1. Background
Genetically, obesity is a complex phenotype that results from intricate interactions between inherited predispositions and environmental stimuli, rather than being a simple consequence of sedentary lifestyles or unbalanced caloric intake (1-3). Genomic advances have revealed multiple genes that regulate lipid metabolism, adipocyte function, and energy control, with ATP-binding cassette transporter A1 (ABCA1) emerging as a key participant. This gene encodes a transmembrane protein that enables reverse cholesterol transport (RCT) (4), an essential process for transferring excess cellular cholesterol to high-density lipoproteins (HDL) for clearance from peripheral tissues (5). Changes in ABCA1 mRNA expression, whether due to genetic polymorphisms or environmental factors (6), can lead to impaired lipid efflux (7), aberrant lipid accumulation (8), and heightened susceptibility to metabolic diseases (9), such as obesity (10-12). In response to these findings, the focus has shifted to lifestyle interventions that may influence ABCA1 gene activity and enhance lipid homeostasis (13, 14).
Aerobic exercise, recognized for its extensive cardiovascular and metabolic advantages, has demonstrated an impact on gene expression via pathways associated with mitochondrial biogenesis (15), oxidative stress modulation, and lipid transport. Regular aerobic exercise may elevate high-density lipoprotein cholesterol (HDL-C) levels, decrease low-density lipoprotein cholesterol (LDL-C), and improve the LDL-C/HDL-C ratio by lowering LDL-C and/or increasing HDL-C, thereby mitigating risk factors linked to atherogenesis and obesity (16, 17). Furthermore, physical exercise has shown regulatory effects at the transcriptional level on genes involved in cholesterol metabolism, such as ABCA1, which may contribute to long-term changes in lipid transport dynamics.
In addition to structured exercise, bioactive substances from natural sources have attracted scientific attention for their gene-modulating effects. Green tea, abundant in polyphenolic catechins like epigallocatechin gallate (EGCG), demonstrates antioxidant, anti-inflammatory, and lipid-lowering properties (18). Clinical research indicates that green tea intake can beneficially influence blood lipid profiles by elevating HDL-C and reducing LDL-C levels (19-21). Research has shown that green tea can affect gene expression related to lipid metabolism (20, 22) and fat oxidation (23, 24), thus supporting its potential use in personalized strategies for regulating obesity-related genes (25-27). The emerging concept that combining physical exercise and dietary polyphenols may provide synergistic effects on gene expression and lipid outcomes necessitates a timely and relevant investigation of their molecular interaction (28).
Peripheral blood mononuclear cells (PBMCs) provide an effective model for evaluating alterations in gene expression in response to systemic interventions, owing to their accessibility and responsiveness to metabolic signals (29-31). Assessing ABCA1 expression in these cells, alongside HDL-C, LDL-C, and the LDL-C/HDL-C ratio, offers a comprehensive view of how external interventions may influence internal molecular pathways related to lipid transport and metabolic health (32, 33). This investigation aimed to evaluate the individual and combined effects of eight weeks of aerobic exercise and green tea supplementation (TS) on ABCA1 mRNA expression in PBMCs and related lipid markers in overweight women. To our knowledge, few randomized, double-blind, placebo-controlled trials have simultaneously investigated the combined effects of aerobic exercise and standardized green TS on ABCA1 mRNA expression and lipid markers in PBMCs of overweight women.
2. Objectives
This study addresses an important gap by integrating molecular and clinical lipid outcomes within a single intervention design.
3. Methods
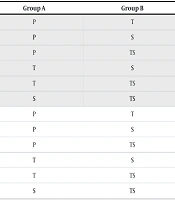
This randomized, double-blind, placebo-controlled clinical trial was designed to examine the effects of aerobic exercise and green TS on ABCA1 mRNA expression and related lipid indicators within PBMCs of overweight women. The study was duly registered with the Iranian Registry of Clinical Trials (IRCT20240618062168N1) and received approval from the Ethics Committee of Islamic Azad University (IR.IAU.DAMGHAN.REC.1403.002). All procedures adhered to the guidelines outlined in the Declaration of Helsinki. The sample size was determined using Cochran’s formula and adjusted to reflect a projected attrition rate of 20%. It was predicted that a minimum of 13 participants would be required for each group. Accordingly, a total of 60 overweight women (BMI > 25) were recruited and randomly assigned to four groups of approximately equal size through a block randomization technique. The interventions comprised (1) aerobic exercise with green TS, (2) aerobic training alone (T), (3) green TS alone (S), and (4) placebo (P), as depicted in Table 1.
| Variables | TS (n = 15) | T (n = 13) | S (n = 15) | P (n = 14) |
|---|---|---|---|---|
| Age (y) | 57.06 ± 5.14 | 61.92 ± 3.81 | 57.26 ± 4.51 | 56.78 ± 4.39 |
| Height (m) | 1.59 ± 0.05 | 1.57 ± 0.04 | 1.58 ± 0.04 | 1.60 ± 0.01 |
| Body weight (kg) | 74.30 ± 7.32 | 69.85 ± 2.60 | 73.98 ± 6.42 | 74.88 ± 5.26 |
| BMI (kg.m-2) | 29.06 ± 2.06 | 28.26 ± 1.39 | 29.35 ± 1.64 | 29.23 ± 1.35 |
a Values are expressed as mean ± SD.
Participants had to meet eligibility requirements by being free of cardiovascular, renal, metabolic, or endocrine problems and not currently using drugs or supplements that affect lipid metabolism or gene expression. Medication and supplement use were assessed using a structured medical history questionnaire and an interview conducted by a physician. Participants reporting the use of medications known to affect lipid metabolism or gene expression, such as statins, fibrates, corticosteroids, hormone replacement therapy, or other lipid-lowering agents, within the previous three months were excluded from the study. Following clinical screening and the procurement of informed written consent, all participants completed a detailed health history questionnaire and a validated physical activity assessment form. The baseline anthropometric characteristics were assessed and are detailed in Table 1.
The green TS consisted of a daily administration of one capsule of standardized green tea extract (Camellia sinensis; CAMGREEN capsules, green tea extract; Essential Plant Agriculture and Pharmaceutical Company, Gorgan, Iran), providing 500 mg of green tea extract per capsule, as stated on the manufacturer’s label. Participants consumed the capsule 30 minutes prior to lunch throughout the eight-week intervention period. Placebo capsules, which were identical in color, shape, and size, were formulated using wheat flour and produced by the Faculty of Pharmacy at Tabriz University of Medical Sciences. The supplements were distributed by a researcher who was not involved in the outcome evaluation to ensure the integrity of the blinding for both participants and investigators.
All participants received personalized dietary recommendations developed by the researcher to mitigate nutritional bias and effectively manage dietary confounders. These recommendations adhered to the Academy of Nutrition and Dietetics guidelines (34). Participants maintained a stable dietary regimen during the trial and were obligated to complete 3-day dietary recall logs and daily food records to assess compliance (35). These forms were consistently evaluated to verify that food consumption adhered to prescribed thresholds for energy and macronutrients.
Participants in the TS and T groups engaged in an aerobic training regimen designed in accordance with the guidelines of the American College of Sports Medicine (36-38), as well as protocols previously shown to be feasible and effective for overweight women in clinical exercise trials (19, 21, 39). Supervised sessions occurred three times per week for a duration of eight consecutive weeks. Table 2 delineates the workout protocol over the study's duration. Each session included a 10-minute warm-up, a primary training period that extended from 30 to 44 minutes throughout the program, and a 10-minute cool-down. The intensity of exercise was tailored to each individual and progressively increased from 55% to 75% of the maximum heart rate of each participant, continuously monitored using Polar heart rate monitors (FT4, Polar Electro, Finland). The exercise regimen comprised rhythmic, whole-body aerobic movements and was conducted under the supervision of a trained exercise physiologist to ensure standardization and participant safety, as presented in Table 2.
| Weeks | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 |
|---|---|---|---|---|---|---|---|---|
| Duration (min) | ||||||||
| Warm-up | 10 | |||||||
| Training | 30 | 32 | 34 | 36 | 38 | 40 | 42 | 44 |
| Cool-down | 10 | |||||||
| Maximum heart rate (%) | 55 | 55 | 60 | 60 | 65 | 65 | 70 | 75 |
Venous blood samples (5 mL) were obtained from the antecubital vein under fasting conditions at baseline and post-intervention. The PBMCs were extracted via Ficoll-Paque™ density gradient centrifugation (40). Following isolation, cells were rinsed with phosphate-buffered saline and preserved at -80°C until RNA extraction. Total RNA was extracted utilizing the RNeasy Mini Kit (Qiagen, Germany) according to the manufacturer's instructions (41, 42). The quantity and purity of RNA were evaluated using a NanoDrop ND-1000 spectrophotometer (Thermo Fisher Scientific, USA) (43). Complementary DNA (cDNA) was produced with the RevertAid First Strand cDNA Synthesis Kit (Thermo Fisher Scientific, USA) with oligo(dT) primers. Quantitative real-time PCR (qRT-PCR) was conducted utilizing SYBR Green master mix (Takara Bio Inc., Japan) on a StepOnePlus™ real-time PCR system (Applied Biosystems, USA) (44, 45). Relative ABCA1 mRNA levels were determined using the 2-ΔΔCt method, normalized to a housekeeping gene GAPDH (46). Gene expression changes were evaluated by comparing post-intervention measurements with baseline levels.
Plasma samples were incubated at 3000 rpm for 10 minutes and stored at -80°C until analysis. The quantification of HDL-C plasma levels and LDL-C was conducted utilizing enzymatic colorimetric assays that employed cholesterol oxidase/peroxidase methodology (47). This objective was accomplished by utilizing commercially available diagnostic kits from Randox Laboratories (United Kingdom) and Rad-Bio (Iran), following the protocols established by the manufacturers (48). These methods are widely recognized in clinical and research settings due to their high sensitivity, specificity, and reproducibility. The LDL-C to HDL-C ratio was calculated by dividing the obtained LDL-C level by the HDL-C level (49). Each measurement was performed in duplicate, and stringent internal quality control measures were implemented to ensure the reliability of the biochemical assessments.
Statistical analysis was conducted using IBM SPSS Statistics version 27. Descriptive statistics, expressed as mean ± standard deviation (mean ± SD), were employed to summarize the data collected. The outcomes following the intervention were analyzed through analysis of covariance (ANCOVA), utilizing pre-intervention values as covariates for comparisons between groups. In instances where significant differences were identified, Bonferroni-adjusted post hoc comparisons were applied. The assumption of normality was verified using the Kolmogorov–Smirnov test. All dependent variables demonstrated P-values > 0.05 at both pre- and post-intervention stages across all groups, thereby confirming normal distribution. Thus, the application of parametric analysis via ANCOVA was deemed appropriate.
4. Results
This study explores the influence of an eight-week aerobic exercise program combined with green TS on gene expression and lipid metabolism in PBMCs in overweight women. Significant differences among the intervention groups were identified through rigorous statistical analysis employing ANCOVA and Bonferroni-adjusted pairwise comparisons. These results highlight the potential synergistic effects of structured physical activity and nutritional supplementation in promoting metabolic health.
A statistically significant modulation of ABCA1 mRNA expression was observed following the interventions (F = 24.28, P < 0.001) as shown in Table 3. Women engaging in concurrent aerobic exercise with green TS demonstrated significantly increased ABCA1 expression levels (mean adjusted value 2.41 ± 0.31 AU), markedly exceeding those of the placebo (P) group (1.48 ± 0.19 AU; P < 0.001). Similarly, as indicated in Table 4, this combined intervention group exhibited significant differences compared to those who consumed only green tea in the S group (1.73 ± 0.22 AU; P < 0.001) and those who engaged solely in aerobic training in the T group (1.89 ± 0.27 AU; P = 0.003), thereby confirming the synergistic effect of integrated lifestyle modifications on the cellular mechanisms involved in lipid transport.
| Source | Sum of Squares | df | Mean Square | F | Sig. |
|---|---|---|---|---|---|
| Model | 34511.17 | 5 | 6902.23 | 418.99 | 0.000 |
| Pre-test ABCA1 | 1076.28 | 1 | 1076.29 | 65.33 | 0.000 |
| Group | 1599.61 | 4 | 399.90 | 24.28 | 0.000 |
| Error | 856.61 | 52 | 16.47 | - | - |
| Total | 35367.78 | 57 | - | - | - |
Abbreviations: ABCA1, ATP-binding cassette transporter A1.
Abbreviation: ABCA1, ATP-binding cassette transporter A1; HDL, high-density lipoproteins; LDL, low-density lipoproteins.
a Statistically significant (P < 0.001).
b Statistically significant (P < 0.05).
c Not statistically significant.
d Statistically significant (P < 0.01).
Concurrently, significant alterations were observed in essential lipid parameters, particularly in HDL cholesterol levels. Statistical analyses revealed significant response differences between groups (F = 29.16, P < 0.001), as illustrated in Table 5. The combined regimen of aerobic exercise and green TS in the TS group resulted in significant increases in HDL levels (58.2 ± 6.4 mg/dL) when compared to the placebo (P) group (49.6 ± 4.9 mg/dL; P < 0.001). As shown in Table 4, aerobic exercise significantly increased HDL levels in the T group (54.1 ± 5.8 mg/dL; P < 0.001 compared to P), whereas exclusive green TS in the S group did not result in statistically significant changes in HDL concentration relative to the P group. This indicates a selective responsiveness of HDL metabolism pathways to physical activity stimuli.
| Source | Sum of Squares | df | Mean Square | F | Sig. |
|---|---|---|---|---|---|
| Model | 102425.95 | 5 | 20485.19 | 4382.7 | 0.000 |
| Pre-test HDL | 414.71 | 1 | 414.71 | 88.72 | 0.000 |
| Group | 545.22 | 4 | 136.3 | 29.16 | 0.000 |
| Error | 243.05 | 52 | 4.67 | - | - |
| Total | 102669 | 57 | - | - | - |
Abbreviation: HDL, high-density lipoproteins.
Consistent with favorable changes in lipid profiles, low-density lipoprotein (LDL) cholesterol levels exhibited notable differences between groups (F = 19.4, P < 0.001). Participants undergoing the combined regimen in the TS group demonstrated a notable reduction in LDL levels (102.06 ± 5.3 mg/dL) compared to the placebo (P) group (132.85 ± 7.0 mg/dL; P < 0.001), as indicated in Table 6. Aerobic exercise in the T group significantly reduced LDL cholesterol levels (114.23 ± 6.1 mg/dL; P < 0.001 vs. control), while green TS in the S group also resulted in a moderate yet significant decrease in LDL, as illustrated in Table 4 (111.33 ± 5.9 mg/dL; P = 0.001 vs. P). These findings highlight the distinct effectiveness of each intervention in managing lipid abnormalities.
| Source | Sum of Squares | df | Mean Square | F | Sig. |
|---|---|---|---|---|---|
| Model | 771537.89 | 5 | 154307.58 | 4971.1 | 0.000 |
| Pre-test LDL | 12600.18 | 1 | 12600.18 | 405.9 | 0.000 |
| Group | 2414.14 | 4 | 603.54 | 19.4 | 0.000 |
| Error | 1614.11 | 52 | 31.04 | - | - |
| Total | 773152 | 57 | - | - | - |
Abbreviation: LDL, low-density lipoproteins.
The low-density lipoprotein/high-density lipoprotein (LDL/HDL) ratio, recognized as a comprehensive indicator of cardiovascular risk, further emphasized the therapeutic benefits of combined interventions. Women engaging in the TS group exhibited the most advantageous LDL/HDL ratio (2.23 ± 0.31), significantly differing from the supplementation-only S group (2.79 ± 0.27; P = 0.029) and the placebo (P) group (3.53 ± 0.34; P = 0.004). Aerobic exercise in the T group resulted in an intermediate improved ratio (2.52 ± 0.32), although it did not achieve statistical significance compared to the combined regimen in the TS group.
The results highlight the complex relationship between aerobic exercise and dietary polyphenolic compounds, indicating significant implications for therapeutic strategies focused on improving ABCA1 mRNA expression and optimizing lipid metabolism in overweight women.
5. Discussion
This study aimed to investigate the individual and combined effects of aerobic exercise and green TS on ABCA1 mRNA expression and related lipid markers, such as HDL, LDL, and the LDL/HDL ratio, in the PBMCs of overweight women. The results indicated notable molecular and biochemical changes resulting from these interventions, highlighting the importance of integrative lifestyle approaches in managing lipid dysregulation and cardiovascular risk in at-risk female populations (50, 51). The findings indicate that an integrative clinical strategy can improve health outcomes. Given the biochemical synergy observed between exercise-induced mitochondrial adaptations and the modulatory actions of green tea polyphenols, particularly EGCG, on lipid metabolism and gene regulation, such integrated interventions may offer a scalable and non-pharmacological pathway to reduce adiposity, enhance lipid transport mechanisms, and ultimately improve cardiometabolic resilience in vulnerable populations (50-52).
The present study observed a significant increase in ABCA1 mRNA expression, particularly within the group that participated in both aerobic exercise and received green TS. ATP-binding cassette transporter A1 is essential for the cholesterol efflux process to apolipoprotein A-I, serving as a key mediator in the initiation of RCT. This mechanism is crucial for mitigating intracellular cholesterol buildup, thereby significantly reducing the risk of atherosclerotic plaque formation. By promoting ABCA1-mediated efflux of cholesterol to apolipoprotein A-I and nascent HDL particles, these interventions may enhance RCT and reduce foam cell formation in the arterial wall. Such improvements in cellular cholesterol handling provide a plausible mechanistic link between the observed upregulation of ABCA1 mRNA and the favorable changes in LDL-C, HDL-C, and the LDL-C/HDL-C ratio.
Current data align with previous research indicating that aerobic exercise elevates ABCA1 mRNA expression in PBMCs and skeletal muscle through mitochondrial enhancement and redox-sensitive signaling pathways (53-55). EGCG, a prominent polyphenol found in green tea, has been shown to enhance ABCA1 mRNA expression via activating LXRα signaling and its associated transcriptional pathways (56, 57).
The observed additive effect in the combined intervention group likely indicates converging molecular pathways, both mechanical and biochemical, that enhance transcriptional responses associated with lipid clearance. An increase in HDL-C was consistently observed in both the aerobic and combined groups, with the most significant elevation noted in the combined condition. This observation supports existing evidence that moderate-intensity aerobic exercise significantly increases HDL-C levels through the enhancement of lipoprotein lipase activity, hepatic lipoprotein remodeling, and apoA-I turnover (16, 58). In this study, isolated green TS did not significantly affect HDL-C levels statistically. However, when administered in conjunction with an exercise regimen, green tea appears to modulate HDL-related pathways favorably (59). This synergistic effect may be attributable to the antioxidant and anti-inflammatory properties of green tea, which could enhance the stability and functionality of HDL particles (60, 61).
Interestingly, isolated green TS increased ABCA1 mRNA expression without producing a statistically significant rise in HDL-C. One possible explanation is that upregulation of ABCA1 in PBMCs may represent an early transcriptional adaptation that precedes measurable changes in circulating HDL-C concentrations. In addition, HDL-C levels are influenced by multiple hepatic and peripheral pathways beyond ABCA1, and the eight-week duration of the present trial may have been insufficient for these downstream processes to translate into detectable changes in systemic HDL-C. Furthermore, the variability of HDL-C and the relatively modest sample size may have limited our ability to detect small but biologically meaningful changes.
All intervention groups exhibited LDL-C reductions, with the most significant decline observed in participants receiving both interventions. This pattern corroborates previous research indicating that aerobic training enhances hepatic LDL receptor expression and clearance (62), while green tea polyphenols lower LDL-C through increased bile acid excretion and cholesterol catabolism (63). The synergistic effect can be attributed to a dual mechanism that facilitates cholesterol efflux while enhancing hepatic uptake. This interplay effectively drives down net LDL cholesterol levels.
The LDL-C/HDL-C ratio, an important indicator for forecasting cardiovascular events, exhibited significant improvement across intervention groups, especially in the combined arm (64, 65). These findings are consistent with recent evidence demonstrating that structured aerobic exercise combined with targeted nutritional strategies can significantly improve lipid profile indices, including the LDL-C/HDL-C ratio, thereby contributing to cardiovascular risk reduction (66, 67). Ratio-based lipid metrics, such as the triglyceride-to-HDL cholesterol ratio (TG/HDL-C) and the visceral adiposity index, offer a more comprehensive and physiologically relevant evaluation of cardiometabolic risk than isolated lipid parameters. These indices integrate multiple metabolic components and demonstrate greater sensitivity to early pathophysiological changes, making them more effective for detecting risk and monitoring responses to lifestyle or therapeutic interventions (68).
The present findings clarify the molecular and metabolic adaptability resulting from lifestyle changes (13, 28, 50). The integration of aerobic exercise with green TS yields various advantages, including the upregulation of protective gene expression, enhancement of lipid transport, and alteration of biochemical profiles towards an anti-atherogenic condition (19, 20, 52). A comprehensive approach that integrates physical conditioning with functional nutrition may therefore serve as a viable and scalable intervention for improving public health outcomes.
This study has several limitations that should be considered when interpreting the findings. First, the sample consisted exclusively of overweight middle-aged women, which limits the generalizability of the results to men, younger individuals, and other ethnic or clinical populations. Second, the intervention period was limited to eight weeks, which may be sufficient to detect short-term changes in ABCA1 mRNA expression and lipid profile but does not allow evaluation of the long-term sustainability of these effects. Third, although standardized dietary recommendations were provided and 3-day dietary recalls and daily food records were collected, we did not perform detailed quantitative dietary analyses, nor did we measure triglycerides, waist circumference, or body composition as additional cardiometabolic outcomes. These omissions restrict our ability to fully characterize changes in central adiposity and the complete lipid profile. In addition, the relatively modest sample size may have limited the statistical power to detect small but potentially meaningful changes in some outcomes, particularly HDL-C in the supplementation-only group. Finally, we assessed ABCA1 mRNA expression in PBMCs but did not measure ABCA1 protein levels or functional cholesterol efflux, so our conclusions are limited to transcriptional adaptations rather than confirmed changes in protein abundance or transporter activity.
In conclusion, the combined approach of aerobic exercise and green TS provides a well-supported, non-pharmacological intervention for enhancing lipid metabolism. This strategy also influences the gene expression pathways pertinent to cardiovascular health, suggesting a synergistic effect on metabolic and cardiovascular profiles. These interventions function at cellular and systemic levels, addressing essential biological mechanisms, including cholesterol transport and oxidative balance. Their incorporation into personalized healthcare strategies may provide a viable approach for mitigating metabolic risk in overweight individuals and enhancing long-term cardiometabolic resilience.