1. Background
Diabetes mellitus is a group of metabolic diseases whose common feature is an increase in blood sugar levels due to a defect in insulin secretion, a defect in its function, or both (1, 2). The World Health Organization has declared it a latent epidemic due to the increasing statistics and trends in diabetes worldwide (3-5). It is one of the most common and rapidly affecting diseases worldwide and is projected to affect 693 million adults by 2045 (6, 7). Type 2 diabetes mellitus (T2DM) is the most common type of diabetes in the world and affects approximately 90% of diabetic patients (6, 8). Diabetes causes major changes in most systems of the body and results in immediate or delayed complications of the disease. Diabetes causes disability, treatment costs, and high mortality (7-10). This disease is the ultimate cause of blindness, kidney failure, and lower limb amputation (10). More than half of all non-traumatic amputations are due to diabetes (10-14). About 10% of patients are diagnosed with neuropathy when they are diagnosed with diabetes. Diabetic sensory neuropathy is one of the causes of diabetic foot ulcers. It is estimated that the cause of foot ulcers in diabetic patients is 50 to 60% due to peripheral neuropathy, 15 to 20% due to peripheral vascular disease, and 15 to 20% due to both causes (11-13, 15). Symptoms develop in the form of tingling, burning, sometimes pain, and complete numbness in the lower extremities. Loss of sensation is a predisposing factor for wound formation (10, 13, 14).
On the other hand, activities of daily living (ADLs) are important criteria in examining the general performance of individuals. These activities include the ability to bathe, dress, and perform activities necessary for a normal, independent life (16, 17). In patients with diabetic neuropathy, the level of ADLs changes (18). In fact, people with diabetes aged 65 and over are exposed to more restrictions on their daily activities (19). Numerous studies have examined the relationship between ADLs and blood sugar control in patients with T2DM. These studies have shown that diabetes is a risk factor for mobility limitations and disabilities of patients, and in fact, it has been stated that elderly people (65 years and older) with diabetes have more restrictions on daily activities in life, which is related to the duration of diabetes and age. In these studies, it has been stated that it is not clear whether the mentioned limitations are due to high blood sugar levels or due to long-term complications of the disease. Therefore, it is not obvious to what extent correction of high blood sugar levels can help reduce disabilities (18, 20, 21). In some studies, the relationship between blood triglyceride levels and daily activity in patients has been discussed (22-24).
Identifying the relationship between the level of daily activity of patients with T2DM and blood biochemical factors can play an important role in improving the quality of life in diabetic patients, saving costs, treatment, and reducing the complications of the disease in these patients (25).
2. Objectives
The present study aimed to investigate the relationship between ADLs and blood biochemical factors in newly diagnosed patients with T2DM.
3. Methods
3.1. Study Design and Setting
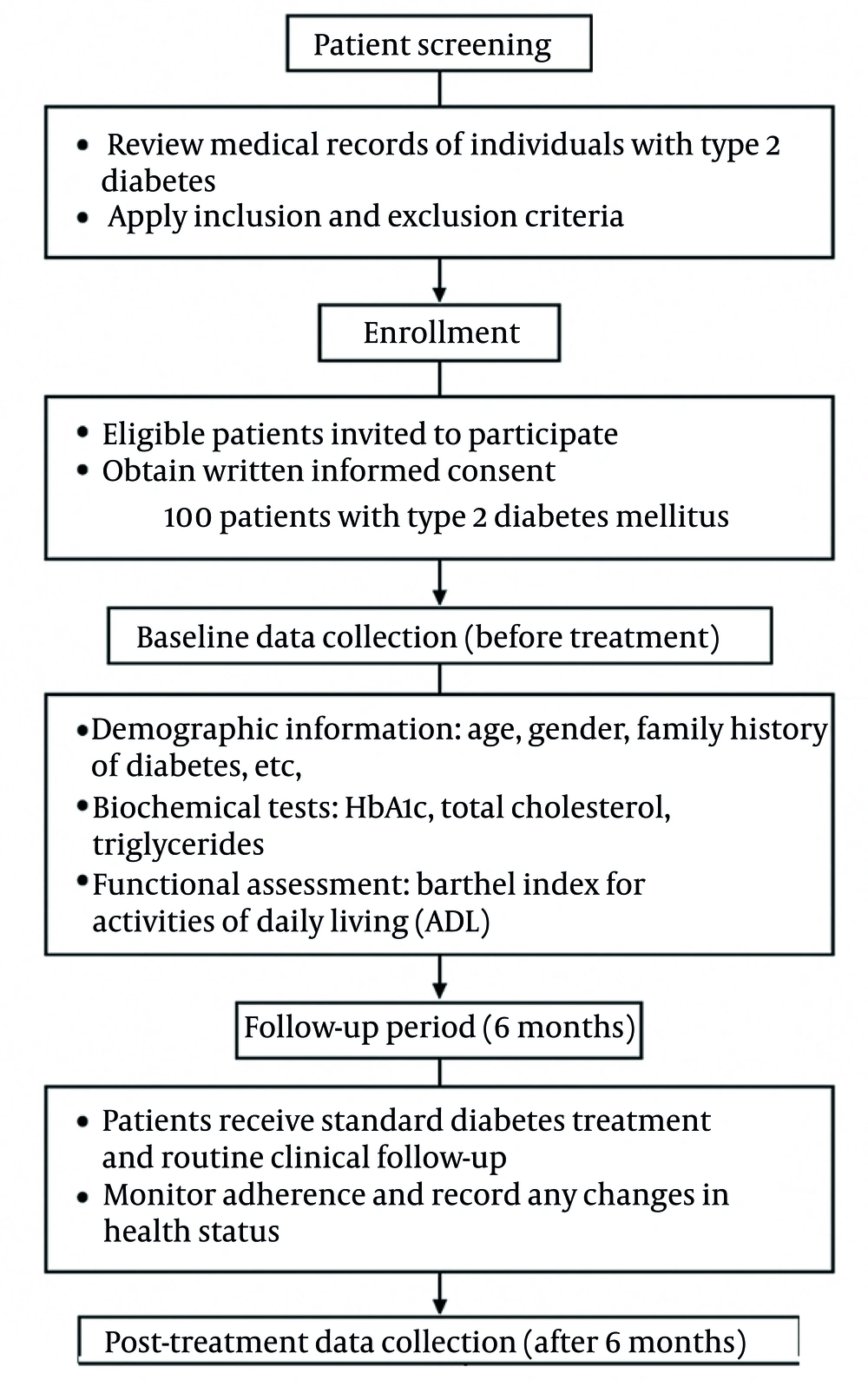
This is a prospective observational (before-after) study implemented between 2021 to 2023. The statistical population includes newly diagnosed patients with T2DM and patients that have a record in the diabetes clinic of Dr. Ganjavian Hospital in Dezful, Iran. Figure 1 shows the step-by-step implementation of the study.
3.2. Participants
Inclusion criteria included T2DM, age between 40 to 70 years, BMI range 18.5 to 24.9, weight 45 to 85, and no underlying disease affecting motor activity (hormonal problems including thyroid disorders, heart attack, coronary heart disease, liver disease, history of internal cancer requiring surgery, history of radiotherapy and chemotherapy in the past 10 years, diabetic foot ulcers, motor disease such as dystrophies, and vision). Exclusion criteria encompassed the occurrence of unexpected events during the study period such as the death of the participant and the patient’s unwillingness to continue cooperation.
Participants were selected from newly diagnosed patients. With informed consent and after providing sufficient explanations about the research, and in case the person met the conditions to enter the study, they were selected as a statistical sample of the study. The sample size is calculated based on the following formula. The sample size was determined using a two-sided test with a 95% confidence level (α = 0.05) and 80% statistical power. According to these parameters, the required sample size was calculated to be approximately 90 participants, and to compensate for possible dropouts, 100 patients were finally enrolled using simple random sampling.
3.3. Data Collection
A total of 100 samples were included in the study with two time points for data collection, so that at the same time as the start of the treatment of diabetes and 6 months later, the activity status, cholesterol, triglyceride, and glycated hemoglobin (HbA1c) levels were measured in their daily lives. The samples studied at the beginning of the research are new cases of the disease that have not yet received medication and have been re-evaluated 6 months after visiting the center. During the 6-month follow-up period, all participants received standard diabetes care, including regular medical visits, lifestyle counseling, and adjustment of antidiabetic medications as clinically indicated. The data required for this study were collected using a two-part questionnaire including demographic characteristics as well as blood biochemical factors and the standard questionnaire of Barthel’s ADLs. This questionnaire consists of 10 questions and the answers to this test are set on a 4-point scale. The questionnaire includes questions about bowel movements, urination, skin health care, toilet use, handling, mobility, dressing, stair climbing, bathing, and nutrition. The score of each of these criteria is added up and finally they are scored between zero and twenty, and the higher the score, the less dependence it shows in performing daily activities (17). The validity and reliability of this questionnaire were evaluated in the study of Khajavi and Parsa Calculation of Pearson correlation coefficient between two completions of the questionnaire was 0.97 to 0.76 for subscales 1 to 5, respectively, and it was 0.97 for the total score of the scale. Moreover, internal reliability was calculated by Cronbach’s alpha method, which gave a coefficient of 0.96, indicating the excellent internal reliability of this scale (26).
3.4. Statistical Analysis
SPSS software version 25 was used to describe the data, and numerical descriptive indicators including mean, standard deviation, and median were used. Then, the mixed model was used to investigate the relationship between the score of ADLs and laboratory levels of blood biochemical factors. Model assumptions such as normality of residuals and homogeneity of variance were examined before interpretation. A mixed model is a model that is used to examine the relationship of variables when observations are interdependent. Because the values of individuals were measured twice, the assumption of independence between observations was not established and therefore simple linear regression models could not be used. Therefore, the linear mixed model was used as an alternative. In this study, HbA1c level, blood cholesterol level, and triglyceride level as response, patients as random effects, and individual characteristics of patients including gender, age, occupation, and activity level of patients as fixed effects were included in the model. All analyses were performed at a significance level of 0.05 (P < 0.001).
4. Results
The mean age of patients was 58.5 ± 8 years and mean levels of HbA1c, cholesterol, triglyceride, and ADLs score were 7.91 ± 1.87, 166.39 ± 44.27, 164.57 ± 87.88, and 18.38 ± 1.01, respectively. Also, 42% of the patients were male and the rest were women, 62% of whom had a positive family history of diabetes (Table 1).
| Variables | Values |
|---|---|
| Age | 58.56 ± 8.82 |
| History of diabetes by year | 6.49 ± 5.31 |
| Sex | |
| Male | 42 (42) |
| Female | 62 (62) |
| Family history of diabetes | 62 (62) |
a Values are expressed as No. (%) or M±SD.
During the study, the mean blood biochemical factors decreased; HbA1c decreased from 8.10 to 7.73, triglyceride from 187.12 to 142.03, and cholesterol from 182.09 to 150.70. The amount of daily activities of life increased from 18.30 to 18.46 six months after diagnosis and treatment (Table 2). During the study, the relationship between blood factors and ADLs was investigated by controlling the age, gender, and occupation of patients and using a mixed model, according to which the amount of HbA1c had a significant correlation with ADLs score (P < 0.001) but the correlation of blood cholesterol and triglyceride with the score of ADLs was not statistically significant (P = 0.186 and P = 0.206). Accordingly, by reducing the level of HbA1c in the blood, the score of ADLs increases. In addition, the significance of the covariance parameter in all models indicates the correlation between the observations and the suitability of the mixed model for this analysis (Table 3). Frequency of measurement was also significantly associated with all three blood factors. Accordingly, with increasing HbA1c, the score of ADLs decreases.
| Variables | Time 1 (Before Treatment Initiation) | Time 2 (After 6 Month) |
|---|---|---|
| HbA1C (%) | 8.10 ± 1.85 | 7.73 ± 1.89 |
| Cholesterol (mg/dL) | 182.09 ± 46.36 | 150.70 ± 35.95 |
| Triglyceride (mg/dL) | 187.12 ± 98.55 | 142.03 ± 69.17 |
| ADL | 18.30 ± 1.09 | 18.46 ± 0.92 |
Abbreviations: HbA1C, glycated hemoglobin; ADL, activity of daily living.
a Values are expressed as M±SD.
| Variables | Coefficient | Standard Deviation | Significant Amount | 95% CI | |
|---|---|---|---|---|---|
| Lower Bound | Upper Bound | ||||
| HbA1C | -0.41 | 0.13 | 0.001 | -0.67 | -0.17 |
| Cholesterol | -6.48 | 3.17 | 0.043 | -12.75 | -0.218 |
| Triglyceride | -11.42 | 6.16 | 0.066 | -23.59 | 0.748 |
Abbreviations: HbA1C, glycated hemoglobin.
Also, the level of HbA1c, cholesterol, and triglyceride in the patients was higher in the first measurement than in the second time (taking the drug reduced the level of blood factors). In this study, patients had higher HbA1c measurements in the first time and women had more HbA1c than men (P = 0.121 and P = 241).
5. Discussion
In line with the objectives of this study, the results indicate that lower HbA1c was linked with higher ADLs scores in newly diagnosed patients with T2DM. This finding is consistent with numerous previous studies. The study conducted by Kalyani et al. (27) probes the association between diabetes and mobility disabilities in the elderly and the possible mediating role of comorbidities and HbA1c, and diabetes significantly increased the chance of developing motor disability 2 to 3 times in movement groups. In this study, it is stated that the elderly with diabetes have a higher chance of developing disability at different levels associated with comorbidities and HbA1c (27). The results of the study conducted by McGrath et al. on the relationship between grip strength and diabetes on the inability to perform ADLs in elderly Mexican Americans, are consistent with the present study, confirming that muscle weakness and diabetes are independently and jointly associated with higher rates of ADL disability in elderly Mexican Americans (18).
Some studies have suggested the role of diabetic neuropathy in reducing ADLs, and since there is a significant correlation between neuropathy, high blood sugar, and HbA1c, it is clear that if the desired HbA1c is maintained, neurological complications of diabetes (neuropathy) and the amount of ADLs can be controlled. In this regard, we can refer to the study of Ghavami et al. on the study of the relationship between diabetic neuropathy and HbA1C concentration. This study aimed to evaluate diabetic patients in terms of diabetic neuropathy and the relationship between HbA1c and diabetic neuropathy (they had HbA1c more than 9.5%) (15).
In the Ki-Wol’s study on the relationship between ADLs and biochemical variables in the elderly with diabetes mellitus, data on ADLs and biochemical variables of 76 elderly people were examined. This study showed a positive correlation between ADLs and high-density lipoprotein and a negative correlation between total cholesterol, triglyceride, and low-density lipoprotein (LDL) (19). In 2016, Han et al. conducted a cross-sectional questionnaire study to examine the correlation between daily physical activity and diabetes in the United States. The results of this study showed that in order to judge the correlation between daily physical activity and diabetes, the roles of gender, age, physical and social environment, motivation and self-efficacy, and support for successful aging for different populations should be considered (28).
In the present study, the relationship of blood cholesterol with the score of ADLs was not significant (P = 0.186). This result is not consistent with previous studies, as in the study of Hetz et al., on increased participation in ADLs by controlling low cholesterol levels in people with spinal cord injury, ADL levels were associated with lower total cholesterol and LDL (29).
This study has several limitations. First, the research was conducted in a single clinical center with a relatively small sample size, which may limit the generalizability of the findings to broader populations of patients with T2DM. Second, the study followed patients for only six months; therefore, long-term effects of blood biochemical factors on ADLs could not be fully evaluated. Future studies with larger, more diverse populations and longer follow-up periods are recommended.
5.1. Conclusions
The findings of this study indicate that higher HbA1c levels are significantly associated with reduced ADL scores in patients with T2DM. In contrast, cholesterol and triglyceride levels showed no significant association with ADL performance. These results suggest that poor glycemic control may negatively affect patients’ functional independence. Therefore, maintaining optimal HbA1c levels could play a key role in preserving daily functional abilities and preventing disability among individuals with type 2 diabetes.