1. Context
Male sexuality is a multifaceted physiological phenomenon and plays a significant role in overall quality of life. Normal sexual performance requires the harmonious interaction of several body systems, including the nervous, cardiovascular, endocrine, and reproductive systems (1). Changes in physical systems or psychological factors can disturb a man’s sexual life. Sexual dysfunction in men is not a single illness, but rather a problem that can appear at any stage of sexual activity, such as desire, erection, penetration, or ejaculation (2). Research indicates that approximately 31% of men experience some form of sexual dysfunction (3). Among older men, 30 - 52% suffer from varying degrees of sexual dysfunction, with 54% facing one or more sexual health problems lasting three months or longer (4, 5). In Iran, 35.6% of men report having sexual issues, with erectile dysfunction (ED) being the most common, ranging from 14% to 87.7% (6, 7). Social stigma and feelings of embarrassment often prevent men from seeking help for these conditions (8). Although various treatments for sexual dysfunction are available (9), many men still refrain from seeking assistance (10). A contributing factor is adherence to societal expectations of masculinity, which often hinders men from reaching out for medical support (11).
Male sexual dysfunction (MSD) can affect various aspects of life, including physical health, mental well-being, self-esteem, and intimate relationships. Sexual satisfaction, an essential human right, is closely linked to overall health and well-being (12, 13). When sexual function is impaired, it can lead to diminished satisfaction and negatively influence self-esteem, relationships, and mental health (14). Conversely, good sexual health can enhance overall well-being, improve relationship satisfaction, and contribute to a better quality of life (15). Sexual dissatisfaction can lead to serious issues, such as relationship problems, family conflicts, infidelity, and divorce, and may even contribute to higher rates of criminal behavior and mental health disorders (16-24). As such, MSD represents a significant concern for many men (25).
Despite the high prevalence of sexual dysfunction, particularly among younger men who may lack a primary care physician (26, 27), many men are hesitant to seek care due to the stigma surrounding ED (28, 29). In response to these challenges, telemedicine services have rapidly expanded, especially during the COVID-19 pandemic, providing an alternative means of addressing sexual health concerns. Telehealth is now a crucial component of men's healthcare (30). Telemedicine offers numerous advantages, such as increased accessibility, affordability, confidentiality, and convenience, overcoming barriers such as geographic limitations (31-33). Healthcare providers can remotely diagnose, treat, and monitor patients, using modern communication technologies to complement in-person consultations (34). Studies have shown that telemedicine is effective in addressing various aspects of MSD, including ED (35, 36), with internet-based therapies such as cognitive behavioral therapy proving beneficial in treating ED (37).
Despite the high prevalence and significant impact of MSD on quality of life, many affected men do not seek or receive timely and effective treatment due to factors such as stigma, limited access to specialized healthcare, and geographic barriers. Telemedicine, as an emerging digital health approach, offers a promising solution by providing convenient, accessible, and confidential care. However, despite growing interest, evidence regarding the effectiveness of telemedicine interventions specifically for managing MSD remains scarce and fragmented.
2. Objectives
This systematic review aims to critically evaluate and synthesize existing research on telemedicine-based management of MSD, identifying current knowledge gaps and guiding future high-quality studies to optimize patient outcomes and healthcare delivery in this domain.
3. Methods
3.1. Data Sources
The research question was prepared following the population, intervention, comparison, and outcome (PICO) methodology (Table 1). The present review complies with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) 2020 guidelines (38), and its protocol was prospectively registered in PROSPERO under the unique identifier CRD420250632730.
| Items | Statement |
|---|---|
| P (population) | Men aged 18 and older diagnosed with any type of sexual dysfunction, including ED, PE, low libido, or sexual dissatisfaction; studies including men with comorbidities such as diabetes, hypertension, and cancer will also be considered. |
| I (intervention) | Telemedicine-based interventions, such as online consultations with healthcare providers, video therapy sessions, and mobile health apps designed to improve sexual health. These interventions may include educational content, lifestyle advice, and behavioral therapies. |
| C (comparison) | Traditional in-person or group treatments that do not involve telemedicine. |
| O (outcomes) | Primary outcomes: Improvements in sexual function assessed using validated tools, including: The IIEF, The PEDT, and self-reported measures of libido; secondary outcomes: Patient satisfaction. |
| Type of studies | Articles on high-quality RCTs regarding telemedicine interventions for MSD |
Abbreviations: ED, erectile dysfunction; PE, premature ejaculation; IIEF, International Index of Erectile Function; PEDT, Premature Ejaculation Diagnostic tool; RCT, randomized controlled trial; MSD, male sexual dysfunction.
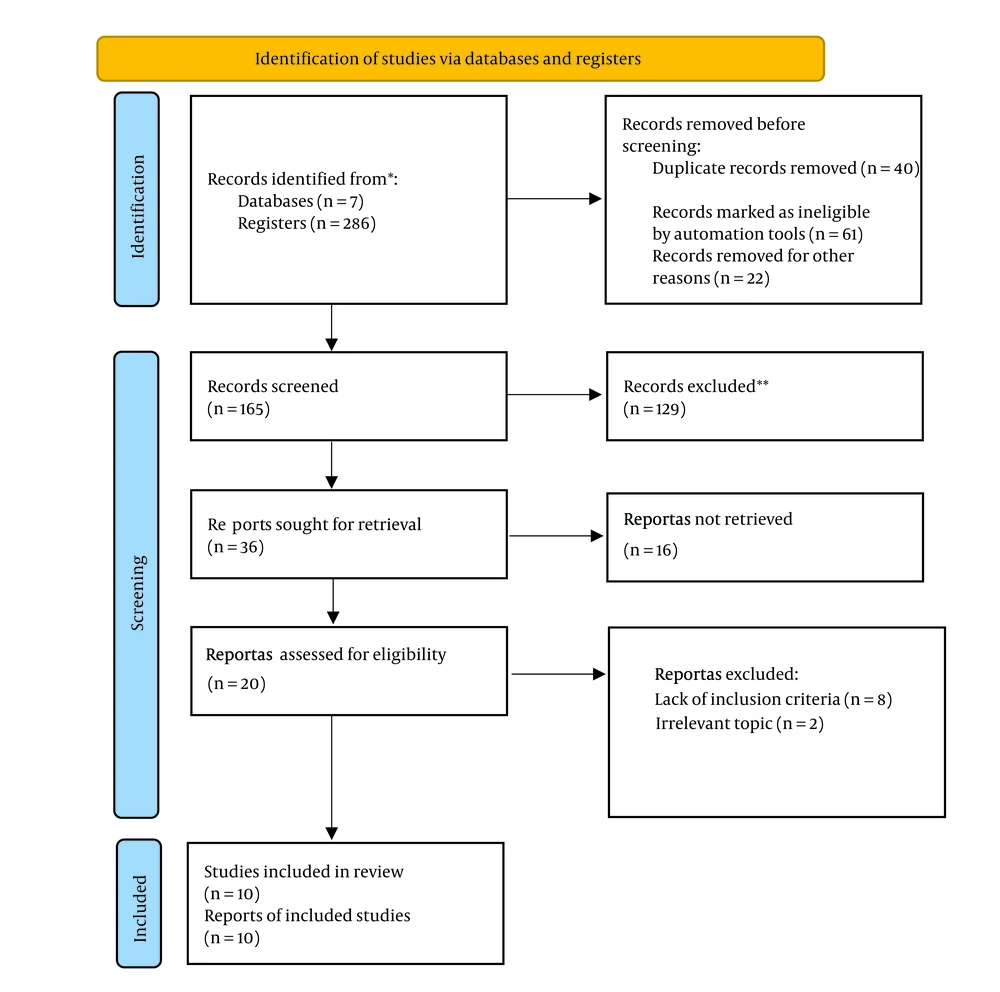
A comprehensive search was conducted across seven electronic databases from 2006 to January 30, 2025. Database-specific search strategies were developed and executed, with detailed syntax provided in Table 2 and results presented in Table 3. In addition, the entire literature search process up to the final decision on the number of studies included in this review is depicted in Figure 1 using the PRISMA Flowchart.
| Database | Search Date | Search Strategy | Records Identified |
|---|---|---|---|
| PubMed | Jan 30, 2025 | ["Telemedicine"(Mesh) OR "Digital Health"(Mesh) OR "Telehealth" OR "Remote Health"] AND ["Sexual Dysfunction, Physiological"(Mesh) OR "Erectile Dysfunction"(Mesh) OR "Premature Ejaculation"(Mesh)] AND ["Men"(Mesh) OR "Male"(Mesh)] | 85 |
| Scopus | Jan 30, 2025 | [(telemedicine OR "digital health" OR telehealth) AND ("sexual dysfunction" OR "erectile dysfunction" OR "premature ejaculation") AND (men OR male)] | 78 |
| WOS | Jan 30, 2025 | [(telemedicine OR "digital health" OR telehealth) AND ("sexual dysfunction" OR "erectile dysfunction" OR "premature ejaculation") AND (men OR male)] | 62 |
| Science Direct | Jan 30, 2025 | (telemedicine AND "sexual dysfunction" AND men) | 18 |
| Google Scholar | Jan 30, 2025 | telemedicine "sexual dysfunction" men | 25 |
| SID | Jan 30, 2025 | ("Telemedicine" OR "Digital Health") AND ("Sexual Dysfunction" OR "Erectile Dysfunction") AND ("Men" OR "Males") | 12 |
| Magiran | Jan 30, 2025 | ("Telemedicine" AND "Sexual Dysfunction" AND "Men") | 6 |
Abbreviation: SID, The Society for Information Display; WOS, Web of Science.
| Author Name, Country (Publication Year) (Reference) | Design | No. of Participants | Intervention | Control Group | Intervention Duration | Intervention Provider | Follow-up | Outcome | Main Findings |
|---|---|---|---|---|---|---|---|---|---|
| Kliesch et al., Germany (2024) (39) | RCT | 241 | Digital health application (EDDIG study) | Continue current ED management (control group) | 12 wk | Physicians | At baseline and end of study | Erectile function, quality of life, patient activation | Participants who received the intervention experienced significant enhancements in erectile function (measured by IIEF-5), overall quality of life (QOL-Med), and self-management capabilities (PAM-13), compared to those in the control group (P < 0.0001). |
| Zarei et al., Iran (2020) (40) | RCT | 70 | Mobile-based educational intervention on sexual-marital life for men with spinal cord injury | Spinal cord injury men | 8 wk | Health specialist | Baseline, 4- and 8-weeks post-intervention | Sexual adjustment, satisfaction, marital satisfaction | Notable increases in both sexual satisfaction and marital satisfaction were observed at 4- and 8-weeks post-intervention (P < 0.001). However, no statistically significant changes were found in marital adjustment at these time points (P = 0.16 and P = 0.25, respectively). |
| van Lankveld et al., Netherlands (2009) (41) | RCT | 98 | Internet-based sex therapy | Waiting-list control group | 3 mo | Sex therapists | Pre-, post-, and follow-up at 3 and 6 months | Erectile functioning, PE, sexual desire, overall satisfaction, and self-confidence | The intervention led to significant enhancements in erectile function (P < 0.05), sexual satisfaction (P < 0.001), and sexual self-confidence (P < 0.05). However, no significant changes were observed in the PE group. |
| Rahimi et al., Iran (2020) (42) | RCT | 60 | App-based group for men with spinal cord injury | Lecture-based sexual education group | 2 mo | Health specialist | Pre-, post-, and follow-up at 6 weeks | Sexual satisfaction | Significant increase was observed in sexual satisfaction in the app-based group compared to lecture-based group (P < 0.05). |
| Schover et al., United States (2012) (43) | RCT | 115 couples | Internet-based CAREss intervention, email contact | Traditional face-to-face counseling | 12 wk | Therapist | Baseline, post-waitlist, post-treatment, 3, 6, 12 months | Sexual function and satisfaction | A notable improvement in sexual satisfaction was observed in the app-based intervention group compared to the lecture-based group (P < 0.05). Significant positive effects on sexual function and satisfaction were found following both internet-based and face-to-face counseling methods (P < 0.05). |
| Wootten et al., Australia (2017) (44) | RCT | 142 | Self-guide online psychological intervention (MRA + Forum) | MRA only and Forum-only | 10 wk | Web-delivered | Pre-, post-, and follow-up at 3 and 6 months | Erectile function, total sexual satisfaction | The MRA + Forum group experienced a significant enhancement in sexual satisfaction (P = .004). Improvements in sexual function and self-esteem were key factors contributing to this increased satisfaction. |
| Fagerkvist et al., Sweden (2024) (45) | RCT | 278 | Self-help, web-based intervention for sexual problems in young adults treated for cancer | Wait-list control | 12 wk | Web-delivered | Pre-, post-, and follow-up at 3 months | Satisfaction with sex life, body image, emotional distress, quality of life, self-efficacy | There was no statistically significant difference in satisfaction with sex life between groups (P > 0.05). However, the intervention group reported significantly lower levels of vaginal dryness and emotional distress compared to the control group (P < 0.05). |
| Optale et al., Italy (2020) (46) | RCT | 35 (IG = 17, CG = 18) | Mobile coaching app exercises | TAU | 15 sessions daily | Smartphone-delivered | Pre- and post-assessments | PE | The app group showed significant improvements in both the PE Diagnostic Tool and Profile scores compared to the TAU group (P < 0.01). |
| Andersson et al., Sweden (2011) (37) | RCT | 78 | Web-based program with email support | Active control group (online forum) | 7 wk | Therapist | Pre-, post-treatment, and 6 months follow-up | Erectile function | Significant improvement in erectile function in the treatment group compared to the control group at post-treatment (P < 0.05). |
| McCabe et al., Australia (2008) (47) | RCT | 31 (IG = 12, CG = 19) | Internet-IMI | Control group | 10 wk | Therapist | Pre-, post-, and follow-up at 3 months | Erectile function, marital satisfaction, sexual satisfaction, self-esteem, relationship | The treatment group demonstrated a significant enhancement in erectile function compared to the control group after the intervention (P < 0.05). Additionally, the treatment group showed significant improvements in both erectile function and the quality of sexual relationships (P < 0.01). |
Abbreviations: RCT, randomized controlled trial; ED, erectile dysfunction; IIEF-5, International Index of Erectile Function-5; QOL-Med, Quality of Life Questionnaire-Medical Version; PAM-13, patient activation measure-13; PE, premature ejaculation; MRA, mindfulness-based relaxation approach; TAU, treatment as usual; IMI, internet-mobile intervention.
3.2. Study Selection
The inclusion criteria for this review required articles to meet the following criteria: (1) Articles examining the effectiveness of telemedicine for the management of MSD in peer-reviewed journals; (2) all electronically published randomized controlled trial (RCT) studies in peer-reviewed journals; (3) published in English and Persian; (4) relevant outcomes defined and reported using the PICO framework (Table 1); (5) provision of sufficient data for quality appraisal.
Studies were excluded for the following reasons: (1) Quasi-experimental and other non-randomized study designs were excluded to minimize selection and confounding biases, thereby focusing on the highest available level of evidence; (2) studies published in conference proceedings, non-original research (including books, review articles, theoretical works, letters to the editor, commentaries, opinions, meta-analyses, and reports), case studies, and those focusing on gay or bisexual men were excluded from this analysis.
3.3. Screening Method and Removal of Irrelevant Articles
Two reviewers (J. G. and Z. K.) independently screened the titles and abstracts of the studies identified in the search. In cases of disagreement between the two reviewers, the final decision was made by a third reviewer (K. H. M.). The data extraction form included key details such as titles, objectives, and conclusions of the relevant studies.
3.4. Data Extraction
In this systematic review, to facilitate understanding of the content from the eligible studies, key information was organized into a table format. The Methods section was expanded to provide a detailed description of the data extraction process. Specifically, data extraction was performed independently by two reviewers (J. G. and K. H. M.) using a standardized data extraction form developed a priori. This form included specific fields: Study characteristics (author, year, country), participant demographics (age, sample size), intervention details (type, duration, frequency), and outcome measures. Outcome measures were categorized as primary and secondary. The primary outcomes focused on improvements in sexual function, assessed using validated instruments: The International Index of Erectile Function (IIEF) for ED, the Premature Ejaculation Diagnostic tool (PEDT) for PE, and self-reported measures for libido. Secondary outcomes included patient satisfaction with the intervention. Each field was clearly defined, and coding schemes were applied to systematically categorize qualitative and quantitative data. Discrepancies between reviewers were resolved through discussion or consultation with a third reviewer. The finalized dataset was then used for qualitative synthesis. All findings were categorized according to the review objectives.
3.5. Quality Assessment
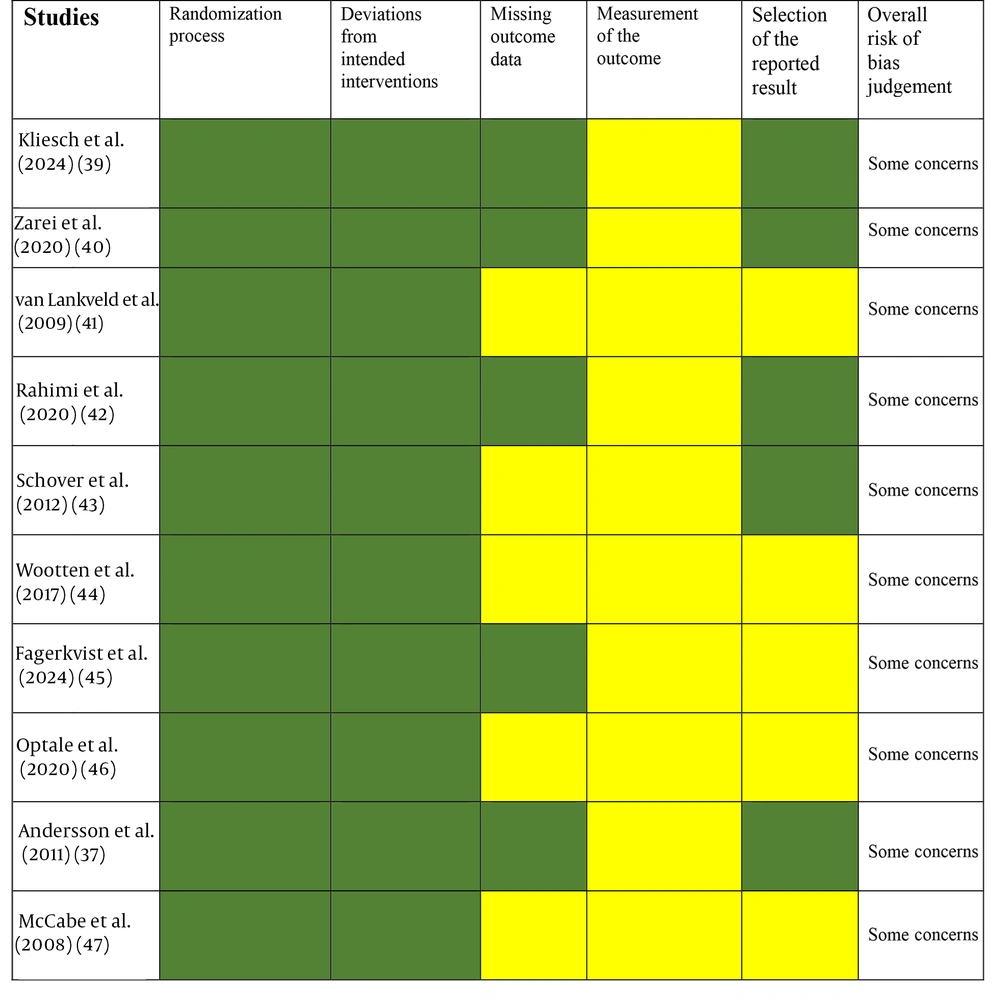
The methodological quality of the included studies was independently assessed by two reviewers (J. G. and K. H. M.) using the Critical Appraisal Skills Programme (CASP) checklist (11 items) (48) for RCTs. Each “Yes” response was assigned 1 point, while “No” or “Can’t tell” responses received 0 points. The total score ranged from 0 to 11. Studies were categorized as high quality (9 - 11), moderate quality (6 - 8), or low quality (≤ 5). Detailed quality assessments are presented in Table 4. The overall risk of bias (RoB) for each study was judged using the Cochrane RoB 2 tool (48), evaluating bias across five domains: (1) Bias arising from the randomization process, (2) bias due to deviations from intended interventions, (3) bias due to missing outcome data, (4) bias in measurement of the outcome, and (5) bias in selection of the reported result. Studies were categorized as having “low risk of bias”, “some concerns”, or “high risk of bias” based on these domain assessments. The results of the RoB assessment were reviewed and approved by all authors, incorporating feedback from external reviewers. Detailed quality assessment is presented in Figure 2.
| Studies | CASP Questions | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Q1 | Q2 | Q3 | Q4 | Q5 | Q6 | Q7 | Q8 | Q9 | Q10 | Q11 | |
| (Kliesch et al., 2024) (39) | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y |
| (Zarei et al., 2020) (40) | Y | Y | Y | Y | N | Y | Y | Y | Y | Y | Y |
| (van Lankveld et al., 2009) (41) | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y |
| (Rahimi et al., 2020) (42) | Y | Y | Y | Y | N | Y | Y | Y | Y | Y | Y |
| (Schover et al, 2012) (43) | Y | Y | Y | Y | N | Y | Y | Y | Y | Y | Y |
| (Wootten et al., 2017) (44) | Y | Y | Y | Y | N | Y | Y | Y | Y | Y | Y |
| (Fagerkvist et al., 2024) (45) | Y | Y | Y | Y | N | Y | Y | Y | Y | Y | Y |
| (Optale et al., 2020) (46) | Y | Y | Y | Y | N | Y | Y | Y | Y | Y | Y |
| (Andersson et al., 2011) (37) | Y | Y | Y | Y | N | Y | Y | Y | Y | Y | Y |
| (McCabe et al., 2008) (47) | Y | CT | Y | Y | N | Y | Y | Y | CT | Y | Y |
Abbreviation: CASP, Critical Appraisal Skills Programme.
a Record ‘Yes’, ‘No’, or ‘Can’t tell’ in response to the questions.
4. Results
The systematic search across four databases [Web of Science (WOS), Google Scholar, Scopus, and PubMed] identified 286 records. After removing 40 duplicates and 61 records marked as ineligible by automation tools, 165 records underwent title and abstract screening. During this stage, 129 records were excluded due to irrelevant topic focus. From the remaining 36 records sought for retrieval, 16 were excluded based on irrelevant abstracts or inability to retrieve the full text. The remaining 20 full-text articles were thoroughly assessed for eligibility. Of these, 10 studies were excluded for the following reasons: Eight studies failed to meet the inclusion criteria, and two studies were deemed irrelevant upon full-text examination. Ultimately, 10 studies met all eligibility criteria and were included in the qualitative synthesis. The study selection process is detailed in the PRISMA flow diagram (Figure 1).
4.1. Characteristics of the Included Studies
The eligible studies were conducted in several countries, with a total of 10 studies meeting the inclusion criteria. These studies originated from Germany (n = 1) (39), Iran (n = 2) (40, 42), the USA (n = 1) (43), Australia (n = 2) (44, 47), Italy (n = 1) (46), the Netherlands (n = 1) (41), and Sweden (n = 2) (37, 45). The publication years ranged from 2008 to 2024. The studies evaluated the effectiveness of various digital and web-based interventions such as online counseling, mobile applications, and telehealth platforms aimed at improving sexual function, marital satisfaction, and patient self-efficacy. Sample sizes ranged from 31 to 278 participants, with intervention durations spanning from 4 weeks to 12 months. Outcomes were measured using validated tools such as IIEF-5. These studies varied in their design specifics and intervention modalities, which are summarized in Table 3.
4.2. Risk of Bias of the Included Studies
The overall RoB was assessed using the Cochrane RoB tool. Ten studies raised some concerns, primarily related to measurement of outcomes (39, 47) and selection of reported results (41, 44-47)and missing outcome data (41, 43, 44, 46, 47). No studies showed high RoB. These concerns may be related to factors such as blinding or incomplete outcome data. Overall, the studies included in this review generally provided reliable evidence; however, the presence of some concerns in the majority of studies should be noted as a potential limitation. The detailed assessment is presented in Table 4. Assessment using the Cochrane RoB tool was indicated in Figure 2.
4.3. Effect of Interventions
Several studies assessed the effectiveness of various telemedicine-delivered psychological, educational, and behavioral interventions for managing MSD. These interventions were delivered via mobile applications, web-based, internet-based, or hybrid platforms and primarily targeted outcomes such as erectile function, sexual satisfaction, sexual confidence, and sexual desire.
4.3.1. Psychological Interventions
Five studies evaluated psychological interventions, including cognitive-behavioral therapy (CBT), psychodynamic therapy, and mindfulness approaches, many of which were provided through online or hybrid platforms. Two CBT-based studies (37, 43) demonstrated significant improvements in erectile function (IIEF-5; P < 0.05), sexual satisfaction [Sexual Satisfaction Scale (SSS); P < 0.01], and sexual self-confidence [Sexual Self-confidence Scale (SECS); P < 0.05]. Psychodynamic therapy (46) led to significant enhancement in PE control and sexual satisfaction (P < 0.05). Similarly, a mindfulness-based intervention (39) significantly improved erectile function and sexual desire after treatment.
4.3.2. Educational Interventions
Four studies investigated educational approaches, including sexual health education and psychoeducation, often delivered via telemedicine tools. Among spinal cord injury patients (40, 42), sexual health education significantly improved sexual satisfaction in both studies (P < 0.001), with additional gains in marital satisfaction and sexual adjustment in one study each (P < 0.05). In cancer survivors, two psychoeducational interventions (44, 45) also demonstrated significant improvement in sexual satisfaction (P < 0.05).
4.3.3. Behavioral Interventions
Two studies explored behavioral strategies, such as sensate focus and pelvic floor muscle training, delivered through online guidance. Sensate focus (41) resulted in significant improvements in erectile function, sexual desire, and sexual self-confidence (P < 0.05), though no significant effect was observed for PE. Pelvic floor exercises (39) significantly enhanced erectile function (P < 0.05).
4.4. Telemedicine Delivery Platforms
Different telemedicine modalities were used to deliver these interventions. Mobile applications (39, 40, 46) showed consistent improvements in erectile function, sexual satisfaction, and PE (P < 0.05). Web-based platforms (41, 45) had mixed results — while one study (41) showed significant improvement across all assessed outcomes, another (45) reported no significant change in sexual satisfaction. Internet-based platforms (37, 40, 44, 46) consistently demonstrated significant improvements in erectile function, PE, sexual satisfaction, and self-confidence (P < 0.05). Hybrid approaches (43) also reported significant gains in sexual function and satisfaction (P < 0.05).
Overall, the findings indicate that telemedicine-based interventions, particularly those integrating psychological and educational components, are effective in improving key aspects of male sexual function and satisfaction. These results support the growing role of digital health tools in addressing sexual dysfunction among men, offering accessible and effective alternatives to traditional face-to-face therapy.
5. Discussion
This systematic review provides comprehensive evidence supporting the effectiveness of telemedicine-based interventions in managing MSD. Drawing from ten RCTs published between 2008 and 2024, the review demonstrates that multidisciplinary interventions — particularly those integrating psychological, educational, and behavioral components — effectively improve multiple dimensions of male sexual health, including erectile function, sexual satisfaction, sexual self-confidence, sexual desire, and relational outcomes.
5.1. Effectiveness Across Intervention Types
Psychological interventions consistently emerged as among the most effective therapeutic approaches. The CBT produced marked improvements in erectile function, sexual satisfaction, and self-confidence (37, 43). These findings align with earlier systematic reviews that identified CBT as a key approach for promoting adaptive emotional and behavioral change by reshaping unhelpful thoughts and responses (49). Mindfulness-based programs (39) also enhanced erectile function and sexual desire, likely by fostering greater body awareness and emotional self-regulation. By cultivating present-moment attention and self-acceptance, mindfulness encourages individuals to shift focus away from distressing memories or anticipated performance issues toward current sensory experiences (50). The present findings support previous reviews confirming the positive influence of mindfulness on sexual functioning (51). Psychodynamic therapy contributed to improved control over PE and enhanced relational satisfaction, underscoring the therapeutic value of addressing deep-seated psychological conflicts (46).
Educational and psychoeducational strategies — particularly among men dealing with chronic health conditions such as spinal cord injury or cancer (40, 42, 44, 45) — were associated with higher levels of sexual satisfaction. This supports prior research indicating that accurate sexual education helps dispel misconceptions, provides reliable information, and leads to improved sexual well-being (52).
Behavioral interventions, such as sensate focus (41) and pelvic floor muscle training (39), produced significant gains in both physiological and psychosocial outcomes. Sensate focus techniques enhanced erectile capacity, desire, and self-confidence, while pelvic floor training improved erectile performance. These findings are consistent with reviews highlighting the dual benefits of behavioral methods (53). Earlier systematic reviews primarily focused on in-person psychological and behavioral interventions and reported improvements in erectile function, sexual satisfaction, and self-confidence (49, 51). Our findings extend this evidence by showing that telemedicine-based and hybrid interventions can achieve comparable or even enhanced outcomes, while overcoming barriers such as geographic distance, stigma, and limited access to specialized care (53, 54). Similarly, prior reviews highlighted the effectiveness of educational and psychoeducational interventions in improving sexual function and sexual satisfaction (53-59), which our study fully supports through digital delivery methods.
Overall, this review provides updated evidence that technology-supported interventions are effective, feasible, and scalable, supporting their integration into routine clinical practice for MSD.
5.2. Methodological Considerations and Limitations
Most included studies were rated as “some concerns” using the RoB 2 tool, primarily due to self-reported outcomes and limited blinding. No study was rated as high risk. Heterogeneity in intervention type, duration, and outcome measures, as well as short follow-up periods, limited the ability to perform meta-analysis and draw conclusions about long-term effects. Reliance on self-reported data introduces potential bias. Future studies should use standardized outcome measures, objective assessments, and longer follow-up periods.
5.3. Clinical Implications and Future Directions
Multidisciplinary and telemedicine-based interventions offer comprehensive, patient-centered care for men with sexual dysfunction. Clinicians can integrate these digital strategies into routine practice to enhance accessibility, reduce stigma, and improve continuity of care. Future research should focus on large-scale trials with standardized outcomes, longer follow-up, diverse populations, cost-effectiveness analysis, partner involvement, and long-term adherence to establish optimal telemedicine models for male sexual health.
5.4. Conclusions
This systematic review demonstrates that telemedicine-based interventions are effective and feasible for managing MSD. Multidisciplinary approaches, combining psychological, educational, and behavioral strategies, consistently improved erectile function, sexual satisfaction, sexual self-confidence, and sexual desire. Digital platforms — including mobile, web-based, and hybrid modalities — offer accessible, cost-effective, and flexible alternatives to conventional face-to-face interventions, particularly benefiting men with limited access to specialized care or those concerned about stigma.