1. Background
Since the 19th century, the world has experienced several industrial revolutions, each transforming production processes and resource management. The Fourth Industrial Revolution focused on digital technologies and efficiency. However, it often overlooked human needs, sustainability, and resilience, which affected employee well-being and natural resources (1-3). Industry 5.0 has emerged to address these issues, focusing on human-centered processes, collaboration between humans and machines, sustainability, and resilience (4). The emerging concept of Industry 5.0 in healthcare is known as “Healthcare 5.0”. It integrates advanced technologies into healthcare services to improve sustainability, reduce costs, and enhance patient outcomes (5).
Healthcare 5.0 represents an integrated and adaptive framework for delivering healthcare services. Hospital 5.0, as a core component of this system, focuses on enhancing patient and staff experiences through advanced technologies and human-centered processes. It serves as a central driver in achieving the goals of Healthcare 5.0 (5).
Transitioning to Hospital 5.0 can reduce healthcare costs. This can be achieved through preventive care, early interventions, smart technologies, telehealth, and robotic-assisted surgeries. These strategies enhance access to healthcare, lower system expenses, and improve public health outcomes (6).
Success in implementing Hospital 5.0 requires readiness in healthcare. This involves the hospital’s capacity for digital transformation, adoption of innovations, and optimization of resources for continuous improvement (7).
Readiness and maturity models have been examined in both Industry 4.0 and Industry 5.0 contexts. Readiness and maturity are distinct concepts. Readiness reflects an organization’s preparedness to begin implementation, while maturity indicates the level of development already achieved (8). This study focuses on readiness in defining the model’s dimensions and indicators for Hospital 5.0. However, the study also used maturity models to develop the final model and analyzed all dimensions and sub-dimensions according to the concept of readiness.
In Industry 4.0, several models have been proposed to assess readiness. For instance, the IMPULS model (9) was designed to evaluate digital transformation in the manufacturing sector. The Conform model (10) examined the readiness of construction companies for Industry 4.0 and identified human capital as the most critical success factor. Also, a readiness model for smart hospitals examined their preparedness for Industry 4.0 and assessed key factors for successful implementation (11). Another study examined digital transformation and the impact of digital technologies on management in the field of smart healthcare (12). Another quantitative study evaluated the readiness of public sector healthcare systems to adopt digital and AI technologies and examined their potential impact on productivity (13). Other studies, including the future university maturity model (14) and assessments of government organizations in Indonesia (13), have focused on technical and strategic readiness in manufacturing and service sectors. However, readiness assessments in Industry 4.0 have mainly emphasized technological and technical aspects, with limited attention to human-centered factors, employee well-being, and social and environmental considerations (15).
Readiness assessment models are generally applied in manufacturing industries, while service sectors such as hospitals have received less attention (10). Several studies have examined readiness for Industry 5.0. However, none of the existing models comprehensively address readiness for all four core dimensions of Industry 5.0 — advanced technologies, human-centricity, sustainability, and resilience (16-19).
Therefore, previous studies have mainly focused on manufacturing and technical aspects, and no comprehensive model exists that addresses all key dimensions of Industry 5.0. To fill these gaps, this study develops a practical model for hospitals, defining key readiness dimensions and indicators.
2. Objectives
The present study pursues two objectives: (1) To develop a comprehensive model to assess readiness for implementation of Hospital 5.0; and (2) to prioritize and weight its dimensions and sub-dimensions. Prioritization is important as it helps managers identify and focus on the most critical areas for effective implementation.
3. Methods
This study employed a mixed-methods approach to develop a readiness assessment model for Hospital 5.0. First, a systematic review was conducted to identify and analyze existing models and indicators from Industry 4.0 and 5.0. The systematic review served both to select a base model and to extract complementary components and indicators. In the next step, the selected base model was adapted using the best-fit framework synthesis method. This combination of methods is appropriate for this study. It ensures the model is conceptually strong and practically relevant for Hospital 5.0. Finally, the indicators of the developed model were prioritized using the grey best-worst method (GBWM).
3.1. Systematic Review
The systematic review was conducted according to PRISMA guidelines to ensure clarity and transparency. In the following sections, we describe the search strategy. All studies were independently screened by two reviewers, and any disagreements were resolved through discussion or consultation with a third reviewer when necessary.
3.1.1. Search Strategy
To identify studies related to Hospital 5.0 readiness and maturity, a systematic search was conducted in three major databases: Web of Science, Scopus, and PubMed. The applied restrictions included document type (research articles and reviews), language (English), and publication years from 2015 to 2025. The search was also purposefully limited to specific categories: Medicine, nursing, computer science, biomedical engineering, health management, and health information technology. This selection reflects the direct focus of Hospital 5.0 on clinical care, advanced technologies, and organizational management. The keywords used in the search included: “Hospital 5.0”, “Future Hospital”, “Healthcare 5.0”, “Readiness Assessment 4.0”, “Readiness Assessment 5.0”, “Maturity Assessment 4.0”, “Maturity Assessment 5.0”, “Hospital and Industry 5.0”, and “Hospital and Industry 4.0”. All studies were independently reviewed by two reviewers, and in cases of disagreement, the issue was resolved through discussion or consultation with a third reviewer.
The quality of the selected studies was systematically evaluated using the CASP framework. According to this framework, ten key domains were assessed, including study objectives, design, data collection, analysis, ethical considerations, evidence support, transparency, value, limitations, and transferability of results. The final selected studies received quality scores ranging from 8 to 10, indicating high methodological rigor and strong scientific validity.
3.2. The Best-Fit Framework
The best-fit framework is a structured approach for integrating existing frameworks and developing a practical model for a specific research context. In this study, it involved three main steps: Selecting a base framework, customizing it for Hospital 5.0, and validating the model (20, 21).
The IMPULS model (9) was selected as the base framework based on the comparative analysis of Industry 4.0/5.0 readiness models. It covers six dimensions — strategy, smart factories, smart operations, smart products, data-driven services, and employees — with detailed sub-dimensions. The model was then customized with healthcare-specific indicators and validated through expert consultation. Its comprehensive structure, focus on both technological and human aspects, and empirical support made it suitable for adaptation to Hospital 5.0.
3.3. Prioritization and Weighting of Model Dimensions and Sub-dimensions
Grey system theory, introduced by Julong in the 1980s, provides a mathematical framework for handling uncertainty in multi-criteria decision-making. It converts vague expert judgments into measurable grey numbers, enabling reliable prioritization even with incomplete information (22, 23). In this study, grey system techniques were applied to prioritize the dimensions and sub-dimensions of the proposed Hospital 5.0 readiness model, effectively managing uncertainty in expert evaluations.
The GBWM is a multi-criteria decision-making technique used to prioritize dimensions and sub-dimensions under uncertainty. Experts first identify the most (best) and least (worst) important criteria. They then make pairwise comparisons between the best criterion and others, and between all criteria and the worst, using grey numbers to capture imprecision. The method optimizes consistency between these comparisons to calculate final weights, reflecting the relative importance of each criterion (24, 25). The formulas used to derive the weights are provided in Appendix 1 in Supplementary File.
4. Results
4.1. Systematic Review
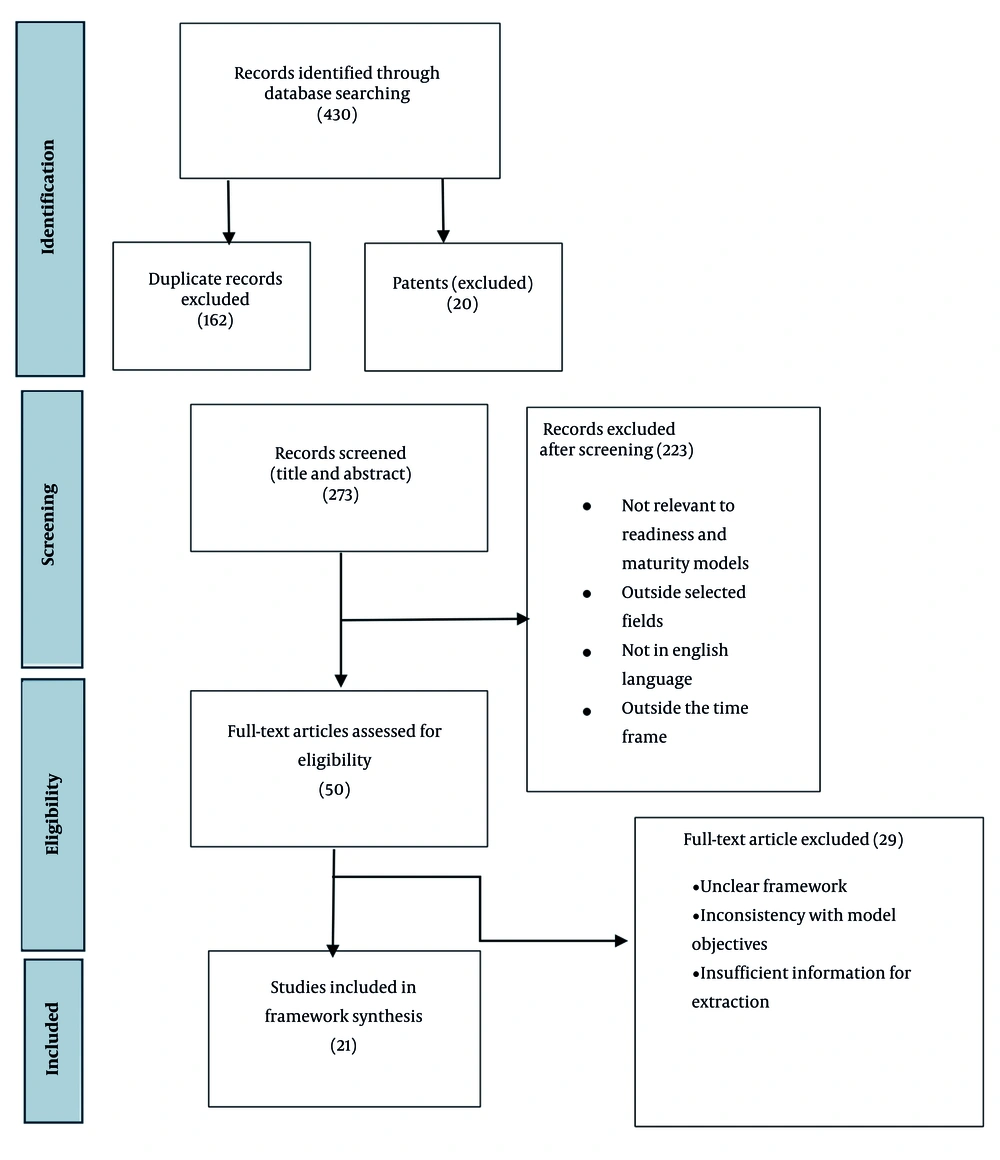
The process of identifying and selecting studies for inclusion in this systematic review is illustrated in the PRISMA flowchart (Figure 1). Initially, a total of 430 studies were identified through database searches. After removing duplicates (162 studies) and patents (26 studies), 273 studies remained for screening. After screening the titles and abstracts, 223 studies were considered potentially eligible for inclusion. A total of 50 studies were included for full-text evaluation. Subsequently, 29 of these studies were excluded. Ultimately, 21 studies were included in the final analysis. Table 1 presents the 21 included studies, including the model’s name, year, article type, and field of study.
| Model Name | Year | Field of Study | Article Type | Source |
|---|---|---|---|---|
| IMPULS Industry 4.0 readiness model | 2015 | Manufacturing and engineering | Empirical study | (9) |
| Industry 4.0 maturity/digital operations self-assessment model | 2016 | Manufacturing and engineering | Industry report/survey | (26) |
| The connected enterprise maturity model | 2014 | Manufacturing and engineering | Industry report | (27) |
| Industry 4.0 maturity model | 2016 | Manufacturing and engineering | Empirical study | (8) |
| Industry 4.0 readiness assessment model for SMEs | 2018 | SMEs | Empirical/tool development study | (28) |
| Industry 4.0 readiness model for tool management | 2017 | Tool management | Conceptual/framework | (29) |
| Industry 4.0 readiness analysis | 2018 | Manufacturing and engineering | Empirical/tool development study | (30) |
| Industry 4.0 maturity model | 2018 | Manufacturing (with potential adaptability to other industries) | Empirical | (31) |
| Health information systems maturity model | 2018 | Healthcare | Conceptual/review | (32) |
| Industry 4.0 maturity model | 2019 | Manufacturing | Empirical | (33) |
| Health information systems maturity model | 2019 | Healthcare | Empirical | (34) |
| AI innovation maturity model | 2020 | Multi-sector/not domain-specific | Conceptual | (35) |
| University 5.0 maturity model | 2020 | Education | Conceptual | (14) |
| Digital maturity assessment model for hospitals | 2021 | Healthcare | Empirical | (36) |
| Smart hospital readiness assessment model | 2022 | Healthcare | Empirical | (11) |
| Comprehensive Industry 4.0 readiness model | 2023 | Multi-sector | Empirical/mixed-method | (37) |
| Industry 4.0 maturity model for SMEs | 2022 | SMEs | Empirical | (38) |
| Quality 4.0 readiness assessment framework | 2024 | Healthcare | Empirical/mixed-method | (39) |
| Industry 4.0 readiness assessment model | 2024 | Construction/manufacturing | Empirical | (10) |
| Industry 5.0 maturity model | 2024 | Manufacturing | Empirical | (40) |
| Industry 5.0 readiness assessment | 2024 | Food industry/SMEs | Empirical | (17) |
Analysis of Table 1 shows that most of the reviewed models focus on the manufacturing industry, SMEs, or information technology. Their application in the healthcare sector is limited or indirect. Moreover, most models pertain to Industry 4.0, while dedicated models for Industry 5.0 are less developed. To date, no model has been specifically developed to assess Hospital 5.0 readiness.
4.2. The Best-Fit Framework Results
Based on the systematic review, we selected the IMPULS model as the base model in the best-fit framework. We chose it because (1) It has a comprehensive structure that connects Industry 4.0’s technology focus with human-centered goals; (2) it is widely cited and proven as a readiness (rather than maturity) model; and (3) its holistic dimensions fill gaps in other frameworks by including workforce and operational factors. Its diagnostic accuracy and empirical validation make it well-suited for assessing hospitals’ digital transformation readiness.
During the localization process, several sub-dimensions were extracted from the original IMPULS dimensions and subsequently adapted to the hospital and healthcare context. These adaptations primarily focus on technology and staff training. For instance, technological infrastructure corresponds to smart factory; emerging technologies and organizational innovation correspond to strategy and organization; security and privacy and automatization of management processes correspond to smart operations and data-driven services; advanced technology training and resource flexibility correspond to employees; change acceptance corresponds to employees and strategy and organization; telemedicine corresponds to smart product; and technological adaptability corresponds to employees and smart factory. These adaptations primarily focus on technology and staff training.
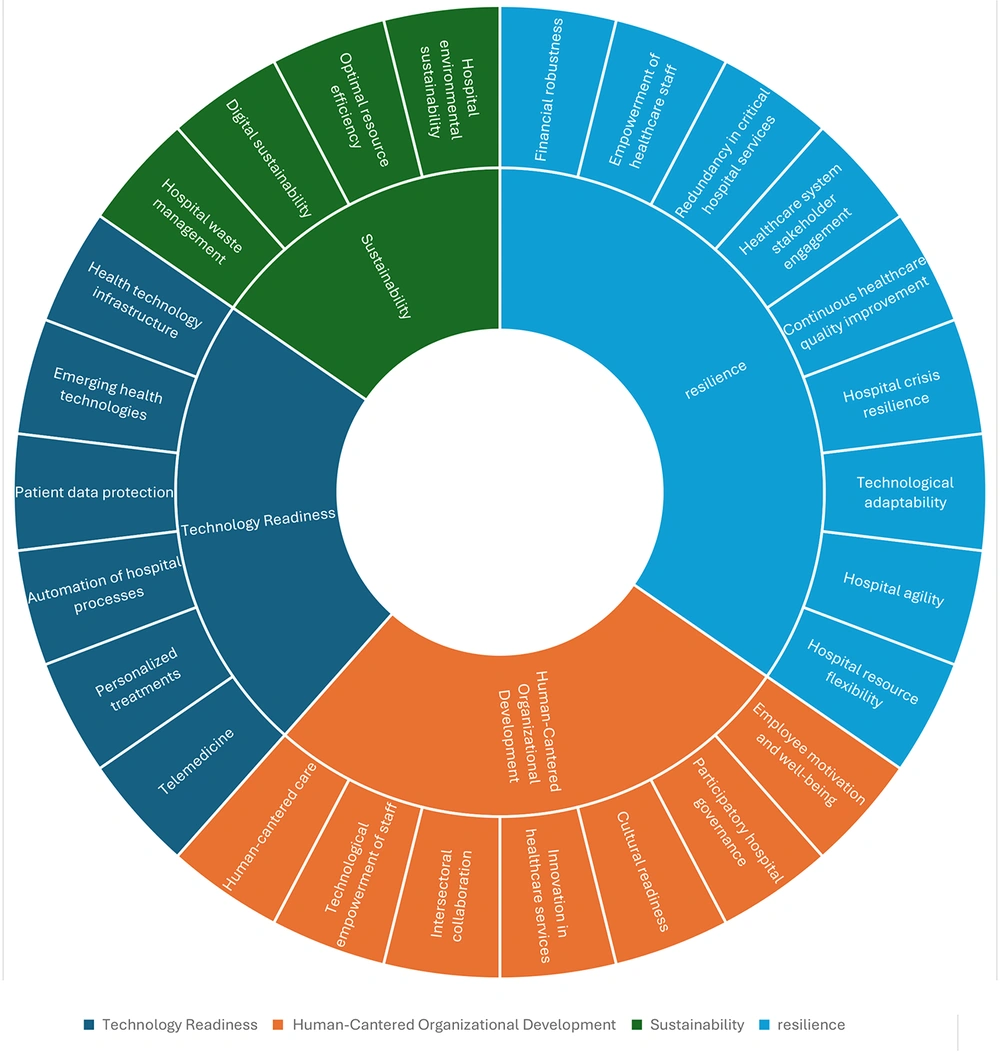
The final model was structured around four key pillars of Industry 5.0: Technological readiness, sustainability, resilience, and human-centered organizational development (17). Accordingly, all indicators identified in the systematic review — whether based on the base model or those added to complete and redefine the model — were assigned to one of these four groups to reflect their characteristics. Table 2 presents the final indicators of the Hospital 5.0 readiness assessment model, and Figure 2 illustrates the overall model framework. Each indicator in the "Reference Models" column shows which of the 21 readiness and maturity models it was derived from. We added indicators that are not linked to any specific model. These indicators are based on the literature in Healthcare 5.0 and Industry 5.0 and align with the research objectives and the specific needs of Hospital 5.0.
| Main and Sub-dimensions | Description | Reference Models | Sources |
|---|---|---|---|
| Technology readiness | |||
| Health technology infrastructure | Systems and technologies required to support digital and intelligent hospital processes. | IMPULS/Industry 4.0 maturity model for SMEs | (9, 38) |
| Emerging health technologies | New technologies, such as IoT, AI, and Big Data, that improve the efficiency and quality of health services. | IMPULS/Industry 4.0 maturity model/AI innovation maturity model | (8, 9, 35) |
| Patient data protection | Rules and procedures for protecting patient and sensitive data | IMPULS/AI innovation maturity model | (8, 9) |
| Automation of hospital processes | Using technology to automate and optimize hospital management processes, improving efficiency and reducing errors. | IMPULS/Industry 4.0 maturity model/AI innovation maturity model/Industry 4.0 readiness model for tool management | (8, 9, 29, 35) |
| Personalized treatments | Treatment approaches that are designed based on the unique characteristics of each patient. | - | (5, 41) |
| Telemedicine | Providing medical services and consultations via technology, allowing remote patient access. | IMPULS | (8, 9, 42) |
| Human-centered organizational development | |||
| Human-centered care | Designing and implementing systems that meet human needs to improve patient and staff experience. | - | (43) |
| Technological empowerment of staff | Training programs that help hospital staff understand and effectively use new technologies. | IMPULS/Industry 4.0 maturity model for SMEs | (9, 38) |
| Intersectoral collaboration | The interaction and collaboration between hospital departments to improve service quality and reduce response times. | The connected enterprise maturity model/Industry 4.0 maturity model for SMEs/Industry 4.0 readiness analysis | (27, 30, 38) |
| Innovation in healthcare services | The hospital’s ability to develop and implement innovative ideas to improve services and processes. | IMPULS/Industry 4.0 maturity model | (8, 9) |
| Cultural readiness | The willingness of hospital staff to embrace new technologies and processes with a positive attitude. | IMPULS/Industry 4.0 maturity model | (8, 9, 44) |
| Participatory hospital governance | Creating an environment that involves staff and patients in decision-making and hospital policies. | - | (45-47) |
| Employee motivation and well-being | Systems of incentives and recognition that enhance staff motivation and job satisfaction. | Comprehensive Industry 4.0 readiness model | (37) |
| Sustainability | |||
| Hospital environmental sustainability | Strategies aimed at conserving resources and promoting environmental sustainability in hospital operations. | - | (17, 48-50) |
| Optimal resource efficiency | Efficient management and allocation of human, financial, and physical resources in hospitals | - | (5, 48) |
| Digital sustainability | The use of digital solutions and new technologies to reduce environmental impact and improve resource efficiency. | - | (51-54) |
| Hospital waste management | Measures to minimize waste of resources and time in medical and administrative processes. | - | (5, 41, 42, 55) |
| Resilience | |||
| Hospital resource flexibility | Employees with multiple skills who can work across different hospital departments. | IMPULS | (9, 42) |
| Hospital agility | The hospital’s ability to quickly adapt to changes in environment, technology, or patient needs through flexible structures and rapid decision-making. | - | (56-58) |
| Technological adaptability | The hospital’s ability to adopt and use new technologies within existing systems. | IMPULS | (9, 59) |
| Hospital crisis resilience | The hospital’s ability to prepare for and handle crises and emergencies. | - | (60-62) |
| Continuous healthcare quality improvement | Ongoing efforts to enhance processes and service quality through regular evaluation and incremental innovation. | - | (5, 41, 63) |
| Healthcare system stakeholder engagement | Working together with all stakeholders — patients, staff, and the community — to enhance service quality. | - | (64-66) |
| Redundancy in critical hospital services | Presence of systems and processes that ensure services continue during malfunctions or issues. | - | (14, 67, 68) |
| Empowerment of healthcare staff | Creating opportunities for staff to develop skills and knowledge, improving individual and team performance. | - | (69, 70) |
| Financial robustness | Hospitals’ ability to manage finances and deliver sustainable health services. | - | (71, 72) |
To validate the proposed model, a panel of five experts in healthcare management and digital transformation reviewed the Hospital 5.0 readiness model. They provided structured feedback in two rounds, assessing the clarity, relevance, and practical applicability of each dimension and sub-dimension. Modifications were made based on consensus, ensuring alignment with both theoretical foundations and real-world hospital practices.
4.3. Validity of the Model
To ensure the relevance of the proposed indicators for Hospital 5.0, all items were carefully adapted to the healthcare context, with terminology and descriptions reflecting hospital processes and human-centered care. A panel of 12 healthcare experts then evaluated each indicator for its necessity. The agreement measure, known as the content validity ratio (CVR) (73), ranged from 0.67 to 1.00 across all indicators, confirming that they were considered essential or highly relevant. These results, summarized in Table 3, demonstrate that the framework is appropriate for hospital settings and captures the unique characteristics of Hospital 5.0 rather than merely adopting Industry 4.0 indicators.
| Indicators | No. of Experts Rating “Essential” | CVR | Result |
|---|---|---|---|
| Health technology infrastructure | 12 | 1.00 | Accepted |
| Emerging health technologies | 11 | 0.83 | Accepted |
| Patient data protection | 12 | 1.00 | Accepted |
| Automation of hospital processes | 10 | 0.67 | Accepted |
| Personalized treatments | 11 | 0.83 | Accepted |
| Telemedicine | 12 | 1.00 | Accepted |
| Human-centered care | 10 | 0.67 | Accepted |
| Technological empowerment of staff | 11 | 0.83 | Accepted |
| Intersectoral collaboration | 12 | 1.00 | Accepted |
| Innovation in healthcare services | 11 | 0.83 | Accepted |
| Cultural readiness | 10 | 0.67 | Accepted |
| Participatory hospital governance | 12 | 1.00 | Accepted |
| Employee motivation and well-being | 11 | 0.83 | Accepted |
| Hospital environmental sustainability | 12 | 1.00 | Accepted |
| Optimal resource efficiency | 10 | 0.67 | Accepted |
| Digital sustainability | 12 | 1.00 | Accepted |
| Hospital waste management | 10 | 0.67 | Accepted |
| Hospital resource flexibility | 12 | 1.00 | Accepted |
| Hospital agility | 11 | 0.83 | Accepted |
| Technological adaptability | 10 | 0.67 | Accepted |
| Hospital crisis resilience | 12 | 1.00 | Accepted |
| Continuous healthcare quality improvement | 11 | 0.83 | Accepted |
| Healthcare system stakeholder engagement | 10 | 0.67 | Accepted |
| Redundancy in critical hospital services | 12 | 1.00 | Accepted |
| Empowerment of healthcare staff | 11 | 0.83 | Accepted |
| Financial robustness | 10 | 0.67 | Accepted |
Abbreviation: CVR, content validity ratio.
4.4. Prioritization and Weighting of Model Dimensions and Sub-dimensions
This study uses a questionnaire based on the GBWM, as detailed in Appendix 2 in Supplementary File, to weight the indicators. The best-worst method is designed to be effective with a limited number of experts (usually between 5 and 10), making it a logical and cost-effective choice for studies with constrained resources (74).
To ensure a comprehensive evaluation of the Hospital 5.0 indicators using the GBWM, a panel of five experts with diverse and complementary professional backgrounds was carefully selected. The panel included:
- A hospital manager aged 40 - 49 with over 15 years of experience in hospital administration.
- An IT director aged 40 - 49 with more than 15 years of experience in healthcare information systems.
- A department supervisor aged 50+ with over 15 years of clinical management experience.
- A faculty member from Shiraz University in the Health Management Department, aged 40 - 49 with more than 15 years of academic and managerial experience.
- A hospital manager aged 40 - 49 with 10 - 15 years of experience in hospital administration.
Including experts from clinical, managerial, academic, and technological domains ensured that the assessment captured not only technological perspectives but also human-centered and operational aspects of hospital management. This careful selection mitigated any bias toward purely IT-focused views and provided a robust, multi-dimensional validation of the proposed Hospital 5.0 framework. The final weights of the dimensions are presented in Tables 4 and 5. The obtained weights represent the global weights (the global weight of each sub-dimension is calculated by multiplying the weight of the main dimension by the weight of the sub-dimension within that dimension) of the sub-dimensions, which are relatively small.
| Main Dimensions | Final Weights |
|---|---|
| Technology readiness | 0.49 |
| Human-centered organizational development | 0.23 |
| Sustainability | 0.13 |
| Resilience | 0.16 |
| Sub-dimensions | Final Weights |
|---|---|
| Health technology infrastructure | 0.160 |
| Emerging health technologies | 0.090 |
| Patient data protection | 0.060 |
| Automation of hospital processes | 0.100 |
| Personalized treatments | 0.040 |
| Telemedicine | 0.040 |
| Human-centered care | 0.059 |
| Technological empowerment of staff | 0.032 |
| Intersectoral collaboration | 0.023 |
| Innovation in healthcare services | 0.040 |
| Cultural readiness | 0.051 |
| Participatory hospital governance | 0.004 |
| Employee motivation and well-being | 0.019 |
| Hospital environmental sustainability | 0.026 |
| Optimal resource efficiency | 0.030 |
| Digital sustainability | 0.052 |
| Hospital waste management | 0.022 |
| Hospital resource flexibility | 0.019 |
| Hospital agility | 0.020 |
| Technological adaptability | 0.024 |
| Hospital crisis resilience | 0.016 |
| Continuous healthcare quality improvement | 0.028 |
| Healthcare system stakeholder engagement | 0.011 |
| Redundancy in critical hospital services | 0.018 |
| Empowerment of healthcare staff | 0.011 |
| Financial robustness | 0.013 |
5. Discussion
5.1. Results and Findings
Analysis of the dimension weighting based on expert opinions shows that “Technological Readiness” is the most important dimension in assessing Hospital 5.0 readiness, accounting for 50% of the total weight. Within this dimension, the highest importance is assigned to technological infrastructure (16%) and automation of hospital processes (10%), while sub-indicators such as telemedicine (4%) and personalized treatments (4%) receive lower weights. This distribution indicates that experts primarily focus on strengthening technical infrastructure and leveraging new technologies, whereas emerging areas like telemedicine and personalized treatments currently have a lesser emphasis.
One of the key and frequently mentioned strategies in the reviewed studies for enhancing this dimension is the optimization and maximum utilization of existing infrastructures and equipment. By improving the quality of software systems and management platforms, as well as enhancing communication networks, hospitals can increase their capacity to adopt emerging technologies and the internet of things without incurring excessive costs. This approach not only reduces the workload of healthcare staff but also improves the ability to provide specialized services to patients with specific needs (75, 76).
In second place, "Human-Centered Organizational Development" holds a 23% share. Within this dimension, the highest emphasis is on human-centered care (6%), intersectoral collaboration (2%), and innovation (4%). In contrast, indicators such as employee incentive and recognition systems (2%) and participatory hospital governance (1%) are considered less important. This indicates that experts prioritize strategic alignment and fostering a culture of collaboration and innovation, while softer cultural indicators, like organizational democracy, receive less attention.
Studies have shown that developing strategies to maintain and enhance the physical and mental well-being of employees, as well as preparing them to embrace change, are key factors in strengthening the human-centered organizational development dimension (77).
Resilience (0.016) ranks third among the main dimensions. Within this dimension, "Technological Adaptability" (0.024) is identified as the most critical sub-dimension, while "stakeholder engagement" (0.011) is the least critical. Overall, this distribution highlights that experts emphasize the hospital’s ability to adapt technologically, whereas participatory processes are considered less critical in the current assessment. According to previous studies, the response time of hospitals to changes — such as the implementation of new technologies in clinical and managerial processes and the execution of crisis management programs — plays a crucial role in enhancing organizational resilience (60, 78).
Sustainability ranks third with a (13%) share. Within this dimension, resource efficiency (3%) and digital sustainability (0.05%) are identified as the top priorities, while waste reduction (0.02%) and hospital environmental sustainability (0.02%) have lower shares. This distribution indicates that experts focus more on optimizing resource use and managing sustainable technologies rather than on high-level policymaking or waste reduction. This distribution indicates that experts emphasize optimizing resource use and managing sustainable technologies.
According to the studies, the optimal use of human, financial, and physical resources to reduce energy consumption, along with the adoption of advanced technologies to minimize negative environmental impacts, are two key strategies for enhancing the sustainability of Smart Hospital 5.0 (79, 80). The first strategy is less costly than the second one. Therefore, optimizing resource efficiency is considered an effective and practical approach, particularly suitable for Iranian hospitals facing financial constraints.
5.2. Managerial Implications
In this section, key indicators are introduced to operationalize the main dimensions of the Hospital 5.0 framework, providing measurable metrics to assess, monitor, and improve hospital performance. These indicators provide practical measures to guide hospital assessment and improvement. Table 6 presents selected, representative indicators for each of the four main dimensions.
| Main Dimension | Indicators | Operational Definition/Brief Analysis | Source |
|---|---|---|---|
| Technological readiness | Network capability for leveraging emerging technologies; Quality of technological infrastructure in reducing staff workload; Adoption and utilization of emerging technologies; Degree of administrative task automation | These indicators assess the hospital’s technological preparedness, including the effectiveness of communication networks for emerging technologies, IT infrastructure supporting staff efficiency, adoption of innovations like IoT and AI, and automation of routine administrative tasks. Collectively, they link digital readiness with operational and human-centered outcomes. | (5, 75, 76, 81-83) |
| Human-centered organizational development | Strategies for enhancing the wellbeing of staff, patients, and the community; Access to advanced technology training; Mechanisms supporting innovation; Readiness for organizational change | These indicators evaluate the hospital’s focus on human-centered management, including staff well-being initiatives, training in emerging technologies, mechanisms to promote and support innovation, and overall readiness of employees to accept organizational changes. Collectively, they capture not only the technological and operational aspects but also the wellbeing and engagement of staff, patients, and the broader community. | (77, 84-87) |
| Sustainability | Degree of application of emerging technologies to decrease environmental impacts; Implementation of circular waste management practices; Degree of setting environmental sustainability goals | These indicators collectively evaluate the hospital’s readiness for digital and operational sustainability, its commitment to minimizing environmental impact and waste through circular management practices, and its organizational focus on achieving defined sustainability goals. | (81, 88-90) |
| Resilience | Effectiveness and efficiency of crisis response programs; The degree of redundancy in health system; The degree of hospital financial reserve | These indicators collectively capture the hospital’s resilience, reflecting its ability to respond effectively and efficiently to unexpected events, maintain backup systems, and preserve financial resources to ensure continuity. | (60, 91, 92) |
5.3. Theoretical Implications
Although the proposed Hospital 5.0 indicators are designed to be conceptually universal, their practical application requires contextual interpretation. Previous studies emphasize that core dimensions such as technological readiness, human-centered development, sustainability, and resilience maintain cross-context validity across healthcare systems. For example, Baihaqy and Subriadi (93) highlight the universal relevance of digital transformation indicators in hospitals; Kovesdi et al. (94) demonstrate that human-technology integration metrics apply across diverse health systems; Dolcini et al. (95) and Verma et al. (96) identify environmental sustainability and resilience as globally shared priorities for next-generation hospitals.
However, when the indicators are used for assessment, prioritization, and policy decision-making, contextual adaptation becomes necessary. Local infrastructure maturity, financial capacity, regulatory frameworks, and workforce characteristics can significantly influence how the same indicator manifests in different hospital environments.
For instance, in the context of Iran, even if the technological readiness dimension is universally defined, its operationalization must reflect local constraints. If the assessment reveals a low level of technological readiness — especially due to limited digital infrastructure or financial constraints — hospitals may prioritize low-cost, high-impact interventions such as:
- Transitioning from paper-based documentation to basic electronic health record modules instead of full-scale AI-based systems
- Adopting open-source or locally developed digital tools instead of expensive commercial platforms
- Investing in targeted staff training programs rather than large-scale hardware upgrades.
This example illustrates how universal indicators guide the conceptual framework, while local conditions shape implementation pathways. Therefore, the framework maintains theoretical universality, yet the managerial implications require contextual customization to ensure feasibility and effectiveness in different healthcare systems.
5.4. Conclusions
In this study, a Hospital 5.0 readiness assessment model was first developed using a systematic review and the best-fit framework. The model indicators were then prioritized. The results showed that technological readiness and human-centered organizational development received the highest weights, followed by resilience and sustainability. This pattern aligns with the experience of developed countries, where technological infrastructure and capable human resources are established first, followed by the implementation of resilience and crisis preparedness programs.
From this perspective, the transition to Hospital 5.0 is viewed by experts as a technology-driven process, strengthened by human resource empowerment, while sustainability and resilience play complementary and supportive roles. The findings of this study can serve as a practical guide for hospitals to prioritize investments in technology and human resource development. They can also support planning efforts to enhance organizational resilience and sustainability. At the national level, the results provide an evidence-based framework for the Ministry of Health to develop policies and strategies for the transition toward smart hospitals.
The study’s limitations include the use of literature primarily in English and a limited number of experts. Although only five experts participated, this is reasonable given the novelty of the Hospital 5.0 concept. However, involving more experts could improve the generalizability of the results. The proposed model was specifically designed for hospitals but could be adapted for smaller healthcare centers. Future research could apply case studies across multiple hospitals to evaluate and prioritize readiness levels for the transition to Hospital 5.0.