1. Background
Delirium is the most common neurological diagnosis among patients admitted to the intensive care unit (ICU). It is a severe brain disorder, associated with reduced attention and cognition. The onset of this disorder is acute, as it can manifest within hours to days. It is characterized by fluctuations in the level of consciousness or impaired consciousness, along with a decrease in environmental awareness (1). The incidence of delirium in ICUs is about 8% - 92%, which depends on the severity of the disease, the number of patients treated with mechanical ventilation, and different populations of patients (e.g., internal surgery) (2).
Generally, delirium remains unknown or misdiagnosed in 84% - 66% of cases because it has symptoms similar to depression and dementia (1). Complications of delirium persist in at least 20% of patients aged 65 years or above, thereby increasing the hospital costs. These complications are associated with the increased length of hospital and ICU stay, increased mortality, delayed separation from mechanical ventilation, nosocomial pneumonia, increased risk of delirium recurrence, risk of fall, urinary incontinence, permanent skin disorder, and lack of improvement in the cognitive status (2-5).
Haloperidol exerts its therapeutic effects mainly by blocking dopamine receptors. Alpha-adrenergic and muscarinic receptors are also partially blocked by haloperidol. Indications for haloperidol use include psychotic disorders, hallucinations, neurological tics, delirium, and behavioral problems in children. The extrapyramidal symptoms are among the most important side effects of haloperidol. Extrapyramidal complications, especially akathisia and dystonic reactions, are also more common among haloperidol users. Although haloperidol is commonly used to treat delirium in the ICU setting, the presence of extrapyramidal complications has limited its use in many patients (5, 6). Other side effects of haloperidol include drowsiness, nightmares, mood instability, euphoria, and insomnia. People with long-term use may also develop dyskinesia (7).
Other side effects of haloperidol include dry mouth, constipation, blurred vision, fatigue and weakness, nasal congestion, and urinary retention, which occurs occasionally. Also, use of this agent changes the number of white blood cells and increases the liver function parameters. In the cardiovascular system, it also causes changes in the electrocardiogram (EKG) and results in hypotension, tachycardia, and hypertension (6). Some studies suggest that the use of dexmedetomidine, a selective α-2 antagonist, reduces the incidence of cognitive impairment and delirium in mechanically ventilated patients (8).
There are two theories about the effect of dexmedetomidine on reducing delirium. Some researchers believe that gamma-aminobutyric acid (GABA), as the main neurotransmitter and inhibitor in the central nervous system, is one of the predisposing factors for delirium. Dexmedetomidine can be effective in the prevention and control of delirium by controlling and acting on GABA receptors. On the other hand, the possibility of an association between sleep disorders and delirium, especially in patients admitted to the ICU, is another hypothesis. Dexmedetomidine can be effective in reducing delirium by creating a sedative and normal state of normal sleep in individuals (9-12). According to the second theory, the cholinergic nervous system is related to various aspects of the cognitive system, including memory, attention, concentration, and learning. According to this theory, anticholinergic drugs can increase the risk of delirium. Dexmedetomidine reduces the risk of delirium due to its sedative effects, besides reducing the need for anticholinergic drugs, such as benzodiazepines and narcotics (9-19).
Considering the importance of delirium in patients and the scarcity of research in this field, we aimed to compare the effects of haloperidol and dexmedetomidine on delirium and agitation in mechanically ventilated patients following concussion admitted to the ICU. Also, the level of consciousness, the number of days hospitalized in the ICU, and the number of days intubated were studied.
2. Objectives
Patients under mechanical ventilation in the ICU have a higher risk of delirium. To date, the ideal sedative combination in terms of cost and side effects for delirium treatment has not been identified. This study was designed to compare the effects of haloperidol and dexmedetomidine on delirium in trauma patients under mechanical ventilation in the ICU.
3. Methods
After obtaining permission from the Ethics Committee of Ahvaz University of Medical Sciences, Ahvaz, Iran (code: IR.AJUMS.REC.1399.155) and registering the study in the Iranian Registry of Clinical Trials (code: IRCT20200803048288N1), sixty patients with a moderate traumatic brain injury (GCS = 9-12), admitted to the ICU of Golestan Hospital in Ahvaz, Iran, were enrolled. Due to intubation and lack of awareness in all patients, after explaining the objectives of the study and ensuring the confidentiality of information, the patient's guardian was informed (due to intubation of the patient).
The patients were randomly divided into one of the two groups based on even and odd numbers. The inclusion criteria were as follows: age of 18 - 65 years; mechanical ventilation; the Acute Physiologic and Chronic Health evaluation II (APACHE II) score > 48; Richmond Agitation Sedation scale (RASS) score of -5 to +4; and elapsed time of at least 48 hours after ICU admission. On the other hand, the exclusion criteria were as follows: dissatisfaction; allergy to haloperidol; history of moderate to severe dementia; Parkinson's disease; brain injury; chronic use of antipsychotic drugs; long QT intervals (> 500 ms); history of a malignant neuroleptic syndrome; family history of dystonic drug reactions; Torsades de pointes syndrome; pregnancy; admission to ICU for less than 48 hours; extrapyramidal symptoms after haloperidol administration; and patient’s death (chance of survival less than 48 hours).
All patients received routine care. Also, 48 hours after admission to the ICU, patients in the haloperidol group received 2.5 mg of haloperidol intravenously every eight hours for ten minutes daily, and the dexmedetomidine group received 0.5 µg/kg of dexmedetomidine via intravenous infusion every other day. Delirium and agitation were measured and recorded based on the RASS criteria. Also, the length of hospital stay, duration of mechanical ventilation, and need for sedation up to seven days after the intervention were recorded in both groups. If sedation was required, the patient received 1 mg of midazolam and 50 µg of fentanyl intravenously. For blinding, the patients and the individual completing the questionnaire were unaware of the type of injectable drug. The GCS scale was used to assess the patients’ level of consciousness, and the RASS and APACHE II scales were used to determine the level of agitation. The Confusion Assessment method-ICU (CAM-ICU) criteria were used to determine the incidence of delirium.
For comparison of the results, SPSS version 22 was used. For a more accurate interpretation of the results, the two groups were matched by the frequency matching method. Then, qualitative and frequency variables were compared using chi-square test. Independent two-samples t-test, Mann-Whitney test, or chi-square test was also used to compare the quantitative variables based on the normal distribution of data.
4. Results
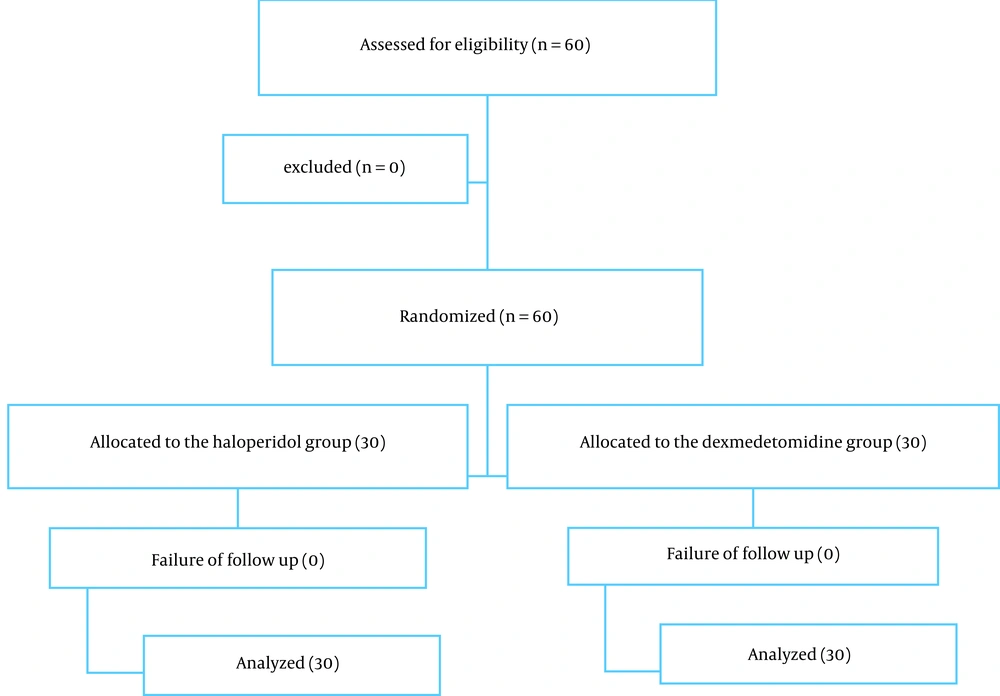
This study was a double-blind, randomized clinical trial, comparing the effects of haloperidol and dexmedetomidine on delirium and agitation in intubated patients with a traumatic brain injury in the ICU of Golestan Hospital in Ahvaz, Iran. Sixty patients, aged 18 - 65 years, were divided into two groups of 30 patients, receiving either haloperidol (H) or dexmedetomidine (D). The demographic information of the patients in both groups is shown in Table 1. Based on the results, there was no significant difference regarding the demographic information of the patients between the two groups (P < 0.05). Figure 1 shows the research procedure and the clinical examination results of the patients.
| Variables | Mean ± SD | P-Value |
|---|---|---|
| Age, y | 0.4 | |
| Haloperidol | 36.8 ± 10.1 | |
| Dexmedetomidine | 40.1 ± 15.2 | |
| Gender, % | 0.7 | |
| Haloperidol | ||
| Male | 53.3 | |
| Female | 15 | |
| Dexmedetomidine | ||
| Male | 23.3 | |
| Female | 8.4 | |
| Number of days in the ICU | 0.4 | |
| Haloperidol | 11.8 ± 3.0 | |
| Dexmedetomidine | 12.2 ± 5.2 | |
| Number of intubation days | 0.1 | |
| Haloperidol | 7.0 ± 3.7 | |
| Dexmedetomidine | 6.3 ± 2.5 |
Based on the results presented in Table 1, there was no significant difference between the two groups in terms of the number of required days for ventilation (P = 0.17) and the number of days in ICU (P = 0.49). Changes in the level of consciousness based on the GCS in the two groups are shown in Table 2. According to this table, there was no significant difference in the level of consciousness of patients between the two groups in any of the studied intervals (1 - 7 days after the intervention) (Table 2). However, there were significant differences between the two groups in terms of the agitation score (RASS) (Table 3) and APACHE II score three to seven days after the intervention (P < 0.05). Patients in the dexmedetomidine group with lower agitation scores were calmer and had a more stable condition (Table 4).
| Time | Dexmedetomidine | Haloperidol | P-Value |
|---|---|---|---|
| First day | 8.9 ± 1.8 | 9.0 ± 1.3 | 0.1 |
| Second day | 8.9 ± 1.8 | 9.4 ± 1.4 | 0. 1 |
| Third day | 9.0 ± 1.7 | 9.8 ± 1.4 | 0.3 |
| Fourth day | 9.1 ± 2.3 | 10.2 ± 1.6 | 0.2 |
| Fifth day | 9.6 ± 1.8 | 10.4 ± 1.7 | 0.4 |
| Sixth day | 9.9 ± 1.7 | 10.7 ± 1.6 | 0.4 |
| Seventh day | 10.0 ± 1.7 | 10.8 ± 1.7 | 0.7 |
| Time | Haloperidol | Dexmedetomidine | P-Value |
|---|---|---|---|
| First day | 0.9 ± 2.8 | 0.8 ± 2.5 | 0.1 |
| Second day | 0.9 ± 2.7 | 0.7 ± 2.2 | 0.04 |
| Third day | 0.8 ± 1.9 | 0.7 ± 2.5 | 0.0 |
| Fourth day | -0.9 ± 0.7 | 0.2 ± 0.2 | 0.0 |
| Fifth day | -0.9 ± 0.4 | -0.8 ± 0.9 | 0.0 |
| Sixth day | -1.0 ± 1.4 | -1.0 ± 0.8 | 0.0 |
| Seventh day | -1.4 ± 1.7 | 1.0 ± 0.1 | 0.0 |
| Time | Haloperidol | Dexmedetomidine | P-Value |
|---|---|---|---|
| First day | 23.5 ± 10.1 | 21.6 ± 7.8 | 0.5 |
| Second day | 28.8 ± 5.2 | 28.3 ± 4.2 | 0.3 |
| Third day | 31.5 ± 2.5 | 25.3 ± 3.8 | 0.0 |
| Fourth day | 28.4 ± 0.8 | 21.5 ± 16.0 | 0.0 |
| Fifth day | 24.1 ± 4.6 | 20.4 ± 5.4 | 0.0 |
| Sixth day | 29.5 ± 5.3 | 26.6 ± 4.9 | 0.0 |
| Seventh day | 26.8 ± 5.0 | 23.2 ± 4.4 | 0.0 |
Moreover, the incidence of delirium was assessed according to the CAM-ICU criteria. The results showed a significant difference between the two groups in terms of the incidence of delirium at 5 - 7 days after the intervention (P < 0.05). The incidence of delirium was lower in the dexmedetomidine group compared to the haloperidol group (Table 5).
| Time | Haloperidol | Dexmedetomidine | P-Value |
|---|---|---|---|
| First day | 6 (20) | 5 (16.6) | 0.5 |
| Second day | 6 (20) | 5 (16.6) | 0.7 |
| Third day | 7 (23.3) | 5 (16.6) | 0.2 |
| Fourth day | 8 (26.6) | 6 (20) | 0.1 |
| Fifth day | 10 (33.3) | 6 (20) | 0.0 |
| Sixth day | 10 (33.3) | 6 (20) | 0.0 |
| Seventh day | 12 (40) | 6 (20) | 0.0 |
5. Discussion
This double-blind, randomized clinical trial was performed to compare the effects of haloperidol and dexmedetomidine on agitation in 60 mechanically ventilated patients admitted to the ICU following concussion. Sixty patients with a moderate traumatic brain injury were randomly divided into two groups. Patients in the haloperidol group received 2.5 mg of haloperidol intravenously every eight hours for ten minutes daily, and the dexmedetomidine group received 0.5 µg/kg of dexmedetomidine via intravenous infusion every other day. Delirium, agitation, length of hospitalization, duration of mechanical ventilation, and need for sedation up to seven days were measured and recorded in both groups.
The results of this study showed that there was a significant difference between patients receiving haloperidol and dexmedetomidine regarding the incidence of delirium according to the CAM-ICU and APACHE II scores and regarding agitation according to the RASS criteria. However, there was no significant difference between the two groups in terms of the level of consciousness, the number of days hospitalized in the ICU, and the number of intubation days. In this regard, Carrasco et al. (8), in a study conducted in 2016 in Spain, evaluated the clinical efficacy and safety of dexmedetomidine for the treatment of delirium and agitation in ICUs and compared it with haloperidol. They showed that the long-acting dexmedetomidine group had shorter ICU and hospital stays than the haloperidol group. Also, the agitation score of the dexmedetomidine group was lower than the haloperidol group. They concluded that dexmedetomidine could be used as a low-risk and effective drug for the treatment of delirium in patients admitted to the ICU; their results are consistent with the present study (8).
In line with the present study, a clinical trial by Pasin et al. (20) from Italy (2014) on the role of dexmedetomidine in the prevention and treatment of delirium in ICU patients showed that dexmedetomidine significantly reduced delirium, agitation, and confusion. Mechanically ventilated patients admitted to the ICU were compared with a control group, and it was found that dexmedetomidine was effective in reducing the incidence of delirium in patients admitted to the ICU (20). Consistent with the present study, Bakri et al. (21), in a three-day clinical trial from Egypt concluded that dexmedetomidine, compared to haloperidol, could be used effectively to control post-traumatic delirium in patients admitted to the ICU.
In 2018, Flukiger et al. (22) conducted a review study (28 clinical trials including 5141 patients admitted to the ICU) to evaluate the effect of dexmedetomidine on the prevention and treatment of delirium in patients admitted to the ICU. Similar to the present study, the incidence of delirium and the need for drugs to control pain and agitation in the group receiving dexmedetomidine were significantly lower than the control group or the group receiving haloperidol. On the other hand, patients in the group receiving dexmedetomidine were significantly exposed to bradycardia and hypotension. They concluded that dexmedetomidine reduced the incidence of delirium in patients admitted to the ICU. However, more extensive studies are needed to compare the effects of this drug with haloperidol (22).
In line with the present study, Reade et al. in 2009 showed that the incidence of delirium, agitation, length of ICU stay, and need for ventilation for seven days in the dexmedetomidine group were significantly less than the haloperidol group (P = 0.05). They concluded that dexmedetomidine was very effective in treating delirium and agitation in patients admitted to the ICU (11). In this regard, Rood et al. (23) found that administration of haloperidol had no effects on the incidence of delirium in patients admitted to the ICU and that there was no significant difference between patients receiving haloperidol and placebo.
Another study by Nelson et al. (24) in 2015 revealed that dexmedetomidine, by providing sedation and reducing the need for it, indirectly reduced delirium in patients admitted to the ICU. Moreover, in 2018, Louis et al. (25) concluded that administration of dexmedetomidine to patients admitted to the ICU could reduce the incidence of delirium, which is consistent with the results of the present study. In a similar study, Abdelgalel (26) compared the incidence of delirium using haloperidol and dexmedetomidine. In this clinical trial, 90 patients were studied under mechanical ventilation. The incidence of delirium, length of hospitalization, and number of days required for mechanical ventilation in patients receiving dexmedetomidine were lower than patients receiving haloperidol. They found that dexmedetomidine was more effective and efficient than haloperidol in preventing and controlling delirium in hospitalized patients; these results are in line with the present study.
In another clinical trial in 2014, Kalisvaart et al. (27) examined the effect of haloperidol on the incidence of delirium after a major surgery in the elderly. It was concluded that haloperidol administration could reduce delirium in patients (27). This difference can be attributed to differences in the sample size or the type of measuring instrument. However, Fukuta et al. (28) reported that there was no significant difference in the incidence of delirium between patients receiving haloperidol and the control group after a major surgery.
5.1. Conclusions
The results of this study showed that there was a significant difference between patients receiving haloperidol and dexmedetomidine in terms of delirium incidence and agitation; patients in the dexmedetomidine group were calmer and experienced less delirium. However, there was no significant difference between the two groups regarding the level of consciousness, the number of days hospitalized in the ICU, or the number of intubation days. According to the results, dexmedetomidine is a less risky and more effective drug for the prevention and treatment of delirium and agitation in patients admitted to the ICU and can provide more stable and appropriate conditions for patients.