1. Background
Establishing a secured airway via Endotracheal Tube (ETT) by anesthesiologists is a daily practice in the operating room theater since 1950s. To maintain an effective ventilation with minimized risk of aspiration and tracheal wall damage, the Endotracheal Tube Cuff Pressure (ETCP) should be kept in the range of 20 - 30 cm H2O (1). Overinflation is associated with several complications such as sore throat and hoarseness (2), laryngeal nerve palsy (3), tracheal rupture (4), stenosis (5, 6), and tracheo-esophageal fistulae (7). Although pilot balloon palpation is the most common technique of ETCP assessment in the clinical setting, its accuracy is disputed (8-11). Earlier studies suggested that measurement of ETCP with monometer is mandatory to reduce the rate of complications (12, 13). However, in daily practice, the manometer may not be available all the times and estimation techniques may be used instead. Some reports suggested that experience of anesthesia staff may improve the safety of palpation technique (14) and some others proposed a negative role for the experience (15). To the authors' best knowledge; all of the earlier surveys evaluated the performance of medical staff without conducting any educational program. In fact, the practice of anesthesia personnel might not be challenged during the years of their professional career.
2. Objectives
The current study aimed to evaluate the effect of an in vitro educational program on the ability of anesthesia personnel to inflate endotracheal tube cuffs within safe pressure limits.
3. Patients and Methods
3.1. Study Protocol
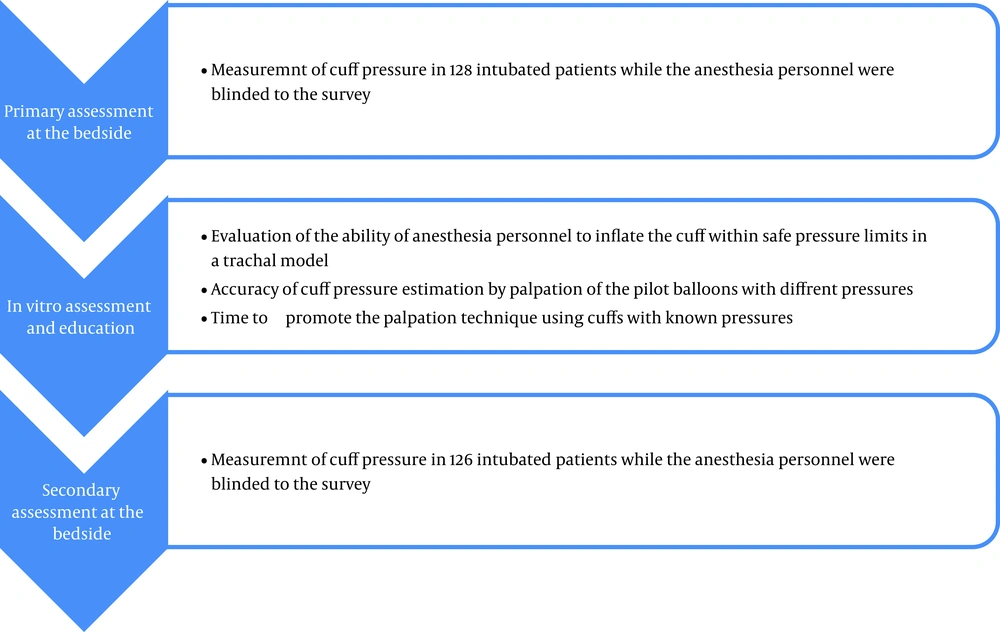
The local ethics committee approved the study protocol (Figure 1). The survey included two series of ETCP measurements in the intubated patients before and after an in vitro educational intervention. In the first step, the ETCP in 128 intubated patients was measured, where the anesthesia personnel were unaware of the survey. Thereafter, 52 anesthesia personnel (anesthetists, anesthesia residents, and technicians) were asked to inflate an ETT cuff inserted in a tracheal model with their usual inflation technique. The pressure of inflated cuffs was measured using a manometer. In the same session, the ability of anesthesia staff to estimate the ETCPs in a series of six ETTs with different cuff pressures was evaluated. After the assessment, the participants were informed about the actual ETCPs and were allowed to train their fingers by in vitro pilot balloon palpation with validated manometer measurements. Two weeks later, the ETCPs in 126 intubated patients were measured, where the anesthesia personnel were unaware of the measurements. Details of assessments followed.
3.2. Ability to Inflate the Endotracheal Tube Cuff Within Safe Pressure Limits
Fifty-two anesthesia personnel (anesthetists, anesthesia residents and technicians) were asked to inflate a polyvinylchloride (PVC) endotracheal tube cuff (Supa, Tehran, Iran) inserted in a tracheal model using their usual inflation technique. The ETT size was 7.5 mm internal diameter (ID), which is the most frequent administered size for the purpose of intubation in the center. The tracheal model included a syringe with 20 mm ID. The syringe was covered with a paper and the participants could not see the inflating cuff. The ETCP was measured with a noninvasive manometer (cuff controller digital 0 - 120 cm H2O, VMB Medizintechnik GMBH, Germany) connected to the pilot balloon.
3.3. Accuracy of Endotracheal Tube Cuff Pressure Estimation by Palpation of the Pilot Balloon
Six endotracheal tubes at different pressure levels were examined by the participants and their estimation of ETCPs was recorded. The ETCPs included 65, 25, 10, 50, 25, and 100 cm H2O. The pilot balloons were numbered sequentially and participants were asked to report the cuff pressures in the same order. The ETT cuffs were placed in a cover and only the pilot balloons were exposed. At the end of assessments, anesthesia personnel were allowed to train their fingers by in vitro pilot balloon palpation with validated manometer measurements.
3.4. Assessment of Endotracheal Tube Cuff Pressure in the Intubated Patients
The ETCPs in 128 intubated patients were measured before and in 126 patients two weeks after the in vitro educational intervention. Either periods of data acquisition included six consecutive days to reduce the probability of selection bias. Inclusion criteria were elective surgery from different specialties requiring general anesthesia and oral intubation with the surgery in the supine position. Patients with head, neck or laryngeal surgery, or those requiring placement of a nasogastric tube were excluded. The position of the head and neck in the recruited patients was neutral during the surgery. Trachea was intubated by either attending anesthesiologist, anesthesia residents or technicians with 7 to 8.5 mm ID cuffed PVC tube. The anesthesia personnel were blinded to the survey and were free to inflate the cuff of ETT as per their clinical judgment. Induction and maintenance of anesthesia was performed with the method of the choice of anesthesiologist, but nitrous oxide was not administered in any of patients. All ETCP measurements were performed within 10 minutes of intubation by the same observer using a noninvasive manometer (VMB Medizintechnik GMBH, Germany). Cuff pressure measurements were performed at the end of expiration. Once the pressure was measured, it was adjusted to normal range. The assessment protocol was the same in the two series of measurements.
3.5. Statistical Analysis
The primary objective of the study was to compare the ETCPs falling outside the recommended range before and after in vitro intervention. The sample size was calculated based on the estimation equation of sample size for two ratios with probability of 70% considering the average results of previous studies. Based on 90% power to detect a significant difference and α level of 0.05, it was estimated that 120 samples for each series of measurements would be appropriate. Data were presented as means (standard deviation) or percentages, as appropriate. Measurements in the two groups were analyzed with student's t-test for continuous data and chi-square test for categorical analysis. Subgroup analyses were performed to evaluate the possible role of experience of the anesthesia personnel on the ability to inflate the cuff within normal range. Subgroups included attending anesthesiologists, anesthesia residents and technicians considering their years of work experience in anesthesia. All comparisons were two-tailed. Statistical analyses were performed with SPSS software version 16.0 (SPSS, Inc., Chicago, IL, USA).
4. Results
4.1. Cuff Pressures in the Intubated Patients
The mean ETCP after the in vitro survey was significantly lower than the mean ETCP before the intervention (45 ± 13 vs. 51 ± 15 CmH2O, P = 0.002). Before intervention, only 24.2% of ETCPs were within the recommended range, 75% were above and 0.8% were below the limits. After the educational program, the percentage of measurements within safe pressure limits increased to 39.7% (P = 0.002). The remaining ETCPs were more than 35 cm H2O.
4.2. In Vitro Cuff Pressures
Findings from the tracheal model showed that only 36.5% of anesthesia personnel inflated the ETT cuff within safe pressure limits and in 55.8% of trials the pressure cuff was more than 30 cm H2O. Years of experience in anesthesia had no effect on the safe inflation of the ETT pilot balloon in the tracheal model (Table 1). In the next step, six ETT cuffs were filled with different pressures and anesthesia staffs were asked to estimate their pressure by palpation of pilot balloon. The mean estimated pressures of prefilled cuffs are presented in Table 1. Most of the anesthesia staff underestimated the ETCPs. Interestingly, while two out of six cuffs had similar pressures (25 cm H2O), some participants reported different pressure values.
| Anesthesia Personnel | No. | Pressure in the Tracheal Model | Pressure of Prefilled Cuffs, cm H2O | |||||
|---|---|---|---|---|---|---|---|---|
| 65 | 25 | 10 | 50 | 25 | 100 | |||
| Anesthesia resident | ||||||||
| First, y | 6 | 33 (15) | 39 (17) | 31 (11) | 14 (6) | 27 (14) | 16 (6) | 45 (19) |
| Second, y | 14 | 41 (19) | 27 (8) | 21 (6) | 12 (6) | 28 (11) | 16 (5) | 38 (12) |
| Third, y | 8 | 43 (27) | 42 (25) | 28 (15) | 9 (3) | 35 (17) | 20 (13) | 51 (21) |
| Anesthesia technician | ||||||||
| < 2, y experience | 6 | 50 (14) | 25 (4) | 18 (2) | 9 (8) | 23 (3) | 15 (3) | 30 (6) |
| 2-10, y experience | 8 | 36 (8) | 30 (9) | 23 (8) | 13 (7) | 23 (6) | 21 (8) | 33 (8) |
| > 10, y experience | 6 | 31 (12) | 28 (8) | 23 (6) | 17 94) | 28 (4) | 17 (9) | 36 (14) |
| Anesthesiologist | 4 | 33 (8) | 32 (6) | 23 (5) | 8 (4) | 28 (3) | 17 (6) | 42 (15) |
| P Value | 0.47 | 0.14 | 0.21 | 0.15 | 0.50 | 0.82 | 0.11 | |
| Total | 52 | 39 (17) | 32 (13) | 23 (9) | 12 (6) | 28 (11) | 18 (8) | 39 (15) |
5. Discussion
The obtained results of the current study indicate the potential role of education in the safe inflation of ETT cuff. The performance of participants in the study significantly improved after a brief in vitro educational program. However, it did not secure the inflation of ETT cuffs and a considerable proportion of ETCPs fell outside the recommended limits. Simultaneously, the years of experience in anesthesia did not improve the performance of anesthesia team. Altogether, it seems that the importance of maintaining ETCP within safe limits is neglected in the formal education of anesthesia personnel. Members of the anesthesia teams are not reasonably trained to estimate the ETCP when equipment for accurate measurement is not available. Implementing educational programs to introduce estimation techniques besides the use of manometer as a standard intraoperative monitoring will improve the safety of the practice. Similar to earlier reports (11-13, 16), most of the participants underestimated the ETCPs. Trials with the prefilled cuffs indicated that the mean estimated cuff pressures were close to the actual values in ETTs with 10 and 25 cm H2O cuff pressures; while the pressure of hyperinflated cuffs were considerably underestimated. An earlier survey reported that the accuracy of finger palpation method to estimate cuff pressure was 69% for high pressures, 58% for normal pressures, and 73% for low pressures (9). Interestingly, while the second and fifth palpated cuffs had similar pressures (25 cm H2O), the mean reported pressure values for the fifth cuff was lower than that of the second cuff. It is noteworthy that the third and fourth cuffs were filled with higher pressures. It sounds that the fingers of participants may be fooled with the preceding cuff pressures. The other side of the coin is that the fingers of the anesthesia team can be trained and the palpation technique could be more reliable and valid when repeatedly calibrated with the manometer. Several factors including the cuff diameter, thickness, compliance and shape, filling material (air or water in certain surgeries) and head and neck position influence the ETCP (17-21). Some of these factors including ETT type, the ETT to tracheal diameter, geometry of cuff, and filling material influence the tone of the pilot balloon and consequently the reliability of the palpation technique (9). For the purpose of in vitro evaluations, the current study used PVC type ETT with 7.5 ID. This is the most common type and size of ETT in the operating room. It is predictable that the accuracy of palpation technique will be reduced with the use of other types and sizes of ETT and in patients with other than neutral head and neck position. Under such circumstances, accurate measurement of ETCP with manometer is more necessary. Some earlier studies suggested that the experience of the anesthesia staff could improve their safe practice of cuff inflation (14); some others reported the opposite results (15). None of the earlier studies reported whether their study samples ever used the manometer to challenge their palpation-based estimations. It is possible that experienced anesthesia staff in some of these surveys test out their daily technique with accurate manometer measurements. This study was underpowered to evaluate the role of experience of anesthesia personnel in the safe inflation of ETT cuff. In conclusion, authors believe that the best practice is accurate measurement of ETCP with manometer, and palpation technique should be reserved for emergency conditions or whenever manometer is not available. However, members of the anesthesia team should improve their estimation techniques for these certain conditions.