1. Background
Orthodontic patients experience various levels of pain during activation of orthodontic appliances and placement of elastic separators. Pain associated with orthodontic treatment is among the most common complaints of orthodontic patients (1). Pain control is an important aspect of health related quality of life (2-6). Pain is a major factor that discourages patients from continuing orthodontic treatment and is the most commonly reported reason for discontinuation of treatment (in 30% of patients) (7). Moreover, pain associated with orthodontic treatment prevents proper plaque control and negatively affects oral hygiene practices (8). Occurrence of orthodontic pain and its severity are unpredictable and it is not possible to determine which patients and to what extent may experience pain (9). Orthodontic treatment pain affects the overall patient satisfaction with the treatment outcome (10).
An understanding of pain that occurs during orthodontic treatment is also obscured by a lack of knowledge about the reason for pain. However, several explanations have been proposed: Orthodontic mechanical stress may induce localized cells to synthesize prostaglandins and causes inflammatory reactions (11). Prostaglandins, which are among the main inflammatory mediators, mediate orthodontic tooth movement and also increase the transmission of painful stimuli and increase pain (12). Orthodontic pain may also be related to the formation of ischemic areas in periodontal ligament (PDL), which undergo sterile necrosis or hyalinization. Although the reaction of dental pulp to orthodontic forces is insignificant, a mild transient inflammatory reaction, at least at the onset of orthodontic treatment, occurs in dental pulp (13). Moreover, the load applied to teeth by orthodontic appliances is detected by nerve endings in the PDL (14).
Several methods have been proposed to decrease orthodontic pain, such as oral administration of non-steroidal anti-inflammatory drugs (NSAIDs) (9), chewing gum or bite wafers (9), application of local/topical anesthetics (15), transcutaneous electrical nerve stimulation, low-level laser therapy, and vibratory stimulation (16-18). All these methods have some drawbacks as well. For instance, high-dose NSAIDs impair orthodontic tooth movement. Gum or bite wafer chewing is difficult for patients with orthodontic appliances and can also cause bending of orthodontic wires. Local anesthetic agents in patients and particularly children may cause wounds due to biting of the tongue and lips or burns due to the use of hot foods or drinks secondary to local anesthesia (19).
Naproxen sodium marketed under the brand names Anaprox and Diocodal is a NSAID, which inhibits the synthesis of prostaglandins and leukotrienes, and thus, decreases inflammatory reactions. Its chemical formula is 2,6 methoxynaphthalene propionic acid and has a molecular weight of 230.29 g/mol. It has a hepatic metabolism and is well absorbed by the gastrointestinal tract. It has a plasma half-life of 12 to 15 hours and is mainly excreted through the urine. It should not be taken by patients with an active gastrointestinal ulcer. Moreover, it may exacerbate asthma attacks in patients with asthma. It should be taken with caution by patients with renal or hepatic disease. Gastrointestinal complications such as nausea, vomiting, stomachache and gastrointestinal bleeding, skin lesions, rash, and angioedema are the main side effects of this drug (20).
2. Objectives
Studies are required to find an easy, available, and practical solution for orthodontic patients to control pain due to activation of orthodontic appliances. This study sought to assess the efficacy of naproxen gel in decreasing orthodontic pain following elastic separator placement.
3. Methods
Considering the standard deviation of 1.1 for pain reduction, to assess one unit difference between the groups, and taking into account α = 0.05, power of 80%, Zα = 1.96, and Zβ = 0.84, sample size was calculated as 30 patients using the formula below:

The study was approved by the ethics committee of Shahid Beheshti University of Medical Sciences, faculty of dentistry, and registered in the Iranian registry for clinical trials (http://www.irct.ir, identifier: IRCT2016010716466N4).
This double blind randomized controlled clinical trial was conducted on 41 males and females between 14 and 20 years old, who were candidates for fixed orthodontic treatment and required elastic separator placement at the onset of treatment for banding of their first molars. They were selected among those that had referred to a private orthodontic office and an orthodontic clinic affiliated to school of dentistry, Shahid Beheshti University of Medical Sciences during years 2015 and 2016. The data were collected using a questionnaire and the pain score was assessed using a 0 to 100 visual analogue scale (VAS) with intervals of 10 (0- 10- 20-30- … - 100).
The inclusion criteria were age of between 14 and 20 years, no pain at the onset of study (neither dental nor gingival pain), tight contact of permanent first molars with the adjacent teeth in a way that bilateral placement of elastic separators was required at the onset of treatment for banding of first molars, absence of spacing in the respective jaw, presence of opposing teeth for the permanent first molars, absence of posterior open bite, and complaint of pain upon placement of orthodontic elastic separators.
The exclusion criteria were lack of use of naproxen and placebo gels by the patient, not filling the questionnaire, use of other analgesics during the study period, and disengagement of one or both elastic separator(s).
This study had a crossover design to minimize the effect of confounding factors on the results. Since pain perception is subjective, the study had a split-mouth design to minimize individual differences related to pain experience; this design also enabled simultaneous comparison of case and control groups in the same patient.
The gel form of naproxen was used in this study because of its simple application as indicated by previous studies (21).
A neutral gel was used as the placebo and 5% naproxen gel was manufactured in the laboratory of Shahid Beheshti University, School of Pharmacy. The gels were experimentally prepared, tested, and modified a number of times to obtain the final formulation. The obtained formulation was first tested in a pilot study to assess its durability, adhesion properties, taste, analgesic efficacy (determining the most appropriate concentration in terms of adhesion and drug release profile among the 3 gels containing 1%, 2%, and 4% carbomer, which is one of the gel components), and proper method of application. The participants in the pilot study were not included in the main study.
The patients were instructed on how to correctly apply gels along their buccal-free gingival margin by a trained technician. The patients were requested to apply naproxen gel on the gingival margin of their first molar at one side after separator placement and reapply every 8 hours. They were also requested to express their level of pain at 2 and 6 hours and at 10 am and 6 pm of the second, third, and seventh days after the application of gel by marking on a VAS form (with decimal numbers from 0 to 100). The first application of gel was done in the clinic immediately after placement of separators. The results of the pilot study showed that the drug did not have any systemic side effects and the gel contained effective dose of the drug. Also, the results showed that the gel containing 4% carbomer was more suitable in terms of adhesion, gradual wash out by the saliva, and optimal release profile of drug compared to other concentrations. The gel gradually released naproxen following the penetration of saliva into its composition.
The final composition of 5% naproxen gel consisted of carbomer P934 gel forming substance (50 g), preservatives (5 g methylparaben and 1 g propylparaben), glycerin as humectant (400 mL), pH regulator (NaOH), and 10 g naproxen powder (South China Pharmaceutical Company, Shenzhen, China).
After confirming the final composition, the gels were supplied in 100 eye dropper bottles of 8 mL volume. Each bottle contained 4 grams of gel. Written informed consent was obtained from all patients. Separators (American Orthodontics, Monrovia, CA, USA) were placed at the mesial and distal of permanent first molars in the right and left sides of one jaw, using orthodontic separator pliers (Dentaurum, Springen, Germany). Necessary instructions were given to patients based on primary assessments in the pilot study. Patients applied naproxen and placebo gels (allocation of type of gel to each quadrant was random and was done by an assistant in the clinic) and reapplied every 8 hours for 3 days. The patients and the assistant were blinded to the type of gels. Each patient was provided with a 0 to 100 VAS form to record the level of pain experienced at the designated time points. The assessment time points were selected based on previous studies (7, 21-26). In the VAS, 0 indicated analgesia while 100 indicated the maximum pain imaginable. Patients were asked to use acetaminophen tablets or their drug of choice if they were disturbed by pain, yet, they were asked to mention the usage (they were replaced by other individuals, who did not use any analgesics). The age and gender of patients were also recorded and they were requested to contact the phone number provided in the form in case of any question or problem regarding the use of gels.
The data were extracted from the questionnaires by a statistician, who was blinded to the type of gel, and normal distribution of data was assessed by the Kolmogorov-Smirnov test. The data were normally distributed and paired samples t test was used to compare the level of pain between the 2 types of gels. Pairwise comparisons of time points were made using the Bonferroni method. The difference in pain severity between males and females and patients > 16 and ≤ 16 years was analyzed using multi-factorial repeated measures analysis of variance (ANOVA). P values of < 0.05 were considered statistically significant.
4. Results
The gels were supplied in 100 eye dropper bottles. Each bottle contained 4 grams of gel. The total amount of the used naproxen in the present study was 10 mg. Of the 41 patients, who experienced pain at the onset of orthodontic treatment, 34 remained in the study until the end of the experiment and returned the questionnaires (7 were lost to follow-up). Of the patients, 23 (67.6%) were female and 11 (32.4%) were male with a mean age of 16.88 ± 1.64 years (range 14 to 20 years). Normal distribution of the data at all time points and at both sides (drug and placebo) was confirmed by the Kolmogorov-Smirnov test (all P values were > 0.05).
The pain score by using the naproxen gel was significantly decreased over time during the 8 consequent times (multiple repeated measures ANOVA, P < 001; Table 1). Also significant differences were noted among most of the time points (Bonferroni method, Table 2).
| Time | Group | Minimum | Maximum | Pain Scorea | P Value |
|---|---|---|---|---|---|
| 2 h | Naproxen | 0 | 80 | 56.91 ± 17.36 | 0.001 |
| Placebo | 15 | 85 | 63.52 ± 15.49 | ||
| 6 h | Naproxen | 5 | 100 | 54.85 ± 16.07 | 0.003 |
| Placebo | 10 | 100 | 62.35 ± 18.83 | ||
| 10 am on the second day | Naproxen | 10 | 100 | 46.47 ± 16.30 | 0.000 |
| Placebo | 30 | 100 | 59.55 ± 15.14 | ||
| 6 pm on the second day | Naproxen | 10 | 100 | 41.61 ± 15.94 | 0.000 |
| Placebo | 15 | 100 | 54.7 ± 16.91 | ||
| 10 am on the third day | Naproxen | 5 | 75 | 38.08 ± 14.66 | 0.000 |
| Placebo | 10 | 75 | 48.97 ± 14.18 | ||
| 6 pm on the third day | Naproxen | 0 | 60 | 33.38 ± 14.49 | 0.000 |
| Placebo | 0 | 60 | 44.11 ± 14.27 | ||
| 10 am on the seventh day | Naproxen | 0 | 25 | 5.6 ± 5.26 | 0.003 |
| Placebo | 0 | 20 | 9.54 ± 6.88 | ||
| 6 pm on the seventh day | Naproxen | 0 | 20 | 4.84 ± 4.75 | 0.003 |
| Placebo | 0 | 20 | 8.33 ± 5.81 |
aValues are expressed as mean ± standard deviation.
| Group 1 | Group 2 | Mean Differencea | P Value |
|---|---|---|---|
| 2 h | 6 h | 1.67 ± 0.79 | 1 |
| 10 am on the second day | 7.57 ± 1.55 | 0.001 | |
| 6 pm on the second day | 12.34 ± 1.81 | < 0.001 | |
| 10 am on the third day | 16.89 ± 1.75 | < 0.001 | |
| 6 pm on the third day | 21.59 ± 1.9 | < 0.001 | |
| 10 am on the seventh day | 53.86 ± 2.34 | < 0.001 | |
| 6 pm on the seventh day | 54.84 ± 2.35 | < 0.001 | |
| 6 h | 10 am on the second day | 5.9 ± 1.23 | 0.001 |
| 6 pm on the second day | 10.68 ± 1.42 | < 0.001 | |
| 10 am on the third day | 15.22 ± 1.57 | < 0.001 | |
| 6 pm on the third day | 19.92 ± 1.85 | < 0.001 | |
| 10 am on the seventh day | 52.19 ± 2.53 | < 0.001 | |
| 6 pm on the seventh day | 53.18 ± 2.54 | < 0.001 | |
| 10 am on the second day | 6 pm on the second day | 4.77 ± 0.9 | < 0.001 |
| 10 am on the third day | 9.31 ± 1.02 | < 0.001 | |
| 6 pm on the third day | 14.01 ± 1.49 | < 0.001 | |
| 10 am on the seventh day | 46.28 ± 2.43 | < 0.001 | |
| 6 pm on the seventh day | 47.27 ± 2.42 | < 0.001 | |
| 6 pm on the second day | 10 am on the third day | 4.54 ± 0.98 | 0.002 |
| 6 pm on the third day | 9.24 ± 1.3 | < 0.001 | |
| 10 am on the seventh day | 41.51 ± 2.58 | < 0.001 | |
| 6 pm on the seventh day | 42.5 ± 2.55 | < 0.001 | |
| 10 am on the third day | 6 pm on the third day | 4.69 ± 0.812 | < 0.001 |
| 10 am on the seventh day | 36.97 ± 2.14 | < 0.001 | |
| 6 pm on the seventh day | 37.95 ± 2.1 | < 0.001 | |
| 6 pm on the third day | 10 am on the seventh day | 32.27 ± 2.17 | < 0.001 |
| 6 pm on the seventh day | 33.25 ± 2.1 | < 0.001 | |
| 10 am on the seventh day | 6 pm on the seventh day | 0.98 ± 0.28 | 0.046 |
aValues are expressed as mean ± standard error.
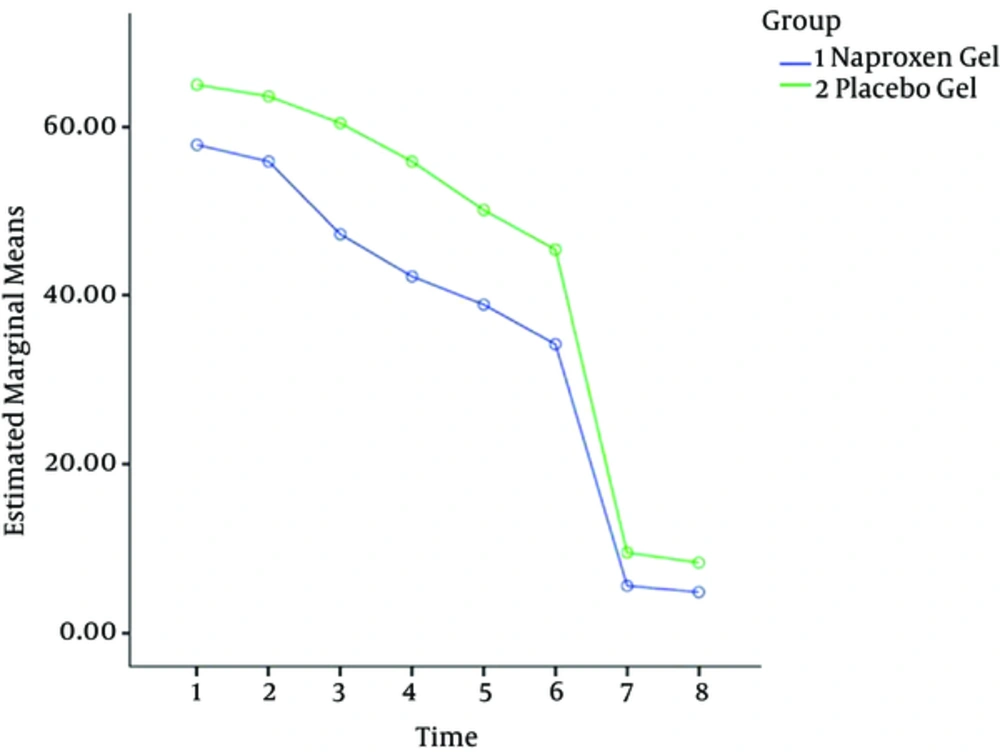
In other words, as seen in Figure 1 the pattern of pain reduction in the 2 methods was not equal over time and had some variations.
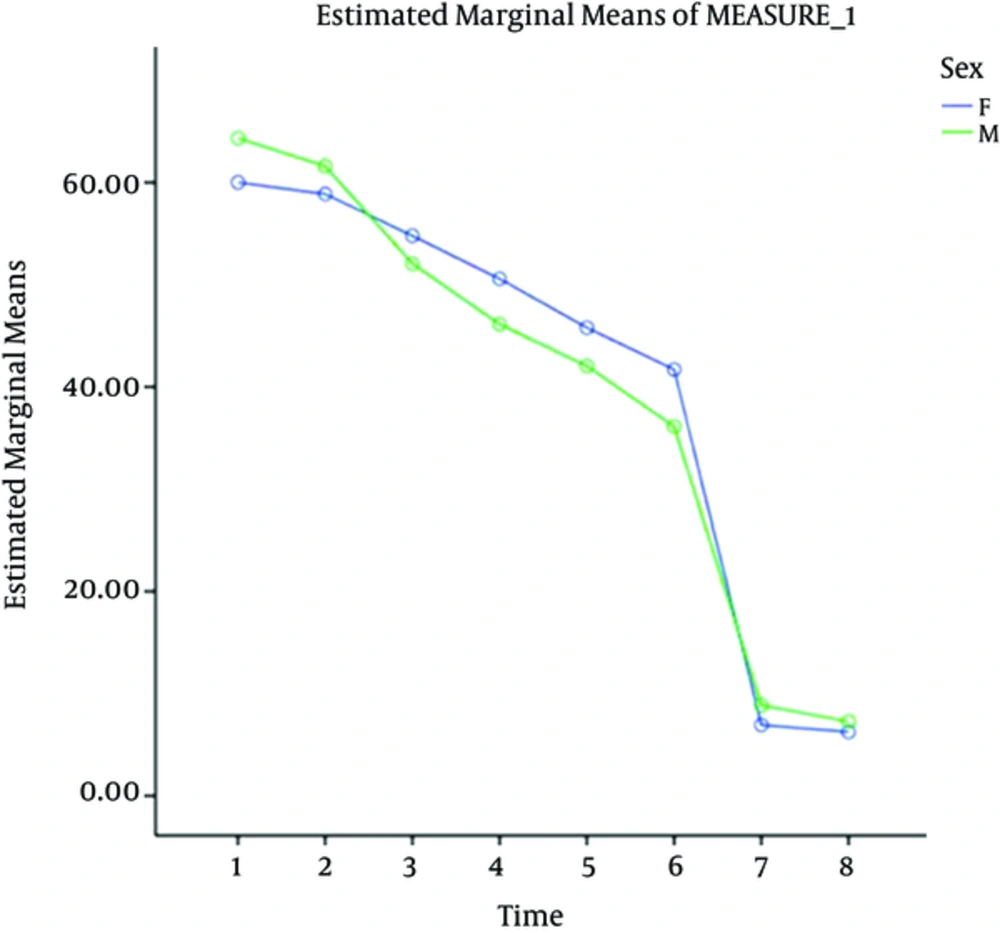
Variations in the severity of pain in the 2 groups of males and females were analyzed using multifactorial repeated measures analysis of variance (ANOVA). As seen in Figure 2, the level of pain was not significantly different in males and females (P = 0.824).
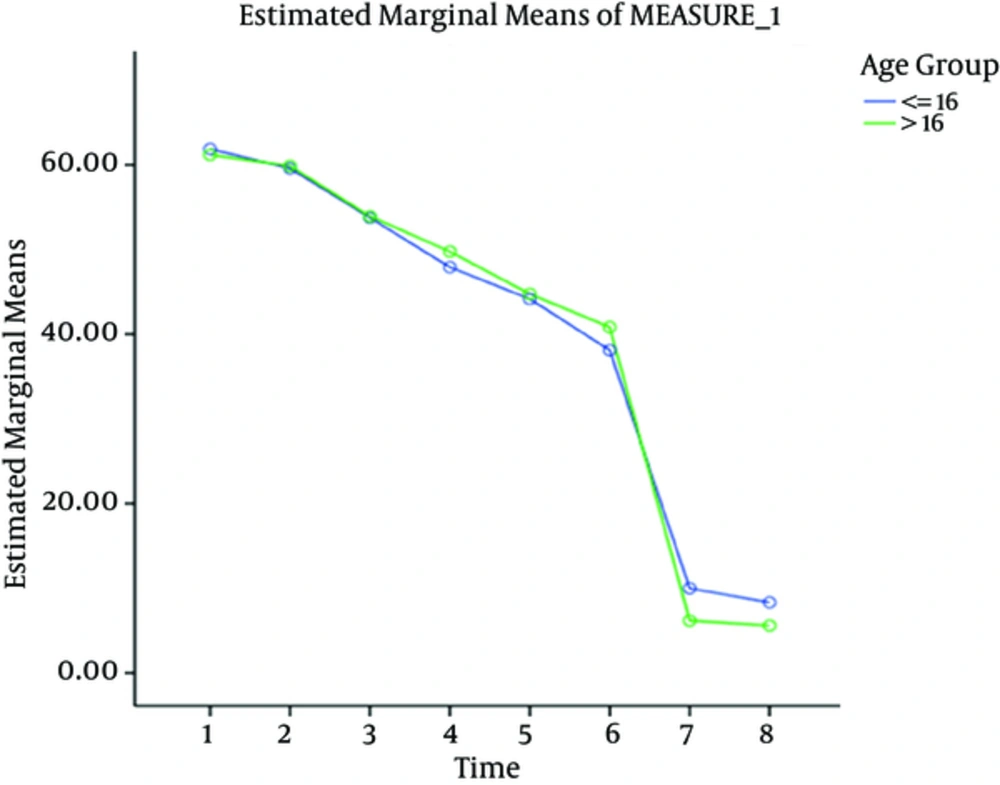
Pain score was also compared between patients ≤ 16 and > 16 years of age using multifactorial repeated measures ANOVA. As depicted in Figure 3, the level of pain was not significantly different in the 2 age groups (P = 0.955).
5. Discussion
This study compared the analgesic efficacy of 5% naproxen and placebo gels following placement of separators in patients under fixed orthodontic treatment using VAS at 2 and 6 hours and on the second, third, and seventh day, and revealed that both the type of gel and time had significant effects on pain score (P < 0.001); the highest pain score was noted at the placebo side while the lowest pain score was noted at the naproxen side and this difference was statistically significant (P < 0.001). In pairwise comparisons, the difference in pain scores at 2 and 6 hours was not statistically significant, yet, the difference between other time points was statistically significant in this regard.
Since pain perception is subjective, this study had a within-subject design to decrease the effect of confounding factors on pain experience. Only a few studies on the analgesic efficacy of drugs for orthodontic pain control had a split-mouth design such as the studies by Eslamian et al. in 2013 (22, 24). Several previous studies used questionnaires and VAS to assess the level of pain experienced by fixed orthodontic patients (26-32). This method enables assessment of changes in pain severity over time and it has been reported that VAS is efficient for assessment of the analgesic efficacy of anti-inflammatory drugs (32). In the current study, a great variability was noted in pain scores of patients. Some patients even reported greater pain in the naproxen side, which may be due to factors such as low pain threshold of the patient, stress, patient’s psychological status, cultural differences, and previous pain experiences (33).
In the current study, the drug was prepared in gel form. Thus, after consultation with a pharmacist and based on the results of the pilot study, the most suitable adhesion properties and drug release profile were noted in the compound containing 4% carbomer (among 1%, 2%, and 4% compounds); this concentration minimized problems associated with simultaneous use of naproxen gel and placebo. Due to the split-mouth design of the study, the case and control groups could be compared in the same patient and the effect of confounders such as the masticatory forces and the effect of referred pain, which does not cross the midline was minimized as such, therefore, the case and control groups were matched as much as possible.
Placement of a separator is often associated with significant pain in the clinical setting, however, individual differences exist among patients and some individuals experience no pain during this process. The advantage of using elastic separators for pain induction in the current study was enhanced matching of samples. Eslamian et al. in 2009 (23), Patel et al. in 2011 (25), and Eslamian et al. in 2013 (22), also used elastic separators for pain induction.
In the current study, patients had to be selected in such a way to maximize the possibility of pain generation in them in order to better assess the analgesic efficacy of the drug. Thus, the inclusion criteria were set in such a way that separators applied a certain amount of load on the first molars (tight contact of first molars with the adjacent teeth, presence of opposing teeth at both sides and occlusal contact of first molars with them, and absence of posterior open bite). Minimum age of patients was 14 years since a tight contact between the permanent first molars and adjacent teeth as well as optimal patient cooperation were among the inclusion criteria for this study. To narrow the age range of patients, subjects between 14 and 20 years old were included. This narrow age range was among the strengths of this study.
In this pilot study, 5% concentration of naproxen was chosen as the lowest effective dosage. Also, 8-hour intervals for gel application were chosen based on a previous study by Eslamian et al. (21) and also according to the instructions provided by naproxen manufacturers, in order to decrease possible side effects and enhance patient cooperation.
No similar previous study was found on naproxen gel, and limited studies are available on the efficacy of naproxen for decreasing pain associated with fixed orthodontic treatment. Polat et al. in 2005 compared the analgesic efficacy of lactose capsules (placebo, control group), 400 mg ibuprofen, 100 mg flurbiprofen, 500 mg acetaminophen, 550 mg naproxen sodium, and 300 mg aspirin in patients after bonding of 0.014 and 0.016-inch arch wires; 120 patients (6 groups) expressed their level of pain and discomfort at 2 and 6 hours, during sleep on the same day and at 24 hours, 2, 3 and 7 days after bonding using 0 to 100 VAS. Level of pain at two hours after bonding in the naproxen sodium and aspirin groups was significantly lower than that in the placebo group (26).
Patel et al. in 2011 assessed the analgesic efficacy of ibuprofen, naproxen sodium, acetaminophen, and placebo tablets at 24 hours after placement of separators in 24 patients. Each patient received 3 of the 4 choices (randomly in monthly periods). The patients took tablets 1 hour prior to placement of separators and during the next 3 and 7 hours, and used a VAS to express their expected level of pain and experienced pain. Administration of ibuprofen after placement of separators significantly affected the VAS score (P = 0.0298). A significant association was noted between time of assessment after placement and pain score (P < 0.0001). The analgesic efficacy dropped on day 2 and led to a high level of pain and decreased the efficacy of mastication. Also, patients, who expected higher level of pain experienced more pain than others (25). Their findings were in contrast to our results because in the current study, pain scores at 2 and 6 hours and at 2, 3, and 7 days after gel application were significantly different between the 2 groups of naproxen and placebo. Moreover, the total pain score at all-time points was lower in the naproxen group than the placebo group.
The analgesic efficacy of other NSAIDs in gel form has also been evaluated in previous studies. Eslamian et al. in 2008 compared the efficacy of 100 mg/160 mL ketoprofen gel and 5% benzocaine gel for orthodontic pain control after each visit. Their study was a cross over double-blind controlled clinical trial and was conducted on 30 patients between 15 and 25 years old. Each patient at each visit randomly received ketoprofen, benzocaine or placebo gel and expressed the level of pain using VAS; 22 patients returned the VAS questionnaires filled out at 2, 6, and 24 hours and also at 2, 3, and 7 days after the use of each gel. They showed that ketoprofen had higher analgesic efficacy than the control and benzocaine gel; the difference in this respect between the ketoprofen and control group was statistically significant. Moreover, the highest level of pain in the 2 groups of control and ketoprofen gel was noted at 2 hours after the application of gel, which subsided overtime. This finding was in line with the results of the current study. In use of 5% benzocaine gel, the severity of pain was the highest at 6 hours after the activation of orthodontic appliance (21).
Reports regarding the effect of age and gender on orthodontic pain are controversial and many studies did not find a significant association between pain and gender of patients (16, 34). The current study found no significant difference in pain score in the case or control groups between males and females (P = 0.824); the same result was obtained by Eslamian et al. in 2009 (23). Kleumper et al. in 2002 (15) also confirmed this finding.
No significant difference was noted in pain score between the 2 groups of > 16 and ≤ 16 years old (P = 0.955) in the current study, which was probably due to the narrow age range of patients. In the study by Eslamian et al. (23) no significant difference was noted in pain score of patients ≤ 18 and > 18 years. However, in another study by Eslamian et al. in 2013 an inverse correlation was found between the severity of pain and age; in other words, pain decreased with age (22). Moreover, Brown and Moerenhout mentioned that patients between 14 and 17 years of age experienced higher level of pain compared to those younger than 13 years and over 18 years (35). Scheurer et al. demonstrated that maximum pain was reported by patients aged 13 to 16 years old (36).
The NSAIDs exert strong analgesic effects by inhibiting the synthesis of chemical mediators (37). In dentistry, naproxen sodium is used to alleviate mild to moderate pain, which may be toothache, postoperative pain following oral surgery or pain of the temporomandibular joint. For mild pain, 220 mg naproxen sodium is administered every 8 to 12 hours, which has an efficacy equal to that of 200 mg ibuprofen administered every 4 to 6 hours. For more severe pain, such as pain after oral surgery, 440 mg naproxen has higher analgesic efficacy than 1000 mg acetaminophen; the efficacy of 440 mg naproxen is equal to that of 400 mg ibuprofen (38).
Future studies are recommended to compare the efficacy of naproxen gel with other forms of drug with the same dosage for local pain relief since the total amount of the used naproxen in the present study was only 10 mg. Also, the analgesic efficacy of naproxen gel should be compared with that of other analgesic gels.
5.1. Conclusions
The highest and lowest pain score was noted at 2 hours and at 7 days after separator placement. Considering the presence of significant differences in pain scores between the case and controls at all time points, it may be concluded that naproxen gel can relieve orthodontic pain associated with elastic separator placement.