1. Background
Premenstrual syndrome (PMS) is characterized by recurrent, moderate-to-severe affective, physical, and behavioral symptoms that develop during the luteal phase of the menstrual cycle and disappear within a few days of menstruation (1). The PMS refers to symptoms that women can experience during the weeks before menstruation. The symptoms of PMS differ among women and can vary from month to month. The most prevalent symptoms of PMS include mood swings, crying, depression, trouble concentrating, feeling upset, anxious or irritable, social withdrawal, fatigue or difficulty sleeping, and decreased libido, which are the major psychological symptoms. The main physical symptoms include bloating or abdominal pain, tender breasts, headache, blotchy skin, greasy hair, changes in appetite such as food cravings, constipation or diarrhea, and weight gain (2). Anger and irritability are among the most persistent PMS-induced symptoms, with women often complaining of anger before menstruation (3).
The exact cause of PMS remains unknown. Despite this, natural fluctuations in hormone levels, especially estrogen and progesterone, likely induce such symptoms 1 or 2 weeks before menstruation. Severe or debilitating PMS symptoms are uncommon and may signal an underlying medical condition. In patients with severe symptoms of PMS, consultation with a physician is required (4). On average, most women in their 30s experience PMS (5). Depression is a major problem among PMS patients. Additionally, aggression, anger, and oversensitivity, which can lead to conflicts, divorces, murders, and suicides, are observed more in such individuals. Another issue for women with PMS is stress and its consequences. Regardless of its origin, stress makes women prone to such symptoms (6).
A 2017 study on women during perimenopause reported that although 75% experienced at least one symptom of PMS, only 8% to 20% met the clinical criteria for a PMS diagnosis (7). In Iran, a 2014 study in Ilam reported the frequency of PMS disorder to be 36.11% (moderate and severe). Analyzing the 19 symptoms of the disorder, the maximum mean was obtained for tiredness, physical symptoms, trouble concentrating, decreased interest in household chores, and anger (8). Currently, some treatments have been proposed to control and reduce the psychological symptoms of this disorder, such as stress management and the use of relaxation techniques, including deep breathing or meditation, which can help regulate PMS-induced emotional disorder (9).
A study performed in Iran stated that the set of psychophysical symptoms of this syndrome, which occurs in most women of reproductive age, results in an obvious decline in their performance and quality of personal, family, and social life. On the other hand, reduced PMS symptoms lead to an increased quality of life (10). Moreover, some studies revealed that the continuation of this disorder causes increased attempts to commit suicide, fragility in performing assignments and work, seeking medical care for physical symptoms, social isolation (11), and incompatibility in family relationships (12). This disorder is a subset of psychological disorders that influence medical conditions, and psychological, social, and biological factors play a role in its etiology; this disorder progresses to premenstrual dysphoric disorder (PMDD) in its chronic state.
The psychological factors in the outbreak or exacerbation of PMS are important. Considering that various studies have indicated psychological variables such as childhood adversity (13, 14), anger (3, 6), social support (15, 16), perceived sex role (17, 18), attitude towards menstruation (19, 20), and stress (6, 13) are related to PMS, no study has been found to show whether this syndrome as a dependent variable can be predicted by the mentioned psychological variables.
2. Objectives
Therefore, the present study was designed and conducted to predict PMS in female university students based on anger, social support, childhood adversity, stress-related factors, menstrual attitudes, and sex role satisfaction.
3. Methods
The study was a cross-sectional analytical-descriptive study that included all female undergraduate and PhD students at Mazandaran University of Medical Sciences (MAZUMS) in 2023. The inclusion criterion was having an undergraduate or general doctorate (doctor of medicine, pharmacy, nursing, midwifery, health science, etc.) degree. A random stratified sampling method was used to select the samples from each faculty. The sample size was calculated using the formula for comparing a proportion against a known value. Based on a previous study (7), the prevalence of PMS among the female students was estimated as 68.9% (P = 0.689). Considering the significance level (α) of 0.05, the statistical power (1-β) of 95%, and the margin of error (d) of 0.1, the minimum required sample size was calculated as 278 participants.
Accordingly, 281 undergraduate and PhD students were selected from each faculty based on the proportion of female students in that faculty relative to the total number of university females. The cluster sampling method (with each class considered as a cluster) was then used to select the sample within each faculty. For this purpose, 5 to 10 classes (depending on the number of classes in each faculty) were randomly selected as the clusters. The questionnaire link was then provided to the representatives of the selected classes. The students in each class first completed the informed consent form attached to the questionnaire in Google Forms. The collected data were analyzed using SPSS version 26 and statistical tests.
3.1. Data Collection Tools
The research tool included 10 questionnaires provided to the study participants:
3.1.1. Demographic and Medical Questionnaire
This included questions about age, BMI, education, type of faculty, residence status, father’s education, mother’s education, birth rank, regular menstruation in recent cycles, menstrual problems, and history of menstrual problems in immediate family members.
3.1.2. Premenstrual Syndrome Symptom Screening Tool
Developed by Steiner et al. (2003) and psychometrically appraised (21). In Iran, Siahbazi et al. evaluated this scale on randomly selected girls living in Tehran University dormitories. Face, qualitative, and quantitative content validity methods were used. The CVR and CVI of the instrument were calculated as 0.7 and 0.8, respectively, indicating its quantitative content validity. Internal reliability was reported as α = 0.9. This tool contains 19 questions in two parts: Fourteen questions about emotional, physical, and behavioral symptoms, and five questions indicating the impact of symptoms on people’s lives. Each question was scored from 0 to 3: Never, mild, moderate, and severe. Three conditions indicate moderate or severe PMS: (1) At least one of options 1 to 4 is moderate or severe; (2) at least 4 items must be moderate or severe from options 1 to 14 in addition to the previous item; and (3) each of the last 5 options should be moderate or severe. Scores from the 19 questionnaire options were summed (22).
3.1.3. Spielberger State-Trait Anger Expression Inventory
Developed and psychometrically evaluated by Spielberger in 1985, including 57 items, 6 scales, and 5 subscales. Anger expression is scored on a 4-option scale from “1 = Not at all” to “4 = Very much” (23). Scores range from 10 to 40, with higher scores indicating more anger. In Iran, this study was performed on 1140 students at Tehran University and evaluated by Khodayarifard et al. The scale’s validity was checked, with criterion validity of the multifaceted anger tool and its subscales for the anger trait being 0.68, 0.30, 0.51, 0.34, 0.27, and 0.31, respectively. Convergent validity was compared with the Restrained Hostility Scale and obtained as -0.03. Divergent validity was compared with the happiness scale and determined to be -0.35; for construct validity, multifactor personality was analyzed, with values of 0.06, -0.08, 0.27, -0.04, and -0.02 reported in the population of girls (24).
3.1.4. Multidimensional Scale of Perceived Social Support
Developed by Zimet et al. in 1988, it measures three sources of social support: Family (FA), significant others (SO), and friends (FR) based on 4 items each (total 12 items). The Multidimensional Scale of Perceived Social Support (MSPSS) has scores ranging from 1 (absolutely disagree) to 7 (absolutely agree). Scores range from 12 to 84, with higher scores indicating more perceived social support. The total score and each subscale score were calculated by summing the items and dividing by the number of items in that scale (25, 26). The scale’s psychometric properties were performed and accepted by Besharat in Iranian samples (742 people: 311 students and 431 public) in 2017. Cronbach’s alpha for the total scale and the three social support subscales, FA, SO, and FR, were 0.91, 0.87, 0.83, and 0.89, respectively, verifying the internal consistency coefficients of the MSPSS (27).
3.1.5. Ten-Item Personality Inventory
Designed by Gosling et al. in 2003 and psychometrically assessed, based on a five-factor model (FFM) of personality dimensions that includes 10 questions, with scores ranging from 10 to 70. Personality dimensions are scored on a 7-option scale from “1 = strongly disagree” to “7 = strongly agree.” The inventory measures five personality traits: Extroversion, agreeableness, conscientiousness, emotional stability, and openness to experience (28). Each trait is measured by two consecutive questions (28, 29). The number of questionnaire items for each personality type was: Extroversion (1, 6), agreeableness (2, 7), conscientiousness (3, 8), emotional stability (4, 9), and openness (5, 10). Questions 2, 4, 6, 8, and 10 were reverse scored (27). Developed by Azkhosh et al. for the elderly Iranian population of 160 people aged over 60 years, the test and post-test reliability (ICC = 0.92, P = 0.00) and convergent validity (r = 0.411, P < 0.00) were psychometrically measured in Iran (29).
3.1.6. Adverse Childhood Experiences Abuse Short Form
Designed in 2012 as 8 questions adopted from the questionnaire (ACE-IQ) by the World Health Organization from its original 43-item questionnaire, developed to measure ACEs in different cultures and countries (30). The short Persian version was developed by Chegeni et al. for 494 students at Kerman University of Medical Sciences, including 8 dimensions scored on a 4-option scale. Statements ranged from “Very much (score 3)” to “Never (score 0),” with scores ranging from 0 to 24. Four questions asked about sexual abuse, and four about physical-emotional abuse. The internal consistency coefficient was 0.77 for the sexual abuse factor and 0.75 for the physical-emotional abuse factor, with a reliability index of 0.73 (31).
3.1.7. Stress-Related Factors Scales
3.1.7.1. Coping Inventory for Stressful Situations
Short version designed by Endler and Parker (1994), covering 21 questions and three subscales: Task-oriented coping, emotion-oriented coping, and avoidance-oriented coping, with 7 items each. A higher score indicates the person’s preferred coping strategy. Each question is scored on a 5-point scale from “Never (1)” to “Very much (5),” with scores ranging from 21 to 105 (32). Questions 1, 3, 6, 11, 12, 13, and 18 concern task-oriented coping; questions 2, 5, 7, 10, 14, 17, and 20 concern emotion-oriented coping; and questions 4, 8, 9, 15, 16, 19, and 21 concern avoidance-oriented coping. Each coping style comprises 7 questions (scores 7 - 35). This study was performed by Mohebbi et al. on 300 students at Shahid Beheshti University. Internal consistency for the subscales of task-, emotion-, and avoidance-oriented coping were 0.78, 0.79, and 0.79, respectively (33).
3.1.7.2. Perceived Stress Scale
Developed by Cohen et al.(34) in 1983 and shortened in 1988. Similar to its 14-item version, this 10-item version has positive (4 items) and negative (6 items) statements with reverse scoring. Scoring is on a Likert scale from never = 0 to very much = 4. Questions 4, 5, 7, and 8 (positively stated items) are reverse scored (35). The 10-item PSS had acceptable reliability (Cronbach’s alpha: 0.78). In Iran, it was psychometrically tested by Maroufizadeh et al. on 106 adults with asthma in Sanandaj. Cronbach’s alpha coefficients were 0.90, 0.90, and 0.77 for the Perceived Stress Scale (PSS-14), PSS-10, and PSS-4, respectively (36).
3.1.8. Menstrual Attitude Questionnaire
A 5-item questionnaire adopted from the Menstrual Attitude Questionnaire (MAQ) instrument, using a 7-point scale from 1 (strongly agree) to 7 (strongly disagree), including menstruation as: (1) An overwhelming event; (2) a disturbing event; (3) a natural event; (4) a predictable event; and (5) an ineffective event on individual behavior. The first two items are reverse scored. Lower scores indicate a more negative attitude toward menstruation, while higher scores indicate a more positive attitude (37).
3.1.9. Literature-Extracted Questions for Assessment
3.1.9.1. Mothers’ Feelings, Thoughts, and Behaviors Acceptance as a Woman
This visual analog scale (VAS) is composed of the following question: “To what extent do you accept your mother’s feelings, thoughts, and behaviors as a woman?” This scale ranges from 1 to 10, from “I do not accept (1)” to “I strongly accept (10)”, designed for students to answer.
3.1.9.2. Satisfaction with Sexual Role
This VAS is composed of the following question: “To what extent are you satisfied with your sexual function as a woman/girl?” This scale ranges from 1 to 10, from “not satisfied (1)” to “highly satisfied (10)”, designed for students to answer.
3.2. Statistical Analysis
To describe the variables, percentages, frequencies, means, and standard deviations were used. For hypothesis testing, the independent t-test (mean comparison of two groups), Pearson’s correlation coefficient (relationship between two quantitative variables), chi-squared test (relationship between two qualitative variables), and the Mann-Whitney test and Spearman’s correlation as nonparametric tests were used. Multivariate logistic regression (MLR) was utilized for the simultaneous relationship of all variables on the status of PMS suffering. For this purpose, the effect of each variable on the status of PMS was initially examined via univariate logistic regression (ULR), and every variable with a P-value < 0.2 in the univariate logistic model was included in the multivariate logistic model. A P-value < 0.05 was considered statistically significant for all cases of statistical analysis, and data analysis was performed using SPSS version 22.
3.3. Ethical Considerations
The study was approved by the Ethics Committee of Mazandaran University of Medical Sciences (IR.MAZUMS.REC.1402.155). All subjects were informed and completed the consent form in writing. They were assured that their participation was voluntary, their information was confidential to the researcher, and it was used for study purposes only.
4. Results
A total of 281 women participated in the study, including 93 with PMS (33.1%) and 188 without PMS (66.9%). The PMS prevalence was higher among women whose mothers had a diploma (37.6%) or less (7.5%), and lower when mothers had a bachelor’s degree (30.1% vs. 48.4% PMS-free) (χ2 = 17.47, P = 0.004). Nursing/midwifery students showed the highest PMS rates (32.3%) (χ2 = 11.78, P = 0.038). Irregular cycles were strongly linked to PMS (45.2% vs. 19.7%) (χ2 = 19.98, P < 0.001). Women with menstrual issues had markedly higher PMS prevalence (57.3% vs. 24.1%) (χ2 = 67.28, P < 0.001). The PMS sufferers more often reported a family history (31.2%) or uncertainty (53.8%) (χ2 = 26.89, P<0.001). Third-born women had elevated PMS prevalence (14.0% vs. 8.0%) (χ2 = 11.33, P = 0.014). Body Mass Index, personal education level (BSc/PhD), residence status, and father’s education showed no significant associations, though the latter approached significance (P = 0.089). Living with family and maternal education patterns were among the sociodemographic factors most associated with PMS prevalence.
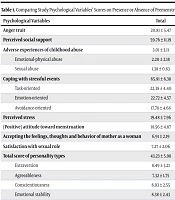
The scores of anger, adverse experiences of childhood abuse, experiences of physical-emotional abuse and sexual abuse, coping with stressful events, emotion-oriented coping, and perceived stress in individuals with PMS were generally greater than those in the other group. On the other hand, the scores for attitudes toward menstruation and satisfaction with sexual roles in those with PMS were markedly lower than those in the PMS-free group (P < 0.001) (Table 1). Concerning personality types, although the mean scores of agreeableness, conscientiousness, and emotional stability types were higher in PMS-suffering students, no significant difference was reported between the two groups in terms of personality types (P < 0.05) (Table 1).
| Psychological Variables | Total | 95% CI for Difference | PMS Suffering | PMS-free | t-Statistics | P-Value |
|---|---|---|---|---|---|---|
| Anger trait | 20.81 ± 5.47 | -6.42050 to -3.81857 | 24.24 ± 4.72 | 19.12 ± 5.44 | 7.75 | < 0.001 |
| Perceived social support | 59.76 ± 11.19 | -2.99902 to 2.59705 | 59.89 ± 11.82 | 59.96 ± 10.90 | 0.14 | 0.888 |
| Adverse experiences of childhood abuse | 3.01 ± 3.11 | -2.97043 to -1.50841 | 4.50 ± 3.28 | 2.27 ± 2.74 | 6.03 | < 0.001 |
| Emotional-physical abuse | 2.20 ± 2.18 | - | 20.30 ± 3.20 | 1.67 ± 1.96 | 5.50 | < 0.001 |
| Sexual abuse | 1.38 ± 0.83 | - | 1.45 ± 1.30 | 1.28 ± 0.60 | 3.98 | < 0.001 |
| Coping with stressful events | 65.91 ± 6.38 | -3.69608 to -.54505 | 67.33 ± 7.32 | 65.21 ± 5.75 | 2.65 | 0.009 |
| Task-oriented | 22.38 ± 4.40 | - | 22.34 ± 4.46 | 22.40 ± 4.39 | 0.11 | 0.914 |
| Emotion-oriented | 22.72 ± 4.57 | - | 24.77 ± 4.33 | 21.80 ± 4.38 | 5.36 | < 0.001 |
| Avoidance-oriented | 17.78 ± 4.68 | - | 17.29 ± 4.68 | 17.69 ± 4.06 | 1.24 | 0.217 |
| Perceived stress | 19.48 ± 7.96 | - | 23.60 ± 5.85 | 17.45 ± 8.09 | 6.54 | < 0.001 |
| (Positive) attitude toward menstruation | 18.56 ± 4.87 | 0.80171 to 3.19348 | 17.23 ± 5.03 | 19.22 ± 4.67 | 3.29 | < 0.001 |
| Accepting the feelings, thoughts and behavior of mother as a woman | 6.91 ± 2.19 | -0.499 to 0.597 | 6.88 ± 2.18 | 6.93 ± 2.20 | 0.18 | 0.860 |
| Satisfaction with sexual role | 7.27 ± 2.06 | 414 to 1.423 | 6.66 ± 2.29 | 7.57 ± 1.89 | 3.59 | < 0.001 |
| Total score of personality types | 43.23 ± 5.98 | -1.28353 to 1.70700 | 43.09 ± 4.86 | 43.30 ± 6.47 | 0.27 | 0.781 |
| Extraversion | 8.49 ± 3.21 | -0.08600 to 1.51108 | 8.02 ± 2.96 | 8.73 ± 3.30 | 1.75 | 0.080 |
| Agreeableness | 7.32 ± 1.75 | -0.84609 to 0.02477 | 7.60 ± 1.84 | 7.19 ± 1.69 | 1.85 | 0.064 |
| Conscientiousness | 8.93 ± 2.55 | -0.76154 to 0.51640 | 9.02 ± 2.75 | 8.89 ± 2.45 | 0.37 | 0.706 |
| Emotional stability | 8.38 ± 2.43 | -0.90612 to 0.30866 | 8.58 ± 2.48 | 8.28 ± 2.40 | 0.96 | 0.334 |
| Openness to experiences | 10.09 ± 2.11 | -0.19511 to 0.85743 | 9.87 ± 2.08 | 10.20 ± 2.12 | 1.23 | 0.217 |
Abbreviation: PMS, premenstrual syndrome.
a Data are presented as mean ± SD.
b Group comparisons were performed using independent samples t-test.
c A P-value < 0.05 was considered statistically significant.
By MLR, the predictor factors of PMS in university girls were tested (Table 2). There was a meaningful direct association between individual and family menstrual problems and the odds of suffering from PMS. In contrast, regular monthly habits in the last few cycles revealed a significant inverse relationship with the odds of PMS incidence. The analysis also showed a significant direct relationship between anger, perceived social support, adverse experiences of childhood abuse, coping with stressful events, and perceived stress (P < 0.05). In contrast, a meaningful inverse relationship was reported between the emotionally stable personality, the attitude toward menstruation (higher scores indicate a more positive attitude toward menstruation), and satisfaction with sexual role (higher scores indicate greater satisfaction) with PMS (P < 0.05).
| Qualitative Variables | Regression Coefficient | Standard Deviation | OR | 95% CI OR | P-Value |
|---|---|---|---|---|---|
| BMI | |||||
| Thin | Ref c | ||||
| Normal | -0.04 | 0.56 | 0.95 | 0.31, 2.91 | 0.942 |
| Overweight | -0.074 | 0.64 | 0.92 | 0.26, 3.27 | 0.929 |
| Heavy | 0.693 | 1.14 | 2.00 | 0.21, 18.68 | 0.543 |
| Education | |||||
| BSc | Ref | ||||
| PhD | -0.257 | 0.254 | 0.774 | 0.470, 1.27 | 0.313 |
| Residence status | |||||
| Living on one’s own | Ref | ||||
| Dormitory | 0.706 | 0.495 | 2.02 | 0.76, 5.34 | 0.154 |
| Living with family | 0.844 | 0.449 | 2.32 | 0.96, 5.560 | 0.060 |
| Regular menstruation in the few last cycles | |||||
| No | Ref | ||||
| Yes | -1.21 | 0.278 | 0.298 | 0.513, 0.173 | < 0.001 |
| Menstrual problems | |||||
| No | Ref | ||||
| Yes | 2.26 | 0.295 | 9.60 | 17.12, 5.38 | < 0.001 |
| Family history of menstrual problems | |||||
| No | ref | ||||
| Yes | 1.83 | 0.392 | 6.28 | 2.91, 1354 | < 0.001 |
| Not informed | 1.39 | 0.341 | 4.04 | 2.07, 7.90 | < 0.001 |
| Personality type | |||||
| Total | Ref | ||||
| Extraversion | -0.068 | 0.070 | 0.960 | 1.07, 0.81 | 0.327 |
| Agreeable | 0.128 | 0.123 | 1.07 | 1.44, 0.89 | 0.300 |
| Conscientiousness | -0.002 | 0.095 | 0.00 | 1.20, 0.82 | 0.984 |
| Emotionally stable | -0.252 | 0.097 | 6.72 | 0.94, 0.64 | 0.010 |
| Openness to experiences | 0.059 | 0.102 | 0.33 | 1.29, 0.86 | 0.563 |
| Age | 0.08 | 0.05 | 1.08 | 0.89, 1.20 | 0.123 |
| Anger | 0.178 | 0.028 | 1.19 | 1.13, 1.26 | < 0.001 |
| Perceived social support | 0.002 | 0.011 | 1.002 | 0.98, 1.02 | < 0.001 |
| Adverse childhood experiences | 0.240 | 0.046 | 1.27 | 1.16, 1.39 | < 0.001 |
| Coping with stressful events | 0.052 | 0.020 | 1.05 | 1.01, 1.09 | 0.010 |
| Task-oriented | 0.049 | 0.055 | 1.05 | 0.94, 1.17 | 0.380 |
| Emotion-oriented | 0.080 | 0.063 | 1.08 | 0.95, 1.22 | 0.201 |
| Avoidance-oriented | -0.047 | 0.049 | 0.95 | 0.86, 1.05 | 0.332 |
| Perceived stress | 0.106 | 0.018 | 1.11 | 1.07, 1.15 | < 0.001 |
| Attitude to menstruation | -0.088 | 0.028 | 0.916 | 0.86, 0.96 | 0.002 |
| Accepting the feelings, thoughts and behavior of mother as a woman | -0.010 | 0.058 | 0.990 | 0.88, 1.10 | 0.859 |
| Satisfaction with sex role | -0.216 | 0.063 | 0.806 | 0.71, 0.91 | < 0.001 |
Abbreviation: OR, odds ratio.
a Logistic regression analysis was used.
b A P-value < 0.05 is considered statistically significant.
c Ref: Reference category; the data are presented as regression coefficients with standard deviations.
5. Discussion
The study was conducted to psychologically predict PMS among students at Mazandaran University of Medical Sciences in 2023. The results showed that approximately one-third of the students had PMS. The research revealed that variables such as type of faculty, mother’s education, birth rank, regular menstruation in the last few cycles, menstrual problems, and a history of menstrual problems in immediate family members demonstrated meaningful differences between the PMS-suffering and PMS-free groups. The scores of psychological variables such as trait anger, adverse experiences of childhood abuse, coping with stressful events, emotion-oriented coping strategies, and perceived stress in individuals with PMS were significantly greater than in PMS-free students. Conversely, the mean scores of attitudes toward menstruation and acceptance of mothers’ feelings, thoughts, and behaviors as women among PMS sufferers were lower than those in the non-PMS group. Additionally, there were no meaningful differences between the mean scores of the two groups in terms of task-oriented, avoidance coping strategies, and personality type.
The findings of studies by Tarannum et al. in India and Buddhabunyakan et al. in Thailand, which aimed to discover the factors of PMS in high school students, showed that a history of menstrual problems was the most important factor in the incidence of PMS in girls (38, 39). Research by Farahmand et al. in Iran also revealed that low family income and a history of menstrual problems are factors affecting the incidence of PMS in girls (40). Additionally, mothers’ lower education and employment were related to PMS incidence (38). Rad et al. reported that, along with menstrual problems and a history of these problems in immediate family members, an individual’s nutritional status, including the consumption of fatty foods, fast food, and canned foods, increases the odds of a PMS outbreak (41). A study by Abeje and Berhanu suggested that premature menstruation and a long menstrual cycle are causes of PMS (1). These results are consistent with the current research, which revealed that menstrual problems, irregular monthly cycles, and a history of immediate family members suffering from menstrual problems are among the demographic factors pertinent to the prevalence of PMS.
Moreover, the results revealed a tangible direct relationship between anger, perceived social support, adverse experiences of childhood abuse, perceived stress, and coping with stressful events. However, a significant inverse relationship was found between attitudes toward menstruation and satisfaction with one’s sexual role and the odds of PMS suffering. Asci et al. and Hwang and Sung reported that the incidence of PMS in individuals with a positive attitude toward menstruation was lower than in those lacking a positive attitude (42, 43). Based on this study, a positive attitude toward menstruation is a negative predictor of PMS. A study by Ito et al. identified the association between a history of childhood abuse and PMS, indicating that childhood maltreatment can increase the odds of PMS incidence during menstruation (44). Wakatsuki et al. investigated the influence of childhood maltreatment, stressful life events in adulthood, and affective temperaments on psychological premenstrual symptoms in nonclinical adult volunteers. Their findings indicated that unpleasant childhood experiences and stressful life events during childhood and menstruation can lead to PMS in girls (45). Saglam and Basar investigated the relationship between anger and PMS and reported that as the anger score increased, the odds of PMS suffering increased (3). Consistent with the present study, research by Antosz-Rekucka and Prochwicz demonstrated that stress and trait anger can serve as significant psychological mechanisms in explaining PMS symptoms. Although that study examined the mediating role of attributional style, its core findings pertained to the direct and significant relationship between stress and trait anger with symptoms, confirming the findings of the current research (46). Zarei and Bazzazian also reported that increased stress and exposure to stressful events can increase the risk of PMS (47).
In various studies, the presence of menstrual problems in immediate family members was recognized as a predictor of increased PMS risk (48-50); these results align with the present research and demonstrate that various factors exist as predictors of PMS. However, in the present study, demographic factors were analyzed simultaneously with psychological factors in a comprehensive study, providing more thorough results than previous studies. Contrary to the above statements, research by Dehghan et al. to identify the relationship between PMS and personality traits among female students revealed that the personality traits of honesty-humility and agreeableness were predictors of PMS (51). In this study, individuals with an emotionally stable personality type were more likely to suffer from PMS than those with other personality types, which were not significantly related. These results were not congruent with those reported by Dehghan et al. Moreover, a study by Bertone-Johnson et al. presented a contrasting perspective, reporting that a history of sexual abuse was not consistently associated with the risk of PMS, and the association was attenuated after adjustment for social support, resulting in a non-significant higher risk of 40%. This finding is inconsistent with the present study, where a significant association between sexual abuse and PMS persisted even after adjustment for social support and other psychological variables (52). This discrepancy may be attributed to key methodological differences, notably that their analysis was part of a large longitudinal cohort with a long follow-up period, whereas our study focused on a younger population of medical students in a cross-sectional design, where the temporal proximity to trauma and a high-stress academic environment may render the effect of trauma more potent and less easily buffered by social support. Moreover, Ghasemipour et al. reported no significant differences in perceived stress and social support between girl students with PMS and normal groups (53). The main difference lies in the study design, data analysis method, and confounding variables. The first study compared the levels of these variables between groups, while the second study used a predictive model assessing the direct and indirect effects of the variables together. Furthermore, regression analysis allows researchers to see whether, for example, social support still has an effect when the impact of all other variables (such as anger, childhood adversity, attitudes toward menstruation, etc.) is held constant. Cultural differences between the two Iranian provinces, Mazandaran and Kermanshah, may account for differences in reported results. Different climatic and cultural conditions may have led to different results. Additionally, utilizing diverse instruments to measure personality traits and types in Dehghan’s study may have produced different results in these two studies. The study utilized a convenience sampling approach via Google Forms, limiting anonymity of responses, which meant researchers could not attribute data to specific classes or student cohorts (entry years).
The findings of this study can pave the way for further research in this field. Researchers can use the findings of the present study as a basis and model to conduct various descriptive and interventional studies in this area. Given that the connection between this issue and specific psychological factors has not been separately investigated in our country, and regarding the high prevalence of the condition observed in both our study and other research, it is recommended that future studies examine psychological factors in other female populations with diverse educational backgrounds. Furthermore, future work should address the development of educational interventions for managing psychological factors related to this problem.
5.1. Conclusions
The present study investigated psychological factors along with demographic and medical factors in patients with PMS. Its results can be useful in screening and providing evidence-based interventions for such patients. This study, by elucidating the interplay between psychological, demographic, and medical factors in PMS, marks a significant step toward a more comprehensive understanding of the disorder. The current findings provide a basis for more precise screening and the design of evidence-based interventions. To fully realize this potential, future longitudinal studies and controlled trials are essential to evaluate the efficacy of integrated treatment protocols developed from these insights.