack of supportive organizational structures — have hindered the full integration of this approach in many countries, including middle-income nations (11, 12). Despite these challenges, familiarity with palliative care can be highly beneficial for nurses. For example, the study conducted by Karadag Arli showed that nurses’ knowledge of palliative care and its management helps them effectively manage symptoms like pain and dyspnea (13).
Given the high burden of critical illness and the elevated mortality rates among ICU patients with poor prognoses, reviewing the existing evidence and examining models, interventions, and challenges in implementing palliative care in the ICU can contribute to the progression of more effective strategies and the localization of such services. This narrative review was conducted with the aim of providing a comprehensive analysis of the existing literature and proposing a framework for improving the integration of palliative care into the ICU, in order to enhance the quality of care and patient-family experience while ensuring optimal utilization of healthcare resources.
2. Evidence Acquisition
This study was carried out as a narrative review aiming to compile and examine the current evidence on interventions, models, and outcomes associated with the integration of palliative care for adult patients in ICUs.
2.1. Information Sources and Search Strategy
An extensive search was performed across international databases (PubMed/MEDLINE, Scopus, Embase, Web of Science, Google Scholar) and national databases (Magiran, Irandoc, SID). The search period was defined from January 2010 to July 2025 in order to capture both seminal classical studies and the most up-to-date research available at the time of manuscript preparation. The search strategy was designed by combining free-text keywords with standardized medical subject headings (MeSH) terms. For example, the PubMed search string was as follows: ["Palliative Care"(MeSH) OR "Palliative Care"(tiab)] AND ["Critical Care"(MeSH) OR "Critical Care"(tiab)] AND ["Intensive Care Units"(MeSH) OR "ICU"(tiab)] AND ["Terminal Care"(MeSH) OR "End-of-life care"(tiab)] AND ["Health Services Integration"(MeSH) OR "Models, Organizational"(MeSH) OR "Health Care Barriers"(MeSH)]. Filters were applied to include studies published between 2010 and July 2025, in English or Persian, and limited to human studies. Equivalent search terms were adapted for other databases (Scopus, Embase, Web of Science, Magiran, Irandoc, SID), with minor adjustments in syntax. A detailed description of search strings for each database is provided in Table 1.
| Database | Search String | Filters Applied |
|---|---|---|
| PubMed/MEDLINE | ["Palliative Care"(MeSH) OR "Palliative Care"(tiab)] AND ["Critical Care"(MeSH) OR "Critical Care"(tiab)] AND ["Intensive Care Units"(MeSH) OR "ICU"(tiab)] AND ["Terminal Care"(MeSH) OR "End-of-life care"(tiab)] AND ["Health Services Integration"(MeSH) OR "Models, Organizational"(MeSH) OR "Health Care Barriers"(MeSH)] | Publication date: Jan 2010 - Jul 2025; language: English and Persian; species: Humans |
| Scopus | TITLE-ABS-KEY("Palliative Care") AND TITLE-ABS-KEY("Critical Care") AND TITLE-ABS-KEY("Intensive Care Unit" OR "ICU") AND TITLE-ABS-KEY("Terminal Care" OR "End-of-life care") AND [TITLE-ABS-KEY("Health Services Integration") OR TITLE-ABS-KEY("Models, Organizational") OR TITLE-ABS-KEY("Health Care Barriers")] | Year: 2010 - 2025; language: English and Persian; document type: Article |
| Embase | ('palliative care'/exp OR 'palliative care':ti,ab) AND ('critical care'/exp OR 'critical care':ti,ab) AND ('intensive care unit'/exp OR 'ICU':ti,ab) AND ('terminal care'/exp OR 'end of life care':ti,ab) AND ('health services integration'/exp OR 'organizational model'/exp OR 'health care barrier'/exp) | 2010 - 2025; humans; English and Persian |
| Web of Science | TS=("Palliative Care") AND TS=("Critical Care") AND TS=("Intensive Care Unit" OR "ICU") AND TS=("Terminal Care" OR "End-of-life care") AND TS=("Health Services Integration" OR "Models, Organizational" OR "Health Care Barriers") | Year: 2010 - 2025; language: English and Persian |
| Google Scholar | "Palliative Care" AND "Critical Care" AND ("Intensive Care Unit" OR "ICU") AND ("Terminal Care" OR "End-of-life care") AND ("Health Services Integration" OR "Models, Organizational" OR "Health Care Barriers") | First 200 results screened; 2010 - 2025; English and Persian |
| Magiran/SID/Irandoc | "Terminal Care" AND "ICU" OR AND "Intensive Care Unit" KEY ("Palliative Care") AND ("Critical Care") | Year: 2011 - 2025; Language: Persian |
Abbreviations: MeSH, medical subject headings; ICU, intensive care unit.
2.2. Eligibility Criteria
Studies were considered for inclusion if they fulfilled the following criteria: Publication in peer-reviewed academic journals; focus on palliative care interventions or models in ICU patients; inclusion of adult populations (≥ 18 years); provision of empirical data or analytical reviews supported by valid evidence; and publication in English or Persian. Exclusion criteria included: Letters to the editor, commentaries, conference abstracts or posters, case reports or small case series (< 5 patients), studies focusing on palliative care outside of the ICU, and articles without full text or lacking valid scientific evidence.
2.3. Study Selection and Quality Assessment
The titles and abstracts of the retrieved studies were independently reviewed by two researchers, and studies meeting the eligibility criteria were subsequently evaluated through full-text assessment. Discrepancies were addressed through discussion and consensus, and if required, a third reviewer was consulted. The overall quality of the included studies was assessed according to their respective designs using validated tools. For review articles, compliance with the preferred reporting items for systematic reviews and meta-analyses (PRISMA) checklist was evaluated, including clarity of objectives, comprehensiveness of the search strategy, and transparency of reporting. Clinical trials were appraised using the Consolidated Standards of Reporting Trials (CONSORT) guidelines, focusing on randomization, blinding, and outcome reporting. Analytical cross-sectional studies were assessed with the JBI Critical Appraisal Checklist, which examines methodological quality, validity, and risk of bias. Qualitative studies were evaluated using the Critical Appraisal Skills Programme (CASP) checklist, emphasizing credibility, relevance, and rigor. Although this study is a narrative review, we employed certain elements of the PRISMA guidelines (such as the flow diagram) to increase transparency in reporting the search and selection process. However, as no systematic quantitative synthesis was performed, the full application of PRISMA was not applicable.
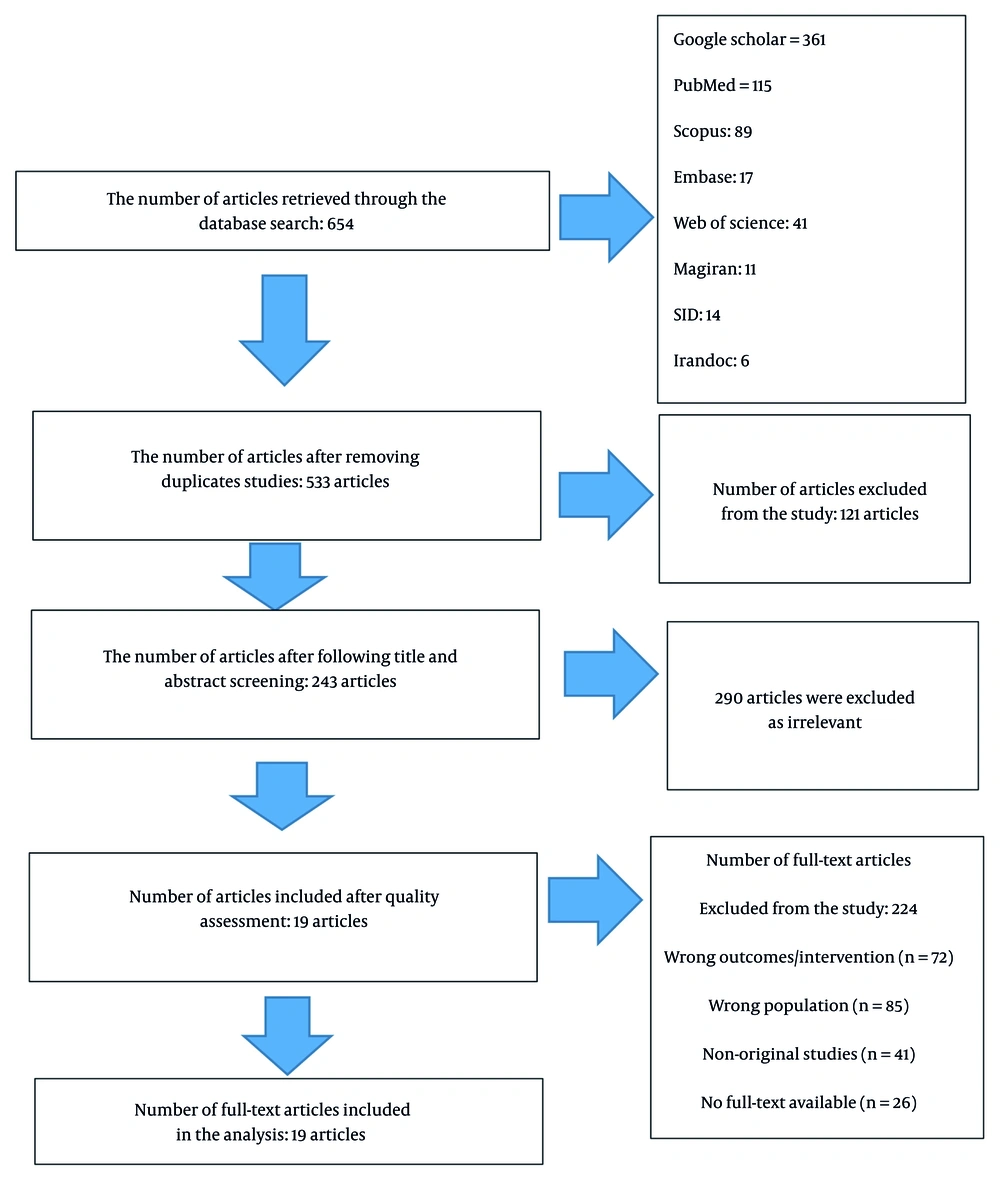
A total of 654 full-text articles, published in peer-reviewed journals and addressing palliative care in the ICU, were collected using EndNote X8. After removing 121 duplicates, 533 records remained. Following title and abstract screening, 290 articles were excluded as irrelevant. At the full-text assessment stage, 224 articles were excluded for the following reasons: Wrong population (n = 85), wrong intervention or outcomes (n = 72), non-original studies such as editorials or commentaries (n = 41), and unavailable full-texts (n = 26). Ultimately, 19 studies met the inclusion criteria and were included in the review. The detailed process of searching, screening, and selecting studies is presented in the PRISMA flow diagram (Figure 1).
2.4. Data Extraction and Analysis
Key information, including author and year of publication, country of study, type of palliative intervention, applied model (consultative or integrative), target population, outcome measures (such as length of stay, mortality, family satisfaction, and resource utilization), and main findings, was extracted and organized into tables. A qualitative analysis of the data was then performed to identify patterns, similarities, differences, and existing research gaps.
3. Results
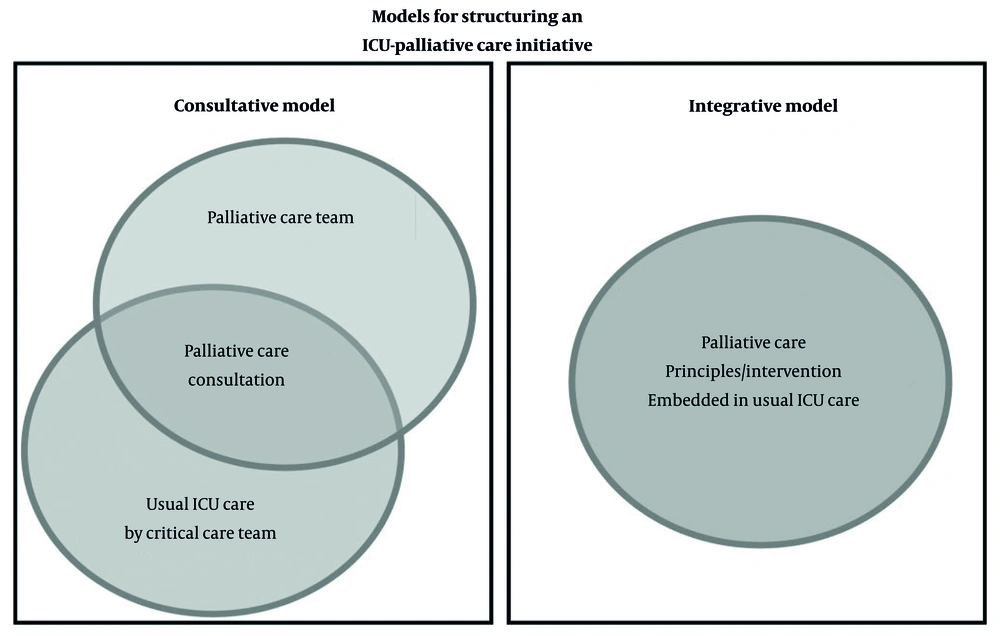
Of the 19 selected articles, 7 employed an expert consensus report with a narrative review, 2 used a narrative review design, 2 were systematic reviews with meta-analysis, 3 were systematic reviews, 3 were interventional studies, and 1 utilized a mixed-methods approach. All articles were published in English. Based on the findings of these 18 studies, several key themes in the provision of palliative care in the ICU can be identified. First, two main models for integrating palliative care were highlighted: The consultative model (utilizing a specialized palliative care team) and the integrative model (embedding palliative care principles within the ICU team). Both models were associated with improved symptom management, alignment of treatment with patient preferences, family support, and reduced length of stay. The specifications of this model, as derived from the study by Nelson et al. (14), are illustrated in Figure 2. In the consultative model, the emphasis is on enhancing the role and impact of palliative care specialists in managing ICU patients and supporting their families. Conversely, the integrative model aims to incorporate palliative care principles and interventions into the routine care provided by the ICU team for all patients and families dealing with critical illness. Specialized training for nurses, development of standardized protocols, and interprofessional collaboration were identified as key factors for successful implementation, although insufficient training and limited resources remain major challenges.
Palliative care interventions included the management of physical and psychological symptoms, advanced care planning, active patient and family involvement in decision-making, and the provision of spiritual and cultural support. Evidence indicates that these interventions enhance the quality of care, increase patient and family satisfaction, and reduce ICU resource utilization, while ongoing nurse education is essential to maintain competency and ensure effective delivery of care. Additionally, the use of appropriate screening criteria and triggers for palliative care referral can improve access to these services and facilitate clinical decision-making. As shown in Table 2, these results consistently emphasize the central role of nurses, the effectiveness of integrative and consultative models, the benefits of advance care planning, and the importance of education and standardized protocols in improving palliative care delivery in the ICU.
| Authors | Title | Study Type | Key Findings |
|---|---|---|---|
| Nelson et al. (2010) | Models for structuring a clinical initiative to enhance palliative care in the ICU: A report from the IPAL-ICU project | Consensus report/review of clinical initiatives | Two models for integrating palliative care in the ICU have been identified: The consultative model (utilizing a specialized palliative care team) and the integrative model (incorporating palliative care principles directly by ICU physicians). Effective integration enhances symptom management, aligns treatment with patient preferences, facilitates care transitions, and supports families (14) |
| Nelson et al. (2011) | Integrating palliative care in the ICU; the nurse in a leading role | Narrative/review with practical recommendations | Nurses play a vital role in delivering palliative care in the ICU, improving the quality of care through symptom management and support for patients and their families. Integrating palliative care is associated with reduced length of stay and decreased workload for the healthcare team. However, a lack of specialized training and limited resources remain significant challenges. Enhancing nurse education and developing standardized protocols can improve the quality of care (15). |
| Mosenthal et al. (2012) | Integrating palliative care in the surgical and trauma ICU: A report from the IPAL-ICU Project Advisory Board and the Center to Advance Palliative Care | Expert consensus report with literature review | The characteristics of surgical patients and the interactions among different care teams create specific challenges for delivering palliative care in the ICU. Consultative, integrative, and combined models can enhance care quality, although the optimal criteria for initiating consultations remain unclear. Successful integration requires collaboration among medical, nursing, and palliative care teams, with attention to cultural and organizational factors (16). |
| Nelson et al. (2013) | Choosing and using screening criteria for palliative care consultation in the ICU: A report from the IPAL-ICU Advisory Board | Narrative review / Expert consensus report | This study examines screening criteria (triggers) for referring ICU patients to palliative care. The use of these criteria can reduce ICU resource utilization and increase patient and family access to palliative services without affecting mortality. The criteria should be tailored to each ICU and implemented in collaboration with stakeholders (17). |
| Aslakson et al. (2014) | The changing role of palliative care in the ICU | Narrative review / Expert consensus report | Palliative care should begin at ICU admission, regardless of diagnosis or prognosis. Evidence suggests that this approach can reduce physical and psychological symptoms, enhance communication, and provide effective support for patients and their families. Additionally, resources and tools are available to implement these improvements, and attention to post-ICU discharge challenges is of high importance (18). |
| Frontera et al. (2015) | Integrating palliative care into the care of neurocritically ill patients: A report from the IPAL-ICU Project Advisory Board and the Center to Advance Palliative Care | Narrative review / Expert consensus report | The sudden onset of severe cognitive and functional impairments in neurocritical illness complicates decision-making, and the application of palliative care principles — including symptom management, emotional support for families, and respect for patient preferences — can enhance care quality and help maintain the professionalism of the healthcare team (19). |
| Khandelwa et al. (2015) | Estimating the effect of palliative care interventions and advance care planning on ICU utilization: A systematic review | Systematic review and meta-analysis | Advance care planning interventions can reduce the risk of ICU admission by 37% in patients with a high likelihood of mortality. Additionally, palliative care interventions in the ICU are associated with an average 26% reduction in length of stay. Despite the variability and differing quality of studies, the results consistently indicate a pattern of decreased ICU resource utilization and reduced care-related costs (9). |
| Roczen et al. (2016) | Palliative care and ICUs: A systematic review | Systematic review | The results indicate that, although quantitative and qualitative evidence on the impact of palliative care on patient and organizational outcomes is limited and sometimes inconsistent, several important and consistent findings have emerged. These include improved communication between the healthcare team and families, increased patient and family satisfaction, and facilitation of decision-making regarding care goals. Limited quantitative evidence also suggests reductions in costs and length of stay (20). |
| Wysham et al. (2017) | Improving ICU-based palliative care delivery: A multicenter, multidisciplinary survey of critical care clinician attitudes and beliefs | Mixed-methods study | This mixed-methods study conducted in three large academic ICUs explored the attitudes of 303 physicians, nurses, and advanced care providers regarding the integration of palliative care in the ICU. Approximately 75% believed that palliative care consultations were underutilized. The most preferred referral triggers included metastatic cancer, unrealistic treatment goals, end-of-life decision-making, and persistent organ failure, whereas criteria such as advanced age or shorter length of stay were less accepted. The findings indicate that integrating palliative care specialists into the ICU is acceptable and desirable, yet selecting effective and feasible triggers and defining the role of nurses remain challenging (21). |
| Martins et al. (2017) | Palliative care for terminally ill patients in the ICU: Systematic review and meta-analysis | Systematic review and meta-analysis | This systematic review and meta-analysis of eight studies involving 7,846 terminally ill ICU patients demonstrated that the use of palliative care teams significantly reduced mortality (RR = 0.78, 95% CI: 0.70 - 0.87) and decreased ICU length of stay by an average of approximately 2.5 days. These findings suggest that integrating palliative care teams into the ICU can both improve patient outcomes and reduce resource utilization (22). |
| Morrison et al. (2018) | Integrating palliative care into the ICU: From core competency to consultative expertise | Literature review and author opinion | This study proposes a three-tiered model for integrating palliative care in the ICU: Basic skills for all team members (primary), internal specialization for selected members (secondary), and an external consultative team for patients requiring extensive care (tertiary). The implementation of the model varies depending on the resources and structure of each center, and interdisciplinary collaboration is essential (23). |
| Mercadante et al. (2018) | Palliative care in ICUs: Why, where, what, who, when, and how | Narrative review | Palliative care in the ICU encompasses symptom management, end-of-life care, effective communication with families, and setting treatment goals while maintaining patient dignity. Successful implementation requires specialized training for anesthesiologists and critical care providers, development of patient selection protocols, utilization of integrative or consultative models, and identification of appropriate referral triggers. Key challenges include limited training, logistical barriers, and the absence of clear referral pathways, while the recommended solutions involve fostering interprofessional collaboration and establishing standardized processes (24). |
| Ganz et al. (2020) | introducing Palliative care into ICUs: An interventional study | Interventional Study | This study was conducted on 122 participants across four national ICU palliative care training courses, assessing changes in their knowledge, attitudes, and performance before and after the course, as well as 2 to 5 years later. The results demonstrated that the training significantly improved participants’ attitudes and performance in palliative care, while knowledge levels and the quality of dying remained stable after the course. Participants acquired the necessary skills to provide palliative care, but organizational barriers hindered its widespread implementation in the ICU (25). |
| Eltaybani et al. (2021) | Palliative care in adult ICUs: A nationwide survey | Cross-sectional survey | This study was conducted on 33 nursing managers and 403 adult ICU nurses in Egypt to evaluate education, performance, and perceived competence in palliative care. The results showed low mean scores for education, performance, and perceived competence (54.0, 49.7, and 54.5 out of 100, respectively), with notable deficiencies particularly in spiritual and cultural care. Better performance was associated with on-the-job training, higher job satisfaction, and greater organizational support, while higher competence correlated with older age, job satisfaction, and university-level education (26). |
| Metaxa et al. (2021) | Palliative care interventions in ICU patients | Systematic review | Palliative care interventions in ICU patients were categorized into five main groups: Communication, ethics consultations, education, involvement of the palliative care team, and advance care planning or goals-of-care discussions. Approximately half of the studies employed an integrative model, while the other half used a consultative approach. Key outcomes examined included ICU or hospital length of stay, decisions to limit life-sustaining treatments, and mortality. The findings indicated that active involvement of palliative care, whether through an integrative or consultative model, had beneficial effects on these outcomes (10). |
| Ghaemizade Shushtari et al. (2022) | Effect of end-of-life nursing education on the knowledge and performance of nurses in the ICU: A quasi-experimental study | Quasi-experimental study | This study examined the effect of end-of-life nursing education based on ELNEC on the knowledge and performance of ICU nurses. The findings indicated that the training resulted in a notable improvement in knowledge across nine areas, such as nursing care, pain and symptom management, ethical and legal considerations, cultural aspects, communication with patients and families, coping with loss and grief, end-of-life care, and quality of life. Additionally, nurses’ performance in preparing to provide palliative care, assessing their ability to communicate with dying patients, and palliative care skills improved significantly in the intervention group (27). |
| Pan et al. (2023) | Palliative care in the ICU: Not just end‑of‑life care | Narrative review | This study examines the evolution of palliative care in the ICU from a purely end-of-life approach to an integral component of ICU care. The authors emphasize adherence to ethical principles — autonomy, beneficence, nonmaleficence, justice, and fidelity — and introduce three models for integrating palliative care in the ICU: Integrative, consultative, and combined. The article recommends that all ICU patients benefit from symptom management and shared decision-making and highlights the need for further research to identify the most effective methods for delivering palliative care to patients and their families (28). |
| Araujo et al. (2023) | Nursing interventions in palliative care in the ICU: A systematic review | Systematic review | Effective nursing interventions in palliative care in the ICU include promoting patient autonomy, respecting patient needs, establishing effective communication, engaging in shared decision-making with the patient and family, individualizing care, maintaining basic nursing care, encouraging self-care, and involving palliative care nursing specialists. Continuous education for nurses to provide specialized care is also essential (29). |
| Rask (2025) | Implications of palliative care education amongst critical care nurses and applicable screening criteria for consultation | Interventional Study | The intervention consisted of providing an educational toolkit on palliative care and on screening patients in need of such care in the ICU. The results showed that the mean knowledge scores of nurses increased from 68.3% to 82.2%, and their confidence scores rose from 17.5 to 21.67 (on a Likert scale). These findings indicate that palliative care education and the use of screening tools can better equip nurses to identify patients requiring palliative care and to advocate for referral to specialized teams. The author recommends that annual training and the standardized implementation of screening tools in the ICU could have a broader impact on improving care quality and reducing costs (30). |
Abbreviations: ICU, intensive care unit; IPAL-ICU, improving palliative care in the intensive care unit.
4. Discussion
In ICUs, palliative care is acknowledged as a crucial strategy for enhancing the quality of life of critically ill patients and providing support to their families. Evidence indicates that initiating palliative care from the time of ICU admission, regardless of diagnosis or prognosis, can reduce physical and psychological symptoms, enhance communication between the healthcare team and families, and provide effective patient support (18, 20). In this context, the study by Nelson et al. demonstrated that this approach also leads to more efficient utilization of ICU resources and reduces the workload of the healthcare team without increasing patient mortality (17). Indeed, evidence analysis suggests that early initiation of palliative care can be considered a preventive strategy that not only improves the quality of care but also alleviates psychological and occupational stress on the care team and yields positive economic outcomes.
Various models have been proposed for delivering palliative care in the ICU, each with its own advantages and challenges. The most common approaches are the consultative model, which relies on a specialized palliative care team for patient referrals, and the integrative model, in which ICU physicians and nurses incorporate palliative care principles into routine care (14, 28). Some centers employ a hybrid of these two models to provide greater flexibility in addressing the needs of patients and families (16). Evidence analysis indicates that the successful integration of palliative care requires collaboration among medical, nursing, and specialized palliative care teams, attention to organizational culture, and the development of feasible referral criteria (21).
The role of nurses in delivering palliative care is clearly prominent. By managing symptoms, facilitating communication, and supporting families, nurses can significantly enhance the quality of care (15, 29). In this context, the study by Eltaybani et al. demonstrated that specialized training and ongoing education programs improve nurses’ attitudes, skills, and practical performance in providing palliative care in the ICU (26). Similarly, recent evidence by Rask highlighted that structured educational toolkits combined with objective screening criteria significantly increased ICU nurses’ knowledge and confidence in identifying and referring patients needing palliative care. This suggests that educational interventions not only empower nurses but also strengthen the overall referral process, thereby bridging gaps in palliative care delivery (30). However, insufficient training, limited resources, and organizational obstacles continue to pose significant challenges to the broad adoption of palliative care in ICUs (25, 27). Evidence suggests that focusing on skill development, organizational support, and the provision of continuous education can help reduce disparities in care delivery and improve the experiences of both patients and their families.
Palliative interventions not only improve the quality of care but also have tangible effects on ICU resource utilization. Meta-analytic studies have shown that the involvement of palliative care teams for end-of-life patients reduces mortality and decreases the average length of stay by approximately 2 to 2.5 days (9, 22). Moreover, active engagement in care planning and discussions about treatment goals — whether in an integrative or consultative model — reduces unnecessary use of life-sustaining interventions and enhances clinical decision-making (10). Therefore, implementing palliative care can improve ICU efficiency and contribute to sustainable clinical resource management without compromising care quality or patient safety.
However, in certain patient populations, such as those with cognitive impairments or critical neurological conditions, clinical decision-making is more complex, and the need for palliative support and adherence to patient preferences becomes even more pronounced (19). This underscores that palliative care is not limited to end-of-life scenarios but is a key component in enhancing the quality of ICU care for all critically ill patients (28). Evidence indicates that integrating palliative care into the routine management of patients with complex cognitive and neurological needs can improve clinical outcomes and reduce family stress (19, 28).
From a practical perspective, the successful implementation of palliative care requires a combination of strategies: Developing standardized patient selection protocols, providing specialized training for nurses and physicians, employing either integrated or consultative models, and designing appropriate referral criteria. Evidence from prior studies (23, 24) indicates that applying these approaches not only improves the quality of care and family satisfaction but also reduces costs and alleviates pressure on the healthcare system. This highlights the importance of comprehensive, evidence-based planning for the sustainable implementation of palliative care.
Ultimately, an overview of studies and practical experiences indicates that palliative care in the ICU should be an essential and permanent component of critical care. Developing interprofessional training, investing in resources, and promoting team collaboration, alongside attention to organizational culture and individual patient needs, can optimize the effects of palliative care and represent an important step toward more humane ICU care (14, 29).
So, in general, the findings of this review are closely aligned with its initial objectives. First, regarding models of integration, the evidence consistently identified two dominant approaches — consultative and integrative — both of which were associated with improvements in patient- and family-centered outcomes. Second, with respect to interventions, palliative care strategies such as symptom management, advanced care planning, and nurse-led educational programs demonstrated effectiveness in enhancing care quality and reducing ICU resource utilization. Third, in terms of implementation challenges, limited training, insufficient resources, and organizational barriers were recurrently reported across studies. These insights directly address our review objectives and emphasize the urgent need for structured educational initiatives, interprofessional collaboration, and system-level planning to integrate palliative care into routine ICU practice.
4.1. Conclusions
The evidence from this review indicates that palliative care in ICUs, whether delivered through integrated or consultative models, plays a pivotal role in improving the quality of care, alleviating physical and psychological symptoms in critically ill patients, enhancing family satisfaction, and optimizing resource utilization. Nurses, as central members of the care team, contribute significantly to the implementation of this approach through symptom management, effective communication, and psychosocial support. Specialized and ongoing training, the presence of standardized protocols, interprofessional collaboration, and attention to organizational barriers are essential prerequisites for the success of these interventions. The findings also emphasize that palliative care should not be limited solely to end-of-life situations; rather, it should be regarded as an integral component of critical care for all ICU patients. Implementing evidence-based policies and strategies, investing in human resources, and fostering a supportive organizational culture can serve as effective steps toward making ICU care more humane and efficient. Practical recommendations include the adoption of clear referral criteria and screening tools to identify patients in need of palliative care, the establishment of multidisciplinary training programs to equip ICU staff with essential competencies, and the integration of standardized care pathways that embed palliative care principles into daily ICU practice. Additionally, pilot implementation of hybrid models tailored to the local organizational context may facilitate gradual integration and allow for continuous evaluation and improvement.
4.2. Limitations
Due to its qualitative nature, this narrative review lacks quantitative statistical analysis, and the findings are based on descriptive interpretations of the included studies. Restricting the search to English and Persian may have excluded valuable evidence published in other languages. Heterogeneity among the studies in terms of design, sample size, type of intervention, and outcome measures made comparison and synthesis of findings challenging. Some studies, including study number 26, faced limitations such as small sample sizes or unvalidated tools, which may affect the generalizability of the results. Moreover, the overall quality of the included studies varied, with some lacking rigorous methodology, standardized outcome measures, or sufficient reporting detail. This variability may have introduced bias and limits the strength of the conclusions drawn from this review. Focusing solely on adult ICU patients also limits the applicability of findings to other age groups or care settings. Although quality assessment was conducted using validated tools, the potential for selection and interpretation bias cannot be entirely eliminated. As this was a narrative review, the application of PRISMA was limited to enhancing reporting transparency (e.g., flow diagram). A full PRISMA-based risk of bias and evidence synthesis could not be applied, which restricts comparability with systematic reviews. Finally, given the rapid advancements in palliative care and evolving ICU management approaches, regular updates of this review are recommended to maintain its relevance and accuracy.
4.3. Ethical Considerations
Since the present study is a narrative review, all analyses were based entirely on previously published studies. The data were extracted as reported in the original articles, with no manipulation or alteration of figures or results. Therefore, the authors adhered to all ethical principles related to publication integrity and scholarly honesty.