1. Background
Preoperative anxiety is an important phenomenon that influences many patients (1). This condition may affect different body systems, including the cardiovascular, immune and gastrointestinal system. It may also increase heart rate and blood pressure and develop a risk for arrhythmia and heart attack in the presence of underlying diseases. Increased respiratory rate and uptake of oxygen has been reported in the respiratory system. Release of steroids that delay wound-healing, reduce immune system and gastrointestinal activity and sleep disorders such as insomnia, are other complications of anxiety (1). Developing psychomotor impairment increases the patients’ recovery time and treatment costs.
Low-dose benzodiazepines are used for their anti-anxiety and amnesic properties. Diazepam is the most commonly used benzodiazepine. Midazolam, however, due to its short duration of action and lack of specific side-effects, is a better alternative. Melatonin, a pineal hormone, has also been found to be a choice for premedication in adults and lowers the level of anxiety with no amnestic effects (2).
Herbal remedies are now being used to reduce anxiety and increase sedation. Passiflora incarnata is a herbal medication that has significantly similar anti-anxiety effects as midazolam, but causes no psychomotor impairments.
2. Objectives
The present study was conducted to compare the effect of Passiflora incarnata and melatonin on cognitive test results and thereby introduce a drug, which has anti-anxiety and sedative effects without causing cognitive impairment.
3. Methods
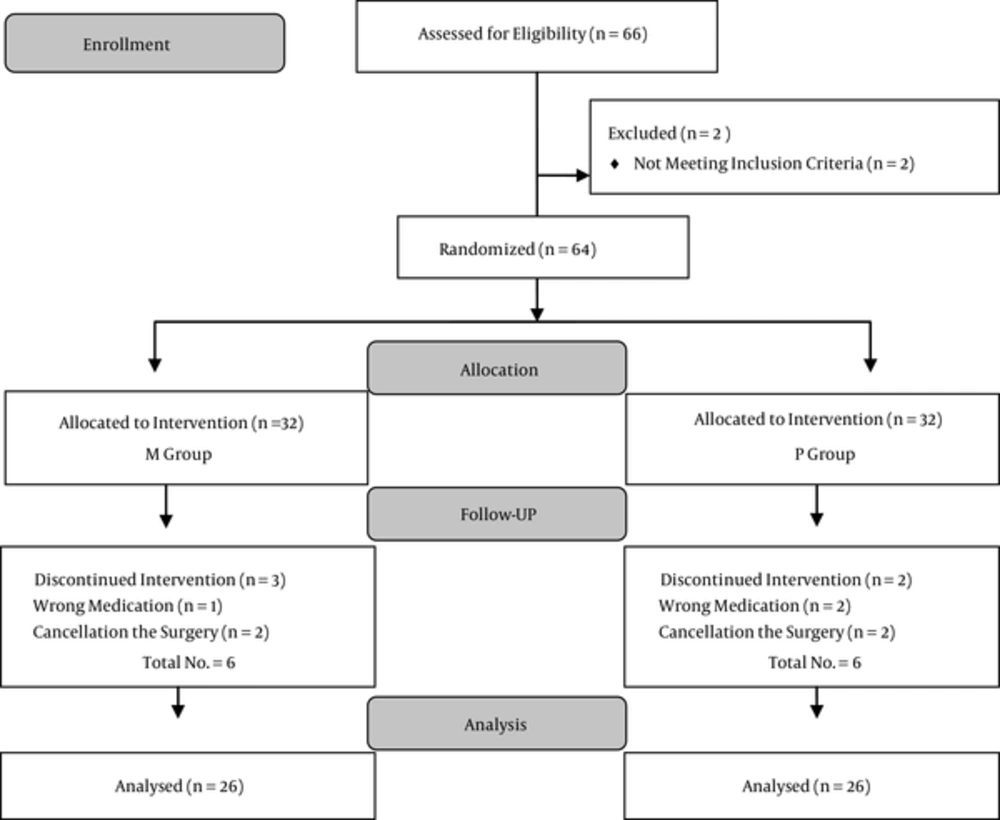
Fifty-two patients aged 20 to 60 years with ASA physical status I and II, candidate for elective minor and intermediate surgery, except neurosurgical procedures, were enrolled. Procedures that had little, modest or intermediate potential to disrupt normal physiology of vital organs and minimum risk of postoperative cardiac or pulmonary complication and less than two hours duration of surgery were selected as minor or moderate surgeries in our study. Exclusion criteria included history of hypertension, diabetes, psychological disorders, mental retardation and being illiterate, history of seizures, use of antidepressant drugs, pregnancy and breast feeding. Informed consent was obtained from all participants before surgery. Approval was obtained from the local ethics committee. The study was registered in the Iranian registry clinical trial center with the following code IRCT13949111174013.
In this double blind randomized clinical trial using a computer derived randomized list, participants were randomly allocated to Passiflora incarnata group (P group, n = 26) and Melatonin group (M group, n = 26). Patients, anesthesiologist and the statistician were blinded to the assignments. Approximately one hour before surgery, patients entered a quiet room in the operating theatre and were monitored with electrocardiogram, pulse oximetry and noninvasive blood pressure control. Peripheral catheterization for crystalloid infusion and oxygen via mask was also applied. Participants in the M group received 6 milligrams of oral melatonin (Nature made Co., USA) and those in the P group received 1000 milligrams of Passiflora incarnata (stress calm), prepared and packed by department of pharmacy, Shahid Beheshti University of Medical Sciences, Iran.
Demographic and hemodynamic data (systolic and diastolic blood pressure (BP), heart rate and respiratory rate, arterial blood oxygen saturation) were recorded for all patients when exiting the post anesthetic care unit (PACU). Post-operative pain was evaluated using the visual analogue scale (VAS) (3-5). Patients’ anxiety and cognitive dysfunction were evaluated with Ramsey score and digital symbol substitution test (DSST), respectively.
Ramsey scale for sedation (1 = patient anxious; 2 =patient cooperativeness; 3 = patient responding to verbal commands; 4 = patient with brisk response to light glabella tap; 5= patient sluggish response to light glabella tap; 6 = patient with no response) (6, 7) was used to evaluate anxiety at the time of entering the operating room, before receiving drugs (melatonin or Passiflora incarnata), one hour after receiving the drugs, before induction and before discharge from the PACU. The patient’s psychomotor condition was evaluated with the DSST at entrance to the operating room, before induction and before discharge from PACU. The chart was shown for 120 seconds to the patient after two minutes, and the DSST chart with some spare spaces was given to the patient to refill for 90-120 seconds (8-10). Visual Analogue scale (VAS) in order to evaluate the pain score was measured one hour after receiving drugs before induction and before discharge from the PACU.
General anesthesia was carried out with fentanyl 2 - 3 mcg/kg, propofol 2.5 mg/kg and atracurium 0.5 mg/kg. After tracheal intubation, anesthesia was maintained with propofol 50 - 100 mcg/kg/min and 10 milligram of atracurium every 30 minutes, and 50 mcg fentanyl if needed. Mechanical ventilation was carried out to maintain End Tidal concentrations of CO2 between 35 - 40 mmHg. At the end of surgery drug infusion was stopped. Neuromuscular blockage was reversed with 0.04 mg/kg neostigmine and 0.02 mg/kg atropine.Student’s t-test was used to examine differences between continuous variables and Mann-Whitney’s U test for categorical variables. P values of less than 0.05 were considered statistically significant. The statistical package for social science (SPSS) for windows, version 21.0 (Chicago, IL, USA) was used for all analysis.
4. Results
Baseline clinical and demographic characteristics of participants are shown in Table 1.
| Melatonin, % | Passiflora incarnata, % | P Value | |
|---|---|---|---|
| Gender | |||
| Male | 11 (42.31) | 12 (46.15) | 0.19 |
| Female | 15 (57.69) | 14 (53.85) | 0.14 |
| ASA | |||
| I | 13 (50) | 15 (57.69) | 0.21 |
| II | 13 (50) | 11 (42.31) | 0.27 |
Abbreviation: ASA: American society of anesthesiologists.
The degree of pain was measured at baseline, before surgery and after surgery. There were no statistically significant differences between groups (P > 0.05). However, the mean score of pain was higher in the M group compared to the P group when discharged from the PACU (27.63 vs. 25.37).
The Friedman’s test was used for the intragroup analyses. The anxiety scores were significantly different with both drugs, and both groups revealed reduced anxiety and increased sedation scores in the Ramsey test (P = 0.001). Regarding the Wilcoxon test, the pre-intervention and post-intervention pain scores was significantly different between the two groups, suggesting a higher sedation score caused by premedication with melatonin (P = 0.003 vs. 0.008).
Regarding the DSST, there was a significant difference between the two groups one hour before the surgery (P = 0.04) and at the time of exiting the operation room (P = 0.007) and Pasiflora was predominant. When evaluating each group, the Passiflora incarnata group revealed a significant difference (P = 0.003).
| Melatonin | Passiflora incarnata | P Value | |
|---|---|---|---|
| Ramsey scale | |||
| Entering the OR | 1.81 | 1.85 | 0.95 |
| Before induction | 1.95 | 1.95 | 1.00 |
| Discharge from PACU | 2.38 | 2.31 | 0.75 |
| DSST | |||
| Entering the OR | 30.67 | 22.33 | 0.04 |
| Before induction | 27.50 | 25.50 | 0.60 |
| Discharge from PACU | 32.10 | 20.90 | 0.007 |
| VAS | |||
| Entering the OR | 26.50 | 26.50 | 1.00 |
| Before induction | 26.50 | 26.50 | 1.00 |
| Discharge from PACU | 27.63 | 25.37 | 0.50 |
5. Discussion
The present study was conducted to compare the effect of premedication with melatonin and Passiflora incarnata on cognitive tests in patients. Our results showed that melatonin has less effect on cognitive tests than Passiflora incarnata. Other studies have emphasized the sedative effect of these drugs. The pain score measured with VAS showed no significant intergroup differences between groups, however mean score of pain was less in the melatonin group. Several studies have been conducted to evaluate postoperative pain after preoperative administration of different drugs and most of them have found valuable results (11-14). It seems that the current study could suggest another drug in this area.
Passiflora incarnata is a herbal medication traditionally used as an anti-anxiety medication and inhibits monoamine oxidase (MAO) activity to reduce depression, stress, anxiety, sleep disorders and restlessness. The anti-anxiety properties of oral Passiflora incarnata begin in 10 - 30 minutes of administration. The postoperative DSST performed in PACU showed more favorable results in the M group compared to the P group. It is used in 500 - 1000 mg doses three times daily. Its side effects are rare and include hypersensitivity, asthma, rhinitis, uterine contractions, nausea, vomiting, arrhythmia and long QT syndrome with long-term use. The likelihood of developing uterine contractions is one of the reasons Passiflora incarnata is prohibited during pregnancy. Passiflora incarnata is also sedative and reduces anxiety and insomnia through stimulating the GABA system. Studies show that this herbal medication has sedative properties without causing psychomotor impairment (15).
Melatonin is produced in the body and influences the reproductive and sleep cycle as an antioxidant, sedative, anti-anxiety and analgesic agent. This hormone is secreted during the day and decreases at night (16). It has receptors in the central nervous system (CNS) and other body tissues. The exogenous oral administration of melatonin at 10 mg doses has positive effects on rapid eye movement (REM) sleep, jetlag, sleep disorders, autism, cluster headaches and smoking cessation anxiety (17). However, this drug is not administered in diabetic patients due to its effects on blood sugar. The anti-anxiety effect of oral melatonin begins within 50 - 90 minutes of administration with the 3 to 15-mg dose. Previous studies have used melatonin as an anti-anxiety and analgesic agent for premedication of adults and obtained similar results to our study (18).
Naguib et al. compared the effects of midazolam and melatonin with that of placebo in reducing pre-operative anxiety and found that midazolam and melatonin increase the sedation score. They also performed the Trieger dot test (TDT) for assessing psychomotor recovery and found more favorable results in the group receiving melatonin (2, 19, 20). Anxiolytic and anesthetic effects of melatonin were also studied and proved in pediatric patients. The study conducted on the analgesic effects of melatonin found that melatonin acts through beta-Endorphins, GABA, opioid receptors, NO and arginine, and affects opioid, muscarinic, benzodiazepine, nicotinic, serotonergic, adrenergic alpha-1 and alpha-2 and MT1 and MT2 receptors in the dorsal horn of the spinal cord and exerts its analgesic effects through the GABA and opioid receptors. The analysis of the effect of melatonin on chronic pain showed that it reduces migraine headache, bloating and pain in patients with inflammatory bowel disease (IBD) (21).
A double-blind study conducted on 32 patients with generalized anxiety disorder (GAD) to compare the effects of the administration of oxazepam and Passiflora incarnata found that oxazepam acts more rapidly but reduces mental and motor activity, leaving Passiflora incarnata a better alternative (22). Similarly in other studies, the pre-operative oral administration of 500 mg of Passiflora incarnata reduced anxiety without causing insomnia (1, 22).
Our study had some limitations. One limitation was that due to different levels of education in our study sample, probable confounding factors might affect our cognitive test results. The other limitation was the use of a quiet and proper setting when the patients were evaluated for the tests.
In conclusion, we found that premedication with Passiflora incarnata reduces anxiety as well as Melatonin. However, Melatonin causes less psychomotor dysfunction compared to Passiflora incarnata. Moreover, no respiratory complications were observed using melatonin. Further possible benefits of melatonin usage as premedication should be evaluated in future studies.