1. Background
In general, the incidence of cancer and the related mortality are rapidly increasing globally as a result of aging, population growth, and changes in the incidence and frequency of major risk factors for cancer, some of which are associated with economic and social development (1). According to the World Health Organization, cancer has been the first or second leading cause of death before the age of 70 in 112 (out of 183) countries and the third or fourth leading cause in 23 other countries (2). According to World Health Organization statistics, although the incidence of cancer is generally 2 times higher in developed countries compared to developing countries, the resulting mortality rate is much higher in developing countries (2). In Iran, as a developing country, socioeconomic growth and changes in the traditional lifestyle have led to changes in the incidence of cancer and its related risk factors (3). In Iran, cancer is the third leading cause of death, after cardiovascular diseases and accidents, and its incidence has been increasing in recent years (4). The average standardized incidence rate for all cancers was 154.98 per 100,000 people, with significant differences observed between provinces and ethnic groups (5). Iran is recognized as a multi-ethnic country with different lifestyles across various regions. This diversity has resulted in varying cancer statistics throughout Iran (6). Studies have shown that the incidence of cancer varies in different regions (7, 8), which is probably attributable to environmental (9, 10), geographic (11-13), and ethnic (14, 15) risk factors rather than genetic differences. Due to the distinctive nature of cancer and the lack of a definitive treatment, this disease is considered one of the most important research priorities in all societies. In this regard, understanding the geographical incidence of various types of cancer is the first step in proper planning.
Storing epidemiological data and statistics related to cancer is the primary requirement of cancer data systems globally and is among the most important infrastructure needs for establishing a cancer control program. This program plays an important role in the development and monitoring of cancer control programs, including the evaluation of cancer screening programs, the development and implementation of preventive programs, the follow-up of cancer patients, the evaluation of prognostic indicators, and the allocation of financial and human resources (16). Epidemiological studies lead to the identification of the age, gender, racial, economic, and cultural patterns of the disease in a region, and direct attention to specific groups to reduce disabilities and costs through screening, diagnosis, and early treatment (17). In Iran, the first attempt to report cancer using organized methods began in 1956. Currently, the Ministry of Health and Medical Education has implemented population-based cancer registry programs in most cities (18). Following the launch of the national cancer registry network in Iran, analysis of the preliminary reported results shows that the province of Khuzestan is the second most affected province in terms of the incidence of lymphoma.
2. Objectives
This study was conducted with the aim of investigating the 5-year incidence trend of common cancers in Khuzestan.
3. Methods
3.1. Study Design and Data Source
This is a registry-based time trend (serial cross-sectional) study, which was conducted using cancer registry information at the research center of Jundishapur University of Medical Sciences, Ahvaz. It should be noted that, in order to improve the quality and quantity of cancer data registration in Iran, the cancer registry program is implemented with a focus on the population (pathology and non-pathology). In the population-based cancer registry, existing data have been collected since the year 2000 from three main sources: Pathology centers, hospital medical records, and mortality data, and are organized based on patients’ national ID numbers by removing duplicates and matching with previous years’ data, leading to the establishment of a single, comprehensive, and accurate national database. Annual national reports of cancer cases are entered into PARS software after removing duplicates and modifying all patient reports, item by item. The PARS Cancer Registry software is Iran's comprehensive national platform for population-based cancer surveillance. Developed and managed by the Ministry of Health and Medical Education, it serves as the central hub for collecting, processing, and analyzing anonymized data on cancer incidence from across the country. This system employs international coding standards such as International Classification of Diseases for Oncology, Third Edition (ICD-O-3) to ensure data compatibility. The data extracted from PARS are fundamental for determining national cancer trends, guiding public health policies, and supporting epidemiological research in Iran. In this program, each patient and each tumor can be tracked as a single entity, and all related reports are stored in the program. For this study, cancer-related data registered from early 2014 to late 2018 in Khuzestan were extracted and analyzed. The data were collected retrospectively.
3.2. Case Definition and Coding
The data included age, gender, city of residence, type of morphology, location of lesion, age of onset, and stage of the disease, and were provided to the researchers in the form of an Excel file for each year by Khuzestan’s Health Department. Cancer cases were coded according to the ICD-O-3. The category ‘Other skin’ refers specifically to non-melanoma skin cancers (ICD-10 code C44), excluding melanoma (C43). In instances of multiple primary tumors in the same patient, each distinct primary cancer was counted as a separate case, in accordance with the rules of the International Association of Cancer Registries (IACR). The age-standardized incidence rates (ASRs) were calculated per 105 person-years using the direct standardization method based on the World Health Organization World Standard Population (2002).
3.3. Quality Control and Duplicate Removal
First, duplicate items in 2014, 2015, 2016, 2017, and 2018 were identified based on first and last names, father’s name, national ID number (if available), place of residence, and similar pathology, and were removed from the data file. Then, based on the defined coding of malignancies, the morphological types of cancers were determined from the cancer registry reports in Khuzestan.
3.4. Population Denominator and Standardization
Annual mid-year population estimates were obtained from the Statistical Center of Iran (SCI), based on the 2011 and 2016 national censuses, with linear interpolation applied for intermediate years. The ASRs were calculated per 105 person-years using the direct standardization method based on the World Health Organization World Standard Population (2002).
3.5. Statistical Analysis
Trend analysis was conducted using a log-linear regression model to estimate the annual percent change (APC) in ASRs between 2014 and 2018. Due to the unavailability of detailed annual case counts for individual cancer sites at the granular level, APCs were derived based on ASR values from the first (2014) and last (2018) years of the study period, under the assumption of a constant log-linear trend over time. The 95% confidence intervals (CIs) and corresponding P-values were calculated using the Poisson distribution, which models the variance of case counts as equal to their mean — a standard and appropriate assumption for rare events such as cancer incidence in population-based studies. The total number of cases reported over the 5-year period for each cancer site was used to estimate the standard error of the ASR, enabling robust uncertainty quantification despite limited temporal granularity. This methodological approach is widely accepted in cancer epidemiology, particularly for short-term trend analyses (≤ 5 years) when full annual incidence series per cancer site are not accessible — a common scenario in provincial cancer registries in Iran and other middle-income settings. Statistical significance was defined as P < 0.05. All APC estimates, along with their 95% CIs and P-values, are reported in the Results section and summarized for the 13 most common cancers. All statistical analyses were performed using Stata version 12.
4. Results
4.1. Overall Cancer Incidence Trends (2014 - 2018)
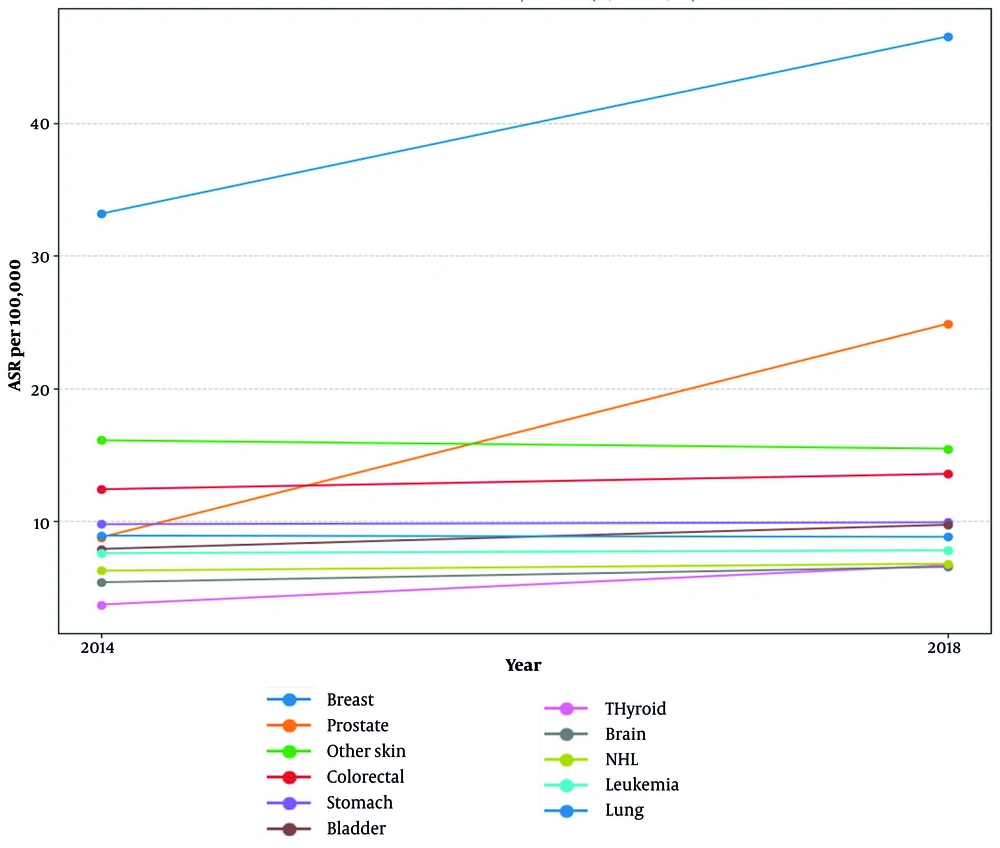
A total of 29,289 cases of cancer were registered in Khuzestan province between 2014 and 2018. Of these 29,289 cases, 5,509 were recorded in 2014, 2,728 in 2015, 6,548 in 2016, 6,572 in 2017, and 6,932 cases in 2018. The crude incidence rate and the ASR for all cancer cases in 2014 for the entire population of the province were 116.64 and 150.90 per 100,000 people, respectively. In 2018, these rates increased to 144.96 and 174.18 per 100,000 population, respectively. Over the 5-year period, the age-standardized incidence increased by 13.37%. Overall cancer incidence showed a statistically significant increase (APC = 2.9%, 95% CI: 1.8 - 4.0, P < 0.001). Among specific cancers, prostate cancer exhibited the steepest rise (APC = 29.5%, 95% CI: 27.1 - 32.0), followed by thyroid (APC = 15.8%, 95% CI: 14.2 - 17.5) and breast cancer (APC = 8.8%, 95% CI: 7.9 - 9.7). Significant increases were also observed for bladder, brain, and colorectal cancers (all P < 0.001). In contrast, other skin cancers showed a modest but significant decline (APC = -1.0%, 95% CI: - 1.8 to -0.2, P = 0.012) (Figure 1).
4.2. Site-Specific Incidence Trends
According to the results shown in Table 1, the highest age-standardized incidence among common cancers in 2014 was related to breast cancer (33.15 per 100,000 people), other skin cancers (11.56 per 100,000 people), colorectal cancer (9.25 per 100,000), and stomach cancer (7.1 per 100,000). In 2018, the highest rates were for breast cancer (incidence rate of 46.51 per 100,000), prostate cancer (17.25 per 100,000 people), other skin cancers (12.05 per 100,000 people), and colorectal cancer (10.98 per 100,000). The 5-year incidence of these cancers (Table 1), except for other skin cancers and lung cancer, showed increasing trends. The highest rates of increase were recorded for prostate cancer (an increase of 183.05%), thyroid (79.41%), breast (30%), bladder (22.95%), and brain (21.4%). A decreasing trend was observed in other skin cancers (-3.91%) and lung cancer (-1.01%).
| Organs | 2014 | 2018 | % Crude | % ASR (per 100,000) | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Number | Crude | ASR (per 100,000) | 95% CIs | Number | Crude | ASR (per 100,000) | 95% CIs | |||
| Breast | 778 | 33.15 | 38.43 | 30.9 - 35.6 | 1121 | 46.51 | 49.96 | 43.9 -49.3 | 40.30 | 30 |
| Prostate | 278 | 5.89 | 8.79 | 7.8 - 9.9 | 419 | 17.25 | 24.88 | 22.6 - 27.4 | 192.87 | 183.05 |
| Other skin | 546 | 11.56 | 16.11 | 14.8 - 17.5 | 576 | 12.05 | 15.48 | 14.3 - 16.8 | 4.24 | -3.91 |
| Colorectal | 437 | 9.25 | 12.42 | 11.3 - 13.6 | 525 | 10.98 | 13.58 | 12.5 - 14.8 | 18.70 | 9.34 |
| Stomach | 331 | 7.01 | 9.79 | 8.8 - 10.9 | 375 | 7.84 | 9.93 | 8.9 - 11.0 | 11.84 | 1.43 |
| Bladder | 269 | 5.70 | 7.93 | 7.0 - 9.0 | 367 | 7.68 | 9.75 | 8.8 - 10.8 | 34.74 | 22.95 |
| Thyroid | 177 | 3.75 | 3.74 | 3.2 - 4.4 | 336 | 7.03 | 6.71 | 5.9 - 7.6 | 87.47 | 79.41 |
| Trachea, bronchus and lung | 300 | 6.35 | 8.93 | 8.0 - 10.0 | 323 | 6.75 | 8.84 | 7.9 - 9.9 | 6.30 | -1.01 |
| Leukemia | 303 | 6.42 | 7.61 | 6.8 - 8.5 | 317 | 6.63 | 7.83 | 7.0 - 8.8 | 3.27 | 2.89 |
| Uterus | - | - | - | - | 148 | 6.29 | 7.25 | 6.1 - 8.6 | - | - |
| Brain, nervous system | 218 | 4.62 | 5.42 | 4.7 - 6.2 | 284 | 5.94 | 6.58 | 5.8 - 7.4 | 28.57 | 21.4 |
| Non-Hodgkin lymphoma | 239 | 5.06 | 6.29 | 5.5 - 7.2 | 274 | 5.73 | 6.82 | 6.0 - 7.7 | 13.24 | 8.43 |
| O&U | 269 | 6.27 | 8.57 | 7.6 - 9.7 | - | - | - | - | - | - |
Abbreviations: ASR, age-standardized rate; CIs, confidence intervals; O&U, other and unspecified.
4.3. Sex-Specific Patterns of Common Cancers
The highest age-standardized incidence of common cancers among men in 2014 was observed for other skin cancers, prostate, colorectal, and stomach cancers, with incidence rates of 18.71, 18.13, 15.21, and 13.52 per 100,000 people, respectively. In women, breast cancer, other skin cancers, and colorectal cancer had incidence rates of 38.43, 13.69, and 9.82 per 100,000 people, respectively (Table 2).
| Organs | 2014 | 2018 | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Male | Female | Male | Female | |||||||||
| N | Crude | ASR per 100,000 (95% CI) | N | Crude | ASR per 100,000 (95% CI) | N | Crude | ASR per 100,000 (95% CI) | N | Crude | ASR per 100,000 (95% CI) | |
| Breast | - | - | - | 778 | 33.15 | 38.43 (35.8 - 41.2) | - | - | - | 1094 | 46.51 | 49.96 (47.1 - 53.0) |
| Prostate | 278 | 11.70 | 18.13 (16.0 - 20.5) | - | - | - | 419 | 17.25 | 24.88 (22.6 - 27.4) | - | - | - |
| Other skin | 308 | 12.96 | 18.71 (16.7 - 21.0) | 238 | 10.14 | 13.69 (12.0 - 15.6) | 326 | 13.42 | 17.65 (15.8 - 19.7) | 250 | 10.63 | 13.33 (11.7 - 15.1) |
| Colorectal | 262 | 11.03 | 15.21 (13.4 - 17.2) | 175 | 7.46 | 9.82 (8.4 - 11.4) | 317 | 13.05 | 16.62 (14.9 - 18.5) | 208 | 8.84 | 10.61 (9.2 - 12.2) |
| Stomach | 220 | 9.26 | 13.52 (11.8 - 15.5) | 111 | 4.73 | 6.32 (5.2 - 7.7) | 242 | 9.96 | 12.83 (11.3 - 14.6) | 133 | 5.65 | 7.08 (5.9 - 8.4) |
| Bladder | 217 | 9.13 | 12.95 (11.3 - 14.8) | 52 | 2.22 | 3.13 (2.3 - 4.2) | 299 | 12.31 | 16.07 (14.03 - 18.0) | - | - | - |
| Thyroid | - | - | - | 139 | 5.92 | 5.95 (5.0 - 7.1) | - | - | - | 263 | 11.18 | 10.60 (9.4 - 12.0) |
| Trachea, bronchus and lung | 207 | 8.71 | 12.60 (11.0 - 14.5) | 93 | 3.96 | 5.43 (4.4 - 6.7) | 233 | 9.59 | 12.72 (11.2 - 14.5) | 90 | 3.83 | 5.00 (4.0 - 6.2) |
| Leukemia | 172 | 7.24 | 8.73 (7.5 - 10.2) | 131 | 5.58 | 6.49 (5.4 - 7.8) | 191 | 7.86 | 9.41 (8.1 - 10.9) | 126 | 5.36 | 6.27 (5.2 - 7.5) |
| Uterus | - | - | - | - | - | - | - | - | - | 148 | 6.29 | 7.25 (6.1 - 8.6) |
| Brain, nervous system | 127 | 5.35 | 6.32 (5.3 - 7.5) | 91 | 3.88 | 4.54 (3.7 - 5.6) | 153 | 6.30 | 6.99 (5.9 - 8.2) | 131 | 5.57 | 6.19 (5.2 - 7.4) |
| Non-Hodgkin lymphoma | 144 | 6.06 | 7.86 (6.6 - 9.3) | 95 | 4.05 | 4.83 (3.9 - 6.0) | 148 | 6.09 | 7.35 (6.2 - 8.7) | 126 | 5.36 | 6.31 (5.3 - 7.5) |
| O&U | 152 | 6.40 | 9.50 (8.0 - 11.2) | 144 | 6.14 | 7.80 (6.6 - 9.3) | 145 | 5.97 | 7.47 (6.3 - 8.8) | 101 | 4.29 | 5.13 (4.2 - 6.3) |
| Kidney | - | - | - | - | - | - | 98 | 4.03 | 5.42 (4.4 - 6.7) | - | - | - |
| Ovary | - | - | - | 77 | 3.28 | 3.88 (3.1 - 4.9) | - | - | - | 119 | 5.06 | 5.84 (4.8 - 7.1) |
Abbreviations: ASR, age-standardized rate; CI, confidence interval; O&U, other and unspecified.
4.4. Diagnostic Verification and Data Quality Indicators
Based on the results in Table 3, of all the cancer cases registered in 2014, cancer diagnosis was confirmed by microscopically verified (MV) methods, including pathology or cytology, in 4,036 cases (73.26%). The diagnosis was purely clinical or based on clinical evaluation in 1,037 of the registered cancer cases (18.82%). In 436 cases (7.91%) of registered patients, the cancer diagnosis was based only on the death certificate [death certificate-only (DCO)]. Of all the cancer cases registered in 2018, 5,749 cases (82.92%) were diagnosed by MV methods, including pathology or cytology. The diagnosis in 712 (10.27%) of the registered cancer cases was purely clinical or based on clinical evaluation. In 472 cases (6.81%) of registered patients, cancer diagnosis was based on DCO.
| Organs | 2014 | 2018 | ||||
|---|---|---|---|---|---|---|
| DCO | Clinical | Pathology | DCO | Clinical | Pathology | |
| Breast | 9 (1.14) | 81 (10.23) | 702 (88.64) | 25 (2.23) | 49 (4.37) | 1047 (93.40) |
| Prostate | 22 (7.91) | 82 (29.50) | 174 (62.59) | 26 (6.21) | 102 (24.34) | 291 (69.45) |
| Other skin | 6 (1.10) | 21 (3.85) | 519 (95.05) | 4 (0.69) | 11 (1.91) | 561 (97.40) |
| Colorectal | 33 (11.62) | 52 (18.31) | 199 (70.07) | 25 (4.76) | 40 (7.62) | 460 (87.62) |
| Stomach | 52 (15.71) | 48 (14.50) | 231 (69.79) | 47 (12.53) | 45 (12.00) | 283 (75.47) |
| Bladder | 6 (2.23) | 36 (13.38) | 227 (84.39) | 14 (3.81) | 18 (4.90) | 335 (91.28) |
| Thyroid | 5 (2.82) | 15 (8.47) | 157 (88.70) | 3 (0.89) | 11 (3.26) | 323 (95.85) |
| Trachea, bronchus and lung | 69 (23.00) | 81 (27.00) | 150 (50.00) | 56 (17.34) | 55 (17.03) | 212 (65.63) |
| Leukemia | 61 (62.89) | 36 (37.11) | 0 (0.00) | 35 (11.04) | 30 (9.46) | 252 (79.50) |
| Uterus | 7 (4.73) | 10 (6.76) | 131 (88.51) | |||
| Brain, nervous system | 54 (24.77) | 62 (28.44) | 102 (46.79) | 62 (21.83) | 53 (18.66) | 169 (59.51) |
| Non-Hodgkin lymphoma | 6 (2.51) | 59 (24.69) | 174 (72.80) | 20 (7.30) | 12 (4.38) | 242 (88.32) |
| O&U | 27 (9.12) | 62 (20.95) | 207 (69.93) | - | - | - |
| All sites | 436 (7.91) | 1037 (18.82) | 4036 (73.26) | 472 (6.81) | 712 (10.27) | 5749 (82.92) |
Abbreviations: DCO, death certificate-only; O&U, other and unspecified.
4.5. Age Distribution of Cancer Incidence
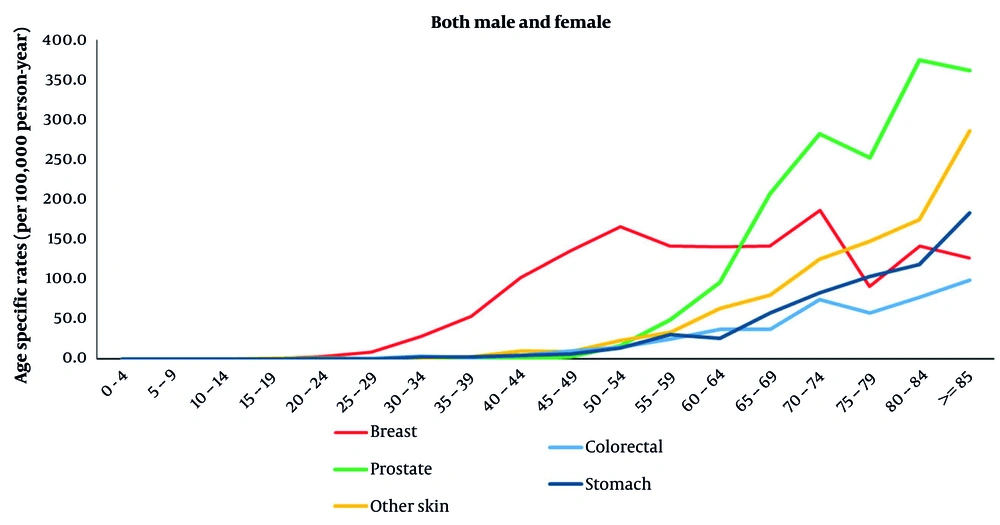
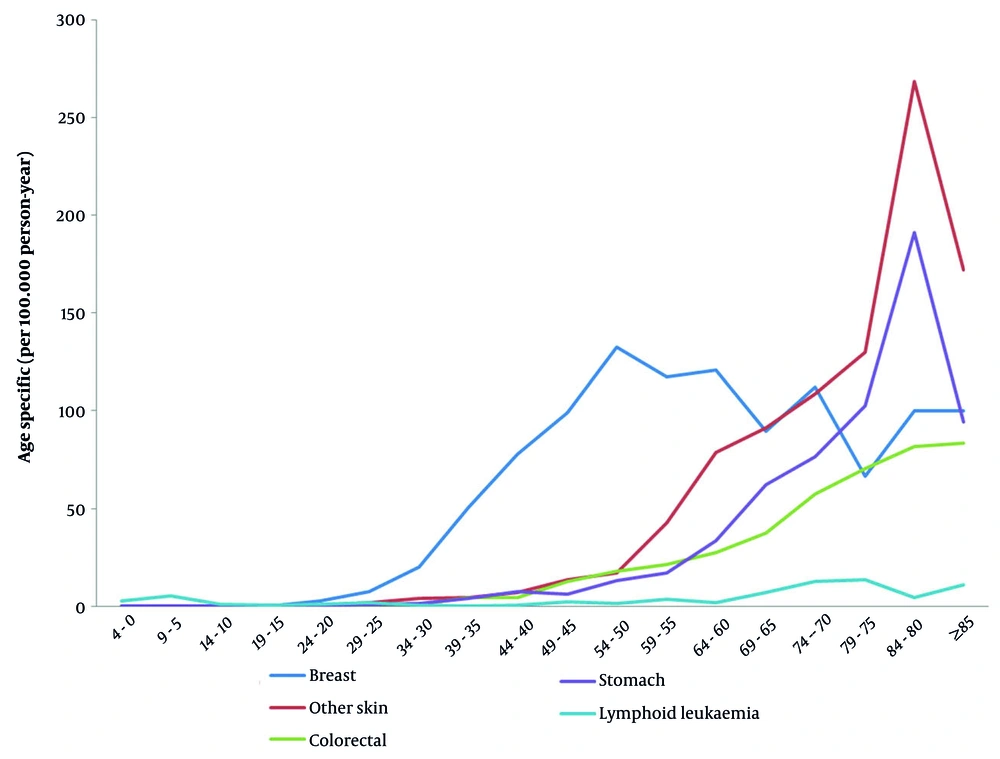
The results in Table 4 show that the highest ASRs for stomach, lung, other skin cancers, prostate, colon, bladder, and brain cancers among patients aged 80 to 84 years were 190.9, 136.63, 268.18, 159.09, 81.82, 113.64, and 63.64 per 100,000 people, respectively. The highest incidence rate was for breast cancer in the age group of 60 to 64 years, uterus cancer in 70 - 74, ovarian cancer in 75 - 79, thyroid cancer in 75 - 79, lymphoma in 70 - 74, and blood cancer in the age group of 75 to 79 years, with incidence rates of 120.69, 2.13, 16.22, 18.92, 32.43, and 13.51 per 100,000 people, respectively (Figure 2). The results in Table 5 show that in 2018, the highest age-standardized incidence of lung, uterus, ovary, prostate, lymphoma, and blood cancers was related to the age group of 80–84 years, with incidence rates of 148.42, 16.62, 375.36, 59.37, and 22.26 per 100,000 people. The highest ASRs for colon cancer, melanoma, other skin cancers, bladder, and other and unspecified (O&U) cases were associated with the age group of 85 years and above, reported as 98.65, 14.09, 286.56, 159.72, and 79.86 per 100,000 people, respectively. The highest incidence rates of stomach and brain cancer were observed in the age group of 75 - 79 years, with incidence rates of 103.96 and 43.77 per 100,000 people, respectively. The highest age-standardized incidence of breast and ovarian cancers was recorded in the age group of 70 - 74 years, with incidence rates of 186.76 and 52.78 per 100,000 people, respectively (Figure 3).
| Organs | Total Number | Percent | Age (y) | |||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 0-4 | 5 - 9 | 10 - 14 | 15 - 19 | 20 - 24 | 25 - 29 | 30 - 34 | 35 - 39 | 40 - 44 | 45 - 49 | 50 - 54 | 55 - 59 | 60 - 64 | 65 - 69 | 70 - 74 | 75 - 79 | 80 - 84 | ≥ 85 | |||
| Stomach | 331 | 6.01 | 0.21 | 0.00 | 0.00 | 0.00 | 0.00 | 0.92 | 1.26 | 4.18 | 7.56 | 6.25 | 12.95 | 17.28 | 33.63 | 62.32 | 76.60 | 102.70 | 190.91 | 94.44 |
| Trachea, bronchus and lung | 300 | 5.45 | 0.21 | 0.24 | 0.00 | 0.25 | 0.20 | 1.29 | 0.84 | 1.67 | 2.41 | 4.58 | 21.24 | 18.52 | 37.17 | 52.17 | 55.32 | 100.00 | 136.36 | 105.56 |
| Other skin | 546 | 9.91 | 0.21 | 0.00 | 0.00 | 0.25 | 0.61 | 1.66 | 3.98 | 4.46 | 7.22 | 13.75 | 17.10 | 42.59 | 78.76 | 91.30 | 108.51 | 129.73 | 268.18 | 172.22 |
| Breast | 778 | 29.66 | 0.00 | 0.00 | 0.00 | 0.00 | 2.83 | 7.61 | 20.08 | 50.56 | 77.62 | 99.15 | 132.63 | 117.50 | 120.69 | 89.47 | 112.00 | 66.67 | 100.00 | 100.00 |
| Uterus unspecified | 22 | 0.40 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.18 | 0.00 | 0.00 | 1.37 | 1.25 | 2.07 | 2.47 | 1.77 | 2.90 | 2.13 | 0.00 | 0.00 | 5.56 |
| Ovary | 77 | 1.40 | 0.42 | 0.00 | 0.27 | 0.25 | 0.00 | 0.74 | 0.84 | 3.06 | 4.12 | 2.50 | 4.15 | 3.09 | 6.19 | 8.70 | 8.51 | 16.22 | 0.00 | 0.00 |
| Prostate | 278 | 5.05 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.69 | 1.67 | 8.29 | 16.05 | 39.82 | 53.62 | 72.34 | 148.65 | 159.09 | 133.33 |
| Colorectal | 284 | 5.16 | 0.00 | 0.00 | 0.00 | 0.00 | 0.20 | 1.10 | 0.84 | 4.46 | 4.47 | 12.92 | 18.13 | 21.60 | 27.43 | 37.68 | 57.45 | 70.27 | 81.82 | 83.33 |
| Bladder | 269 | 4.88 | 0.00 | 0.00 | 0.00 | 0.25 | 0.20 | 0.37 | 1.68 | 1.39 | 3.09 | 5.42 | 15.03 | 22.84 | 29.20 | 40.58 | 59.57 | 100.00 | 113.64 | 72.22 |
| Brain, nervous system | 218 | 3.96 | 3.14 | 2.39 | 1.36 | 1.26 | 2.03 | 2.03 | 2.73 | 3.90 | 6.19 | 7.08 | 8.29 | 9.26 | 18.58 | 15.94 | 12.77 | 27.03 | 63.64 | 38.89 |
| Thyroid | 177 | 3.21 | 0.00 | 0.00 | 0.00 | 0.76 | 3.25 | 5.89 | 3.56 | 7.80 | 5.84 | 5.42 | 6.74 | 5.56 | 5.31 | 10.14 | 10.64 | 18.92 | 9.09 | 11.11 |
| Non-Hodgkin lymphoma | 239 | 4.34 | 1.89 | 3.11 | 1.36 | 1.01 | 2.64 | 2.76 | 1.89 | 2.51 | 4.47 | 10.42 | 11.92 | 14.20 | 21.24 | 18.84 | 40.43 | 32.43 | 31.82 | 16.67 |
| Lymphoid leukemia | 97 | 1.76 | 2.94 | 5.26 | 0.82 | 0.76 | 0.81 | 1.66 | 0.63 | 0.28 | 0.69 | 2.50 | 1.55 | 3.70 | 1.77 | 7.25 | 12.77 | 13.51 | 4.55 | 11.11 |
| Organs | Total Number | Percent | Age (y) | |||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 0 - 4 | 5 - 9 | 10 - 14 | 15 - 19 | 20 - 24 | 25 - 29 | 30 - 34 | 35 - 39 | 40 - 44 | 45 - 49 | 50 - 54 | 55 - 59 | 60 - 64 | 65 - 69 | 70 - 74 | 75 - 79 | 80 - 84 | ≥ 85 | |||
| Stomach | 375 | 5.41 | 0.00 | 0.00 | 0.00 | 0.00 | 0.27 | 0.00 | 2.58 | 3.07 | 4.79 | 6.23 | 13.94 | 30.40 | 26.21 | 57.52 | 83.48 | 103.96 | 118.74 | 183.21 |
| Colorectal | 329 | 4.75 | 0.00 | 0.00 | 0.00 | 0.00 | 0.27 | 0.60 | 3.87 | 1.89 | 4.79 | 9.89 | 14.93 | 24.77 | 37.13 | 36.81 | 74.69 | 57.45 | 77.92 | 98.65 |
| Trachea, bronchus and lung | 323 | 4.66 | 0.00 | 0.00 | 0.00 | 0.00 | 0.27 | 0.60 | 1.11 | 0.94 | 2.24 | 6.59 | 10.95 | 20.83 | 36.40 | 49.46 | 85.68 | 65.66 | 148.42 | 136.23 |
| Melanoma of skin | 25 | 0.36 | 0.00 | 0.00 | 0.00 | 0.00 | 0.27 | 0.20 | 0.37 | 0.00 | 1.28 | 0.00 | 3.48 | 0.56 | 0.73 | 2.30 | 2.20 | 2.74 | 3.71 | 14.09 |
| Other skin | 576 | 8.31 | 0.00 | 0.22 | 0.00 | 0.33 | 1.89 | 0.99 | 1.84 | 3.07 | 9.91 | 9.52 | 22.89 | 33.78 | 63.33 | 80.52 | 125.22 | 147.74 | 174.40 | 286.56 |
| Breast | 1121 | 16.17 | 0.00 | 0.00 | 0.00 | 0.00 | 3.28 | 8.76 | 28.60 | 53.48 | 101.91 | 135.73 | 166.15 | 141.28 | 140.38 | 141.80 | 186.76 | 91.12 | 141.30 | 126.88 |
| Uterus unspecified | 34 | 0.49 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.37 | 0.96 | 4.54 | 2.25 | 8.10 | 6.95 | 2.96 | 4.30 | 4.06 | 0.00 | 16.62 | 0.00 |
| Ovary | 119 | 1.72 | 0.41 | 0.00 | 0.00 | 2.74 | 1.64 | 3.18 | 2.23 | 4.78 | 8.44 | 9.75 | 11.14 | 9.26 | 13.30 | 17.19 | 52.78 | 39.86 | 33.25 | 9.76 |
| Prostate | 419 | 6.04 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 2.15 | 16.63 | 49.30 | 96.13 | 207.98 | 282.45 | 252.75 | 375.36 | 362.29 |
| Bladder | 367 | 5.29 | 0.00 | 0.00 | 0.00 | 0.33 | 0.27 | 0.60 | 2.03 | 0.94 | 5.11 | 8.42 | 12.94 | 23.08 | 48.77 | 51.76 | 63.71 | 90.28 | 122.45 | 159.72 |
| Brain, nervous system | 284 | 4.10 | 4.39 | 2.64 | 1.36 | 1.67 | 1.62 | 3.18 | 3.87 | 5.90 | 5.43 | 7.33 | 12.44 | 15.20 | 14.56 | 23.01 | 26.36 | 43.77 | 29.68 | 32.88 |
| Non-Hodgkin lymphoma | 274 | 3.95 | 2.19 | 0.66 | 2.99 | 1.67 | 2.16 | 1.99 | 2.76 | 2.59 | 3.84 | 9.52 | 10.95 | 19.70 | 17.47 | 33.36 | 43.94 | 21.89 | 59.37 | 37.58 |
| Lymphoid leukemia | 142 | 2.05 | 6.58 | 3.30 | 1.63 | 2.01 | 1.62 | 0.40 | 0.74 | 0.24 | 0.96 | 1.10 | 2.49 | 7.88 | 9.46 | 13.80 | 19.77 | 8.21 | 22.26 | 4.70 |
| O&U | 246 | 3.55 | 1.00 | 0.66 | 0.82 | 1.34 | 0.54 | 1.59 | 1.84 | 2.36 | 5.11 | 3.66 | 11.94 | 16.89 | 16.74 | 32.21 | 46.13 | 41.04 | 63.08 | 79.86 |
| All sites | 6932.00 | 100.00 | 23.73 | 12.31 | 15.78 | 21.44 | 30.51 | 33.38 | 62.64 | 85.14 | 148.31 | 198.15 | 318.03 | 431.81 | 596.21 | 799.48 | 1164.35 | 1132.66 | 1543.60 | 1728.75 |
Abbreviation: O&U, other and unspecified.
The APC in ASRs from 2014 to 2018 is presented in Table 6. Prostate cancer showed the highest increase (APC = 29.5%, 95% CI: 27.1 - 32.0), followed by thyroid (APC = 15.8%) and breast cancers (APC = 8.8%). A significant decreasing trend was observed only for other skin cancers (APC = -1.0%, P = 0.012).
| Top Most Common Cancers | APC (%) | 95% CI | P-Value |
|---|---|---|---|
| Organ | 8.8 | 7.9 - 9.7 | < 0.001 |
| Breast | 29.5 | 27.1 - 32.0 | < 0.001 |
| Prostate | -1.0 | -1.8 - -0.2 | 0.012 |
| Other skin | 2.2 | 1.1 - 3.3 | < 0.001 |
| Colorectal | 0.4 | -0.5 - 1.2 | 0.380 |
| Stomach | 5.3 | 4.0 - 6.6 | < 0.001 |
| Bladder | 15.8 | 14.2 - 17.5 | < 0.001 |
| Thyroid | -0.3 | -1.2 - 0.6 | 0.520 |
| Trachea, bronchus and lung | 0.7 | -0.2 - 1.6 | 0.120 |
| Leukemia | – | – | – |
| Uterus | 5.0 | 3.8 - 6.2 | < 0.001 |
| Brain, nervous system | 2.0 | 0.9 - 3.1 | < 0.001 |
| Non-Hodgkin lymphoma | – | – | – |
| O&U | 8.8 | 7.9 - 9.7 | < 0.001 |
Abbreviations: APC, annual percent change; CI, confidence interval; O&U, other and unspecified.
The unusually low number of registered cases in 2015 (n = 2,728) is likely attributable to a temporary disruption in the provincial cancer registry system, possibly due to health information system upgrades or data transfer delays during that year. To assess the robustness of our trend estimates, we conducted a sensitivity analysis excluding 2015. The APC for overall cancer incidence remained statistically significant (APC = 3.1%, 95% CI: 2.0 - 4.2, P < 0.001), confirming that the rising trend was not driven by the 2015 dip.
Cancer registry quality indicators showed notable improvement over the study period. The proportion of MV cases increased from 73.3% in 2014 to 82.9% in 2018, while DCO diagnoses decreased from 7.9% to 6.8%, reflecting enhanced case ascertainment and diagnostic accuracy.
5. Discussion
This registry-based serial cross-sectional time-trend study, utilizing data from the Khuzestan Cancer Registry at Jundishapur University of Medical Sciences, revealed a consistent increase in registered cancer cases from 2014 to 2018. A total of 29,289 cancer cases were recorded during this five-year period, with the overall ASR rising from 150.90 to 174.18 per 100,000 population — an increase of 13.37%. This upward trend is steeper than that observed in longer-term national studies; for example, Bidhendi-Yarandi and Panahi reported a smaller increase over a 12-year period (2003 - 2015) (19). In 2014, the most common cancers by ASR were breast, other skin (non-melanoma), colorectal, and stomach cancers. By 2018, prostate cancer had risen to the second most common cancer, following breast cancer, while other skin and colorectal cancers remained among the top four. The steepest increases were observed for prostate (APC = 29.5%), thyroid (APC = 15.8%), breast (APC = 8.8%), bladder, and brain cancers. In contrast, other skin and lung cancers showed slight declines. These patterns are consistent with national trends, including the rising burden of breast cancer among Iranian women — now exceeding global estimates (20) — and underscore the urgent need for early detection and cancer control policies.
Sex-specific analyses revealed that the most common cancers among men were other skin, prostate, colorectal, and stomach cancers, while among women, they were breast, other skin, and colorectal cancers. These findings are broadly consistent with prior studies in Khuzestan (21) and other Iranian provinces (22). The majority of cancers occurred in individuals aged 70 years and older, with the exception of breast cancer, which peaked in the 60 - 64 age group. This shift may reflect Iran’s aging population and the absence of a national breast cancer screening program, leading to diagnosis at older ages. Reproductive, dietary, and obesity-related risk factors may also contribute to this trend (20, 23). Notably, the proportion of MV cases increased from 73.3% in 2014 to 82.9% in 2018, while DCO diagnoses declined from 7.9% to 6.8%. This improvement in diagnostic verification supports the reliability of our incidence estimates and is comparable to international standards (24, 25). While aging and lifestyle changes likely contribute to the rising cancer incidence, part of this increase may also reflect improved case ascertainment over time, as evidenced by the rise in MV% and the decline in DCO%.
The observed cancer incidence in Khuzestan appears to be within the higher range of previously reported provincial estimates in Iran. However, direct comparisons across provinces should be interpreted with caution due to potential differences in registry completeness, diagnostic verification rates, and data collection methodologies.
5.1. Conclusions
Cancer incidence in Khuzestan has been increasing in recent years and appears to be within the higher range of previous provincial reports in Iran. However, cross-provincial comparisons should be interpreted with caution due to potential differences in cancer registry completeness, MV rates, and DCO% proportions across regions. This rising trend underscores the urgent need for national policies to facilitate timely diagnosis, strengthen cancer control programs, and improve patient outcomes in the region. Although the current cancer registry system in Khuzestan provides reliable incidence data, it should be expanded to routinely collect additional indicators such as mortality, survival, prevalence, and key risk factors to enable comprehensive cancer surveillance and evidence-based policy-making.
5.2. Research Limitations
This study has several limitations that should be considered when interpreting the findings. First, the 5-year observation window (2014 - 2018) is relatively short for robust trend analysis, particularly for detecting long-term changes in cancer incidence. Second, the registry data did not include information on key risk factors (e.g., smoking, obesity, reproductive history) or cancer screening practices, limiting our ability to explore potential drivers of observed trends. Third, we did not have access to mortality or survival data, so we could not assess case fatality or survival outcomes. Finally, the unusually low case count in 2015 (n = 2,728) suggests potential under-ascertainment during that year, possibly due to temporary disruptions in data collection or reporting systems. Despite these limitations, our analysis provides valuable insights into recent cancer incidence patterns in Khuzestan province.