1. Background
In the treatment of malignancy and solid tumors, cisplatin acts as a strong anti-tumor compound. However, the chemotherapeutic property of cisplatin is limited because of its severe side effects such as ototoxicity and nephrotoxicity, which leads to decrease in cisplatin usage (1-3). Furthermore, cisplatin decreases antioxidant power in chemotherapy, as antitumor drugs induce production of free-radicals (4, 5). In previous studies, cisplatin-induced nephrotoxicity is strongly associated with increase in lipid peroxidation in kidney tissues (6). Propofol (2,6-diisopropylphenol) is a widely used intravenous sedative-hypnotic agent for both induction and maintenance of anesthesia and sedation in critically ill patients (7). Structure of the propofol contains a phenolic hydroxyl group and thus resembles that of α-tocopherol (vitamin E), a natural antioxidant. As shown by both in vitro and in vivo studies, the antioxidant activity of propofol results partly from this phenolic chemical structure (8).
Some studies have demonstrated antioxidant effects of propofol in vitro (9, 10) and some in vivo (11). However, propofol affects differently on different cells, and multiple mechanisms may be involved (12) in that. On the other hand, it has been reported that the antioxidant properties of propofol not only inhibit lipid peroxidation, but also scavenger and remove ROS that have been formed (8). Previous studies showed that induction of nephrotoxicity in cisplatin exposure is strongly associated with lipid peroxidation induction in kidney tissues (13). Recently, nephrotoxicity of cisplatin is controlled by sulforaphane through inhibition of antioxidant enzymes and decrease in oxidative or nitrosative stress (2, 14).
2. Objectives
In the present study, we investigated antioxidant properties of propofol on nephrotoxicity in rats treated with cisplatin.
3. Materials and Methods
Trichloroacetic acid (TCA), tetraethoxypropane (TEP), 2, 4, 6 tripyridyl-s-tiazine (TPTZ), 2-thiobarbituric acid (TBA), n- butanol, 2 thionitrobenzoic acid (DTNB), propofol (propofol-Lipuro 1%: Braun Melsungen AG Germany), ethylenediaminetetraacetic acid (EDTA), and cisplatin were used in this study. All other chemicals were obtained from the Sigma.
3.1. Animals and Treatments
In this experimental study, we used male Wistar rats of 180-250 g body weight kept at a 12:12 h light-dark cycle with free access to drinking water and standard laboratory chow. Animals were randomly divided into six groups (5 rats in each group) and then, treated intraperitoneally (IP) for one week.
The design of these treatments resulted in four experimental groups. The groups were as follows: propofol group, control group, cisplatin group, and propofol with cisplatin group. Then, propofol was administered (10 mg/kg/day, IP) (15, 16) alone or in mixture with cisplatin (7 mg /kg/day, IP) (13, 17). Also, control group received only normal saline. Finally, animals were killed 24 hours after the last dose of treatment, and their blood was taken. Blood samples were collected in heparinized tubes, and plasma was immediately separated.
3.2. Kidney Parameters
In present study, blood urea nitrogen (BUN) and creatinine (Cr) levels were measured by automated biochemistry machine aaccording to the standard procedure of Pars azmoon kits.
3.3. Oxidative Stress Biomarkers
Oxidative biomarkers in this study such as lipid peroxidation, total antioxidant capacity and total thiol molecules were measured.
3.4. Measurement of Lipid Peroxidation
In this method, lipid peroxidation (LPO) product in the tissues was determined by thiobarbituric acid (TBA) reagent during an acid heating reaction that expressed the amount of malondialdehyde (MDA) production. At the end, calibration curve of tetramethoxypropane standard solution was used to determine the concentrations of TBA- MDA adduct in the samples (18).
3.5. Measurement of Total Antioxidant Capacity
In this study, total antioxidant capacity (TAC) was calculated with ferric reducing ability of plasma (FRAP) assay. This process is founded upon the ability of plasma in reducing Fe3 + to Fe2 + in the presence of TPTZ. Also, the reaction of Fe2 + with TPTZ gives a complex with blue color and maximum absorption at 593 nm (19).
3.6. Assay of Total Thiol Molecules
In this protocol, total thiol molecules (TTG) evaluated with DTNB reagent. Thiol molecules react with DTNB and create a yellow complex with excellent absorption in spectrophotometer at 412 nm (20).
3.7. Statistical Analysis
Reported data were mean ± SEM of at least three independent experiments performed two times or more. The 1-way analysis of variance (ANOVA), followed by a Tukey post hoc test, was used to compare multiple groups, and all comparisons were significant when P < 0.05.
4. Results
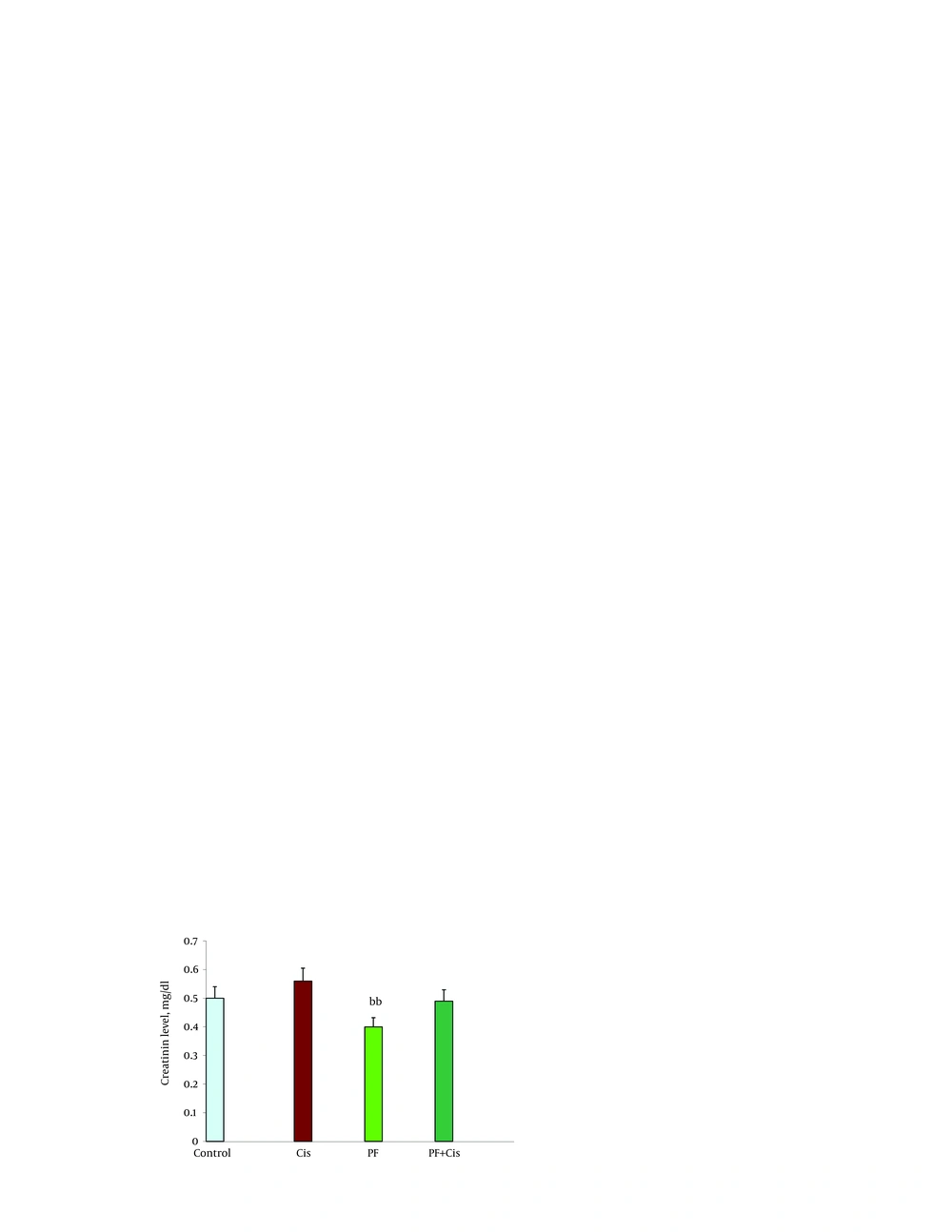
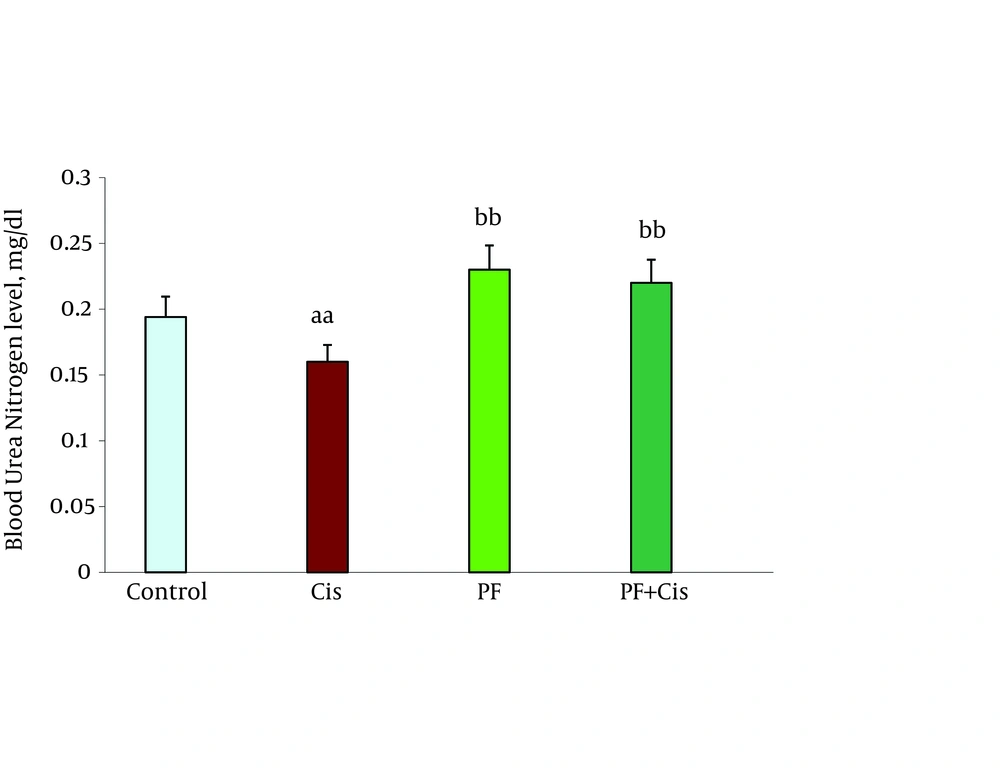
Kidney parameters of creatinine (Cr) level and blood urea nitrogen (BUN) in animal tests are shown in Figure 1 and 2. Propofol caused a significant reduction in Cr and BUN compared with the control group (P = 0.001, P = 0.02, respectively).
4.1. Oxidative Stress Parameters
4.1.1. Lipid Peroxidation
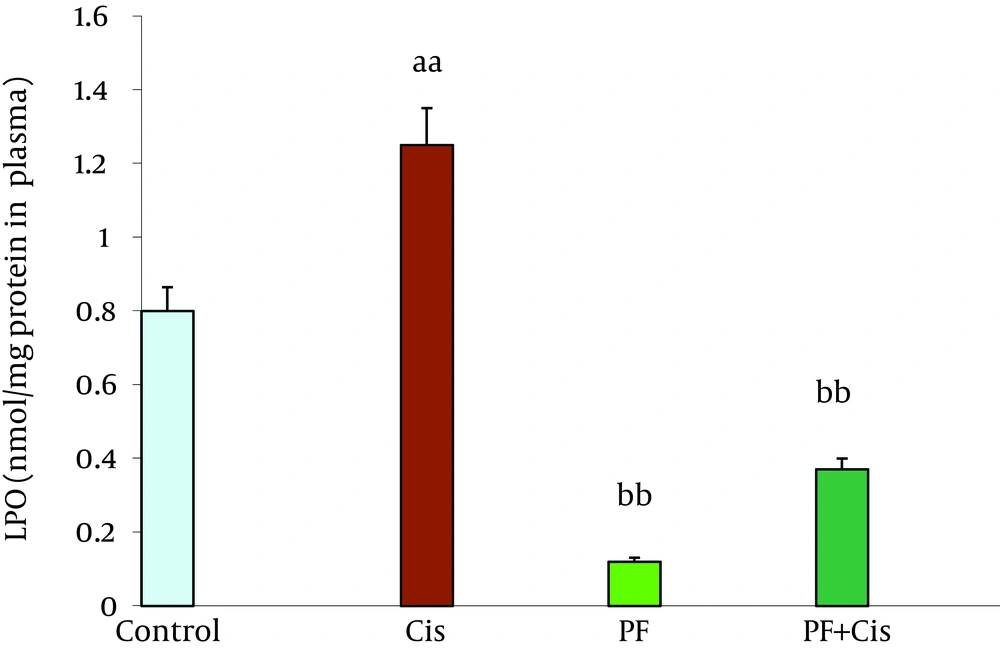
Cisplatin changed a significant increase in LPO compared with the control group (P = 0.03). Propofol induced a significant decrease in LPO compared with the cisplatin group (P = 0.03). Coadministration of cisplatin with propofol decreased cisplatin-induced LPO (P = 0.04) (Figure 3).
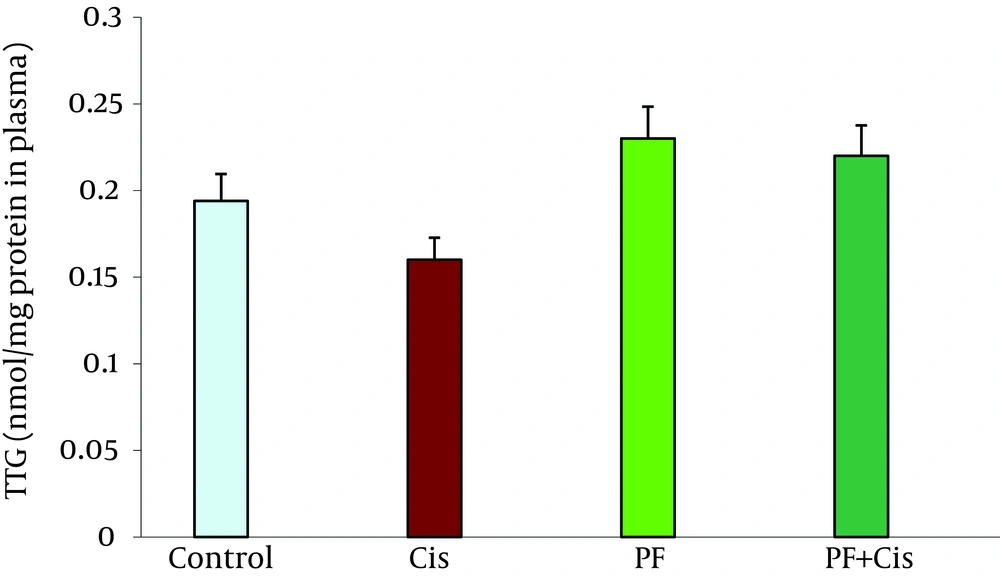
4.2. Total Thiol Molecules
The value of TTG in propofol group was not significantly different from the control and other groups (Figure 4).
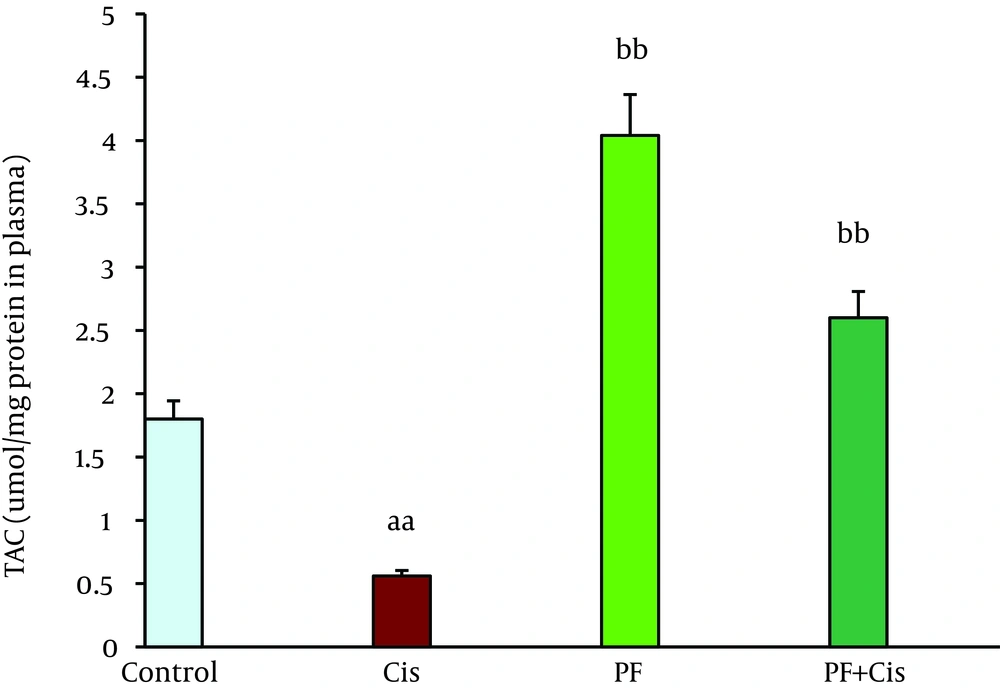
4.3. Total Antioxidant Capacity
Cisplatin caused a significant decrease in TAC when compared with the control group (P = 0.001). Treatment with propofol improved TAC compared with the cisplatin group (P = 0.04). Coadministration of cisplatin with propofol significantly increased TAC level compared with the cisplatin group (P = 0.02) (Figure 5).
5. Discussion
General findings in this study showed the possible toxicity of cisplatin through increasing oxidative injuries. Results indicated that oxidative markers such as LPO, TAC, and TTG are stimulated in contact with cisplatin, although their defense is not sufficient to induce free radicals production. The present results also showed that TTG is decreased by cisplatin. However, propofol indicates antioxidant properties throhout reduction oxidative stress induced by cisplatin. On the other hand, cisplatin toxicity of oxidative reactive agents is characterized by increase in BUN and Cr in the serum. Indeed, oxidative stress induction in cisplatin toxicity is indicated by the increase in ROS and fouling cellular damage as shown by an increase in LPO and decrease in TAC and TTG.
Propofol effect may be due to its chemically similar structure to endogenous antioxidant α-tocopherol (Vitamin E) and theoretically should show similar properties (21). The present result indicates reduction of LPO in the propofol treatment group induced by cisplatin. Numerous antioxidants as free radical scavengers, including flavonoids, vitamin E and vitamin C were reported to have various protective effects in cisplatin-induced damage (4, 22, 23). The antioxidant effects of propofol may also be due to its capacity in attenuating the formation of lipid peroxides (24), inducing the expression of antioxidant enzyme home oxygenase-1 (10), decreasing the expression of nitric oxide synthase (NOS), (25) and fixing the mitochondrial membrane (26).
Our findings showed that, propofol activates oxidative biomarkers against cisplatin toxicity in plasma. In kidney, cisplatin increases production of oxidative stress biomarkers in nephrotoxicity (13, 27) and produces ROS such as hydroxyl radical and superoxide anion (14, 28). Previous studies showed that increased cisplatin induces LPO biomarkers production such as MDA, 4-hydroxy-2-nonenal (4-HNE), and 8-isoprostane (27, 29, 30). We think it is due to the antioxidant properties of propofol in the blood. Propofol was also shown to endorse mitochondrial activity by stabilizing the transmembrane electrical potential (31, 32) and inhibiting mitochondrial permeability transition pore openings (33), both contributing to suppression of mitochondrion-dependent apoptotic signaling (34).
The damages induced by cisplatin are resulted from free radicals through lipid peroxidation of cell membranes, reduction in antioxidant enzyme and antioxidant substrates to induce oxidative stress, which is the main factor in acute and chronic injuries in different tissues (35). In this study, cisplatin exposure causes a significant increase in LPO production. Most significantly, propofol decreased LPO (Figure 3). These findings are consistent with previous investigations using a variety of antioxidant uptakes (36-38). Recently, in vitro studies showed that propofol could efficiently suppress apoptotic signaling and prevent apoptotic death of myocardial cells encountering fatal stimuli (10, 39, 40). Propofol in experiments on heart tissuess, reversed mitochondrial permeability transition (33) and reduced ischemia–reperfusion damage (41-43). These conclusions support the idea that propofol can prevent the sequences of oxidative stress. Interestingly, as evidenced oxidative damage, these results verify that cisplatin-induced oxidative damage could be improved by propofol. Nevertheless, the strict molecular and cellular mechanisms of an accepted role of propofol (protective role) should be investigated in the future.