1. Background
One of the most common complicated events that affect the outcome of urethral repair surgeries is the occurrence of erection during and after surgery, which leads to surgical complications such as fistula, wound dehiscence, surgical failure, and probable reoperation that would be a very important challenge for patients and their surgeons. The overall prevalence of erection during penile surgery under anesthesia is reported to be 0.1 to 2.4% in general anesthesia, 0.34 - 3.5% in spinal anesthesia, 0.11 - 0.3, and 1.72 - 3.8% in epidural anesthesia (1). Partial or complete erection during general anesthesia in urologic surgery is a relatively rare but challenging condition with an incidence of 0.1 to 2.4%. While the cause is unknown, it is generally possible that stimulating the penis while preparing the skin or the tool used for the procedure may be the main cause of the erection (2).
Boys before puberty and adult men have erections three to eight times during the night, which is associated with REM sleep periods. Erection is activated by the parasympathetic system (3). The parasympathetic system is stimulated by the sensory, auditory, visual, and olfactory pathways and through mechanical and reflexogenic stimulation of the genital organs (4, 5). Urinary tract repair surgeries are common and the occurrence of this problem during and after the operation may lead to procedure failure and the need for reoperation and result in more risks and costs to the patient. Achieving the right solution to prevent this problem can have a significant impact on the treatment process and also reduce health care costs.
Many methods have been used to solve this problem. In a report, caudal block (bupivacaine plus epinephrine) and penile block (ropivacaine plus clonidine) were successful to prevent erection (6). Other methods such as dorsal penis block, prescribing phenylephrine, metaraminol, glycopyrrolate, nitroglycerin and sodium nitroprusside, diphenhydramine, amyl nitrite, steroid, oral terbutaline, diazepam, and midazolam have been used to prevent erection (7). Dexmedetomidine is a potent selective α2 agonist with sedative and analgesic effects that reduce the heart rate and blood pressure. Blood pressure reduction is achieved by acting on the sympathetic and reducing norepinephrine secretion by stimulating peripheral α2 presynaptic receptors. In addition, α2 agonist agents, by acting on vascular smooth muscle, can cause vasoconstriction of peripheral arteries and prevent erections (8-11).
Studies showed that aminoamide local anesthetics administration at low doses results in vasoconstriction, and high doses cause vasodilatation. Ropivacaine has vasoconstrictive effects and can be used for epidural infusion to control pain and prevent erection (12, 13). The vasoconstrictive effects of intrathecal and epidural ropivacaine and the effects of dexmedetomidine on vascular smooth muscle can cause vasoconstriction in peripheral arteries. Thus, this hypothesis that erection can be prevented by injecting these two medications in the epidural space came to our mind. In this study, we decided to put this hypothesis to assay.
2. Objectives
In this study, we aimed to compare the effect of dexmedetomidine and ropivacaine epidural infusion on the incidence of erection after reconstructive urethral surgery.
3. Methods
3.1. Study Design
This randomized clinical trial was conducted on 45 patients who were scheduled for reconstructive urethral surgery at the referral urologic hospital of Shahid Beheshti University of Medical Sciences.
3.2. Patient Selection
The participants registered for the study were patients candidates for reconstructive urethral surgery and admitted to the urology ward at our hospital in the age group of 20 - 60 years. The inclusion criteria included patients candidates for urethral reconstructive surgery using oral mucosa aged 20 to 60 years. The non-entry criteria were contraindication of epidural catheterization, spinal deformities, history of using anti-androgen drugs before surgery, using β and α blocker drugs, neurological medications with positive or negative effects on the erection mechanism (SSRI, Antipsychotic, TCA) in the perioperative period, previous spine surgery, conductive cardiac disorder, using a pacemaker, arrhythmia, and erectile dysfunction before surgery. The exclusion criteria intra-operative bleeding leading to massive transfusion and accidental catheter displacement or removal.
Due to the absence of a similar study, in consultation with the statistical consultant and considering the importance of even one erection in each patient after these surgeries, and according to the calculations, 15 people were considered for each group. All patients gave their written informed consent before their inclusion in the study according to the University Hospital Ethics Committee (Ethics code IR.SBMU.RETECH.REC.1399.473; Iranian Clinical Trial Code IRCT20190131042569N4).
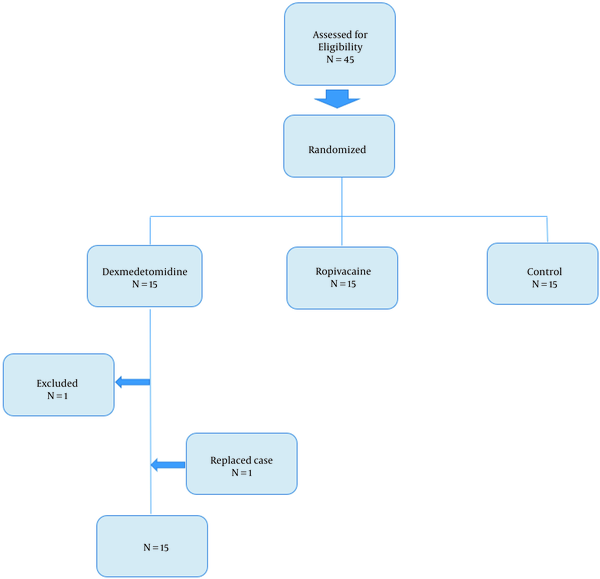
The patients were randomly divided into three groups using computer-generated simple randomization (random number generator software): (1) control group (n = 15), (2) dexmedetomidine group (n = 15), and (3) ropivacaine group (n = 15) (Figure 1). Thus, 15 patients received oral medication after surgery according to the conventional method (cyproterone compound tablets 50 mg BD and diazepam tablets 2 mg TDS for a week) to prevent erection, considered as the control group. The DEX group received dexmedetomidine, and the ROP group received ropivacaine via continuous epidural infusion in addition to the conventional method. The occurrence of erection during day and night was recorded separately until the seventh day after surgery. Due to the long-time interval between case selections, patients were not simultaneously admitted and were blind to their group. For DEX and ROP groups, we inserted an epidural catheter (by the same anesthesiologist for all patients) just before anesthesia induction in the operating room in the following circumstances: (1) sitting position, (2) aseptic technique, (3) bevel heads down, (4) catheter insertion level L5-S1 or L4-L5, and no drug infusion till the end of surgery.
3.3. Induction and Maintenance of Anesthesia
Anesthesia was induced after pre-oxygenation with 100% O2 Premedication: (1) midazolam 0.03 mg/kg, (2) fentanyl 5 µg/kg, and (3) 2% lidocaine 1 mg/kg. General anesthesia was induced by thiopental 3 - 5 mg/kg + atracurium 0.5 mg/kg. Nasal intubation for better surgical field access during buccal graft harvested from the inner lining of the mouth was done with proper nasal tracheal tubes. Anesthesia was maintained with 0.8 - 1.2% isoflurane plus 50 - 50% air-oxygen mixture (three litters each). The TOF stimulation of the ulnar nerve for neuromuscular blockade monitoring was applied. Then, BIS was kept between 40 and 60. Once the patient was fully awake at the end of the surgery, the tracheal tube was removed (TOF > 0.7 and BIS > 80).
After the end of the surgery, epidural infusion of dexmedetomidine or ropivacaine started and continued for one week. The epidural continuous pump contained dexmedetomidine 50 µg in a total of 100 cc sterile water volume (3 µg/h) for the dexmedetomidine group (dexmedetomidine HCL 100 µg/mL; Sedodex, IMAGEN Pharmaceutical, Iran) and 100 cc 0.125% ropivacaine in sterile water for the ropivacaine group (ropivacaine hydrochloride 5mg/mL; ropivacaina molteni, molteni pharmaceutical, Italy). The infusion rate was 6 cc/h (750 µg/h) and was the same for all patients throughout the study. All groups’ patients received oral medication after surgery according to the conventional method to prevent erection in the urology ward. They received 50 mg cyproterone compound tablets (cyproterone compound 50 mg; Aburaihan Pharmaceutical Co, Iran) twice a day and 2 mg diazepam tablets (diazepam 2 mg; Loghman Pharmaceutical Co., Iran) three times a day for a week to prevent erection. In the dexmedetomidine group, one patient's catheter was unintentionally removed, and he was excluded from the study and replaced with another patient (Figure 1). Due to the probable effects of dexmedetomidine and ropivacaine on hemodynamics (HR and BP), all patients were monitored for blood pressure and heart rate throughout the study period, and data were recorded (Table 1).
| Variables | Dexmedetomidine | Ropivacaine | Control |
|---|---|---|---|
| Age (y) | 38.2 ± 6.14 | 40.15 ± 7.10 | 37.85 ± 7.09 |
| Heart rate | 79.2 ± 8.45 | 71.65 ± 7.8 | 76.5 ± 9.1 |
| Systolic blood pressure (mmHg) | 118.5 ± 12.8 | 121.8 ± 11.06 | 116.9 ± 12.22 |
| Diastolic blood pressure (mmHg) | 70.9 ± 6.35 | 67.8 ± 5.49 | 69.05 ± 6.66 |
Demographic Features a
3.4. Data Collection
All patients were hospitalized in the urology ward for seven days after surgery. Every morning for one week after surgery, the patients filled out a questionnaire about the frequency and quality of erection (complete or partial), if any, during the last night/last day separately, and information was recorded. In the dexmedetomidine group, one patient’s catheter was unintentionally removed, and he was excluded from the study and replaced with another patient.
3.5. Statistical Analysis
The data were entered into Microsoft Excel and analyzed using Poisson regression analysis. A P-value of < 0.05 was considered statistically significant.
4. Results
Patients’ characteristics are shown in Table 1. In the DEX group, an average of 0.87 (less than one) erections occurred in seven days. In the ROP group, an average of 1.2 erections occurred. In the control group, 2.8 erections occurred, on average. The results of Poisson regression analysis showed that the number of erections in the control group was 2.7 times the number of erections in the DEX group (P-value = 0.03). The erection occurrence in the control group was 2.1 times the erection occurrence in the ROP group (P-value = 0.04) and it was 0.23 more in the ROP group than in the DEX group, but there was no statistically significant difference between the DEX group and ROP group at the 0.05 level (Table 2).
| N | Mean Number of Erection Incidence in Each Patient | Minimum Number of Erection Incidence in Each Patient | Maximum Number of Erection Incidence in Each Patient | |
|---|---|---|---|---|
| 1.00 | 15 | 0.8667 | 0.00 | 3.00 |
| 2.00 | 15 | 1.2000 | 0.00 | 2.00 |
| 3.00 | 15 | 2.8000 | 0.00 | 8.00 |
| Total | 45 | 1.6222 | 0.00 | 8.00 |
Descriptive Summation
5. Discussion
Urethral reconstruction is a surgical procedure after trauma to the urethra, hypospadias, or urethral stricture. The surgery is most often performed for urethral stricture (or narrowing) reconstruction after traumatic events such as a pelvic fracture. Idiopathic urinary tract stenosis occurs in 0.6% of the general population and is the most common cause, despite known risk factors including trauma, endoscopic interventions, inflammation, and infection (14). The most common symptom is urethral obstruction. However, hematuria, recurrent urinary tract infections, and the impossibility of catheterization during unrelated surgeries or bladder stones also occur (15).
Hypospadias is one of the most common congenital anomalies in boys that require corrective surgery (16). In addition to hypospadias correction surgery, other urinary tract repair surgeries such as urethral tightness repair using oral mucosa are also common surgeries in reconstructive urology. Urethral repair needs graft transfer. The typical grafts that are used in urethral reconstructive surgery are harvested from the inner lining of the mouth. The mouth graft is known as a “buccal graft”. Erection is one of the most important factors leading to complications following reconstructive urethral surgery. The occurrences of erection after surgery before wound-healing completion can place excessive tension on the repair site, as well as repair failure.
To prevent erection after surgery, oral medications such as cyproterone compound and diazepam are commonly used in our institution. Despite the use of these drugs, patients sometimes experience erection episodes. Before deciding to perform this study, because these patients, like other patients undergoing surgery, have postoperative pain in the surgical site, we used to place an epidural catheter for continuous local anesthetic infusion to control postoperative pain in these patients.
Dexmedetomidine is a potent highly selective short-act α2 agonist with sedative and analgesic effects. The α2 agonist agents can reduce norepinephrine secretion by stimulating peripheral α2 presynaptic receptors. In addition, the most important mechanism of dexmedetomidine in penile erection prevention may be due to its α2-adrenoceptor agonistic property by acting on vascular smooth muscle enhancing vasoconstriction in peripheral arteries to prevent erections (8, 9, 17-19).
Hui-Jin Sung showed that the lipid solubility of local anesthetics plays the main role in determining the potency of vasoconstriction induced by local anesthetics at low doses. The disturbing effect of local anesthetics on membrane and lipid solubility associates with the potency of local anesthetics. Transient receptor potential canonical channels are supposed to be involved in determining entry over calcium or sodium channels, which are modulated by cell membrane lipids and anesthetics. The vasoconstriction due to low-dose local anesthetics seems to be essentially dependent on calcium influx over calcium channels (12, 20). A study by GulenGuler et al. showed that the use of intravenous dexmedetomidine can be effective in controlling erection in urinary tract surgery (8). In another study conducted by Ayenayli et al., the use of epidural catheters with a caudal block had a good effect on erection prevention (7). In another study performed by Sengezer et al. investigating epidural catheter insertion and continuous infusion of fentanyl and bupivacaine compared to the group without a catheter, erection did not occur in the group with an epidural catheter, and using this method was recommended to prevent this problem (16). In our study, during the entire seven days of the study, in the first group, 13 erections occurred, including complete and partial erections, amounting to 0.87 per person (Table 2). Erection episodes in the ROP group during seven days was 18, amounting to 1.2 per person, and in the control group, it was 42, i.e., 2.8 per person.
The results of Poisson regression analysis showed that the number of erections in the control group was 2.7 times the number of erections in the DEX group (P-value = 0.03) (Table 2). Erection in the control group was 2.1 times erection in the ROP group (P-value = 0.04). The number of erections was 0.23 more in the ROP group than in the DEX group, but there was no statistically significant difference between the DEX group and the ROP group at the 0.05 level (Table 2). These data showed that the erection occurrence significantly decreased in patients with a continuous epidural infusion of dexmedetomidine and ropivacaine, and they were both less than in patients with only oral medications.
The α2 agonist-induced vasoconstriction and calcium channels modulating effect of ropivacaine may be the main mechanisms of erection prevention with these medications, and they can be used to prevent postoperative erection after urologic reconstructive surgeries. According to the data obtained in this study, dexmedetomidine seems to have a significant effect on erection prevention after genito-urinary reconstructive surgery. Considering that even a single erection episode after reconstructive surgery can lead to wound dehiscence and surgical failure, as well as the need for reoperation and imposing additional costs on patients, epidural dexmedetomidine infusion is recommended for the postoperative period to be effective to prevent erection in these patients. More studies are also recommended on the efficacy of dexmedetomidine for erection in these patients (larger sample sizes and by combining dexmedetomidine with other medications) to minimize the possibility of erection occurrence after reconstructive urethral surgery.