1. Introduction
Chronic donor site pain following autologous iliac crest bone harvest is a common post-operative complication, resulting in significant morbidity and decreased patient satisfaction following many spinal surgeries. The prevalence of post-operative donor site pain has led to multiple treatments aimed at either preventing its development (altered surgical technique, peri-operative local anesthetic infusions to the graft site) or progression (steroid injections, anti-inflammatory medications, opioids, alcohol neurolysis, peripheral nerve stimulation). One of the etiologies of this chronic pain is a trauma to the superior cluneal nerves, which pass over the iliac crest at a distance approximately 7 cm from midline. Due to their relatively superficial location, these nerves are likely to be encountered during a posterior iliac crest bone harvest.
Dysfunction of these nerves can manifest as localized pain over the iliac crest, with or without radiation to the ipsilateral buttock, associated with altered sensation over the upper buttock. While the diagnosis of cluneal nerve-mediated pain can be difficult, especially in the post-fusion patient, Maigne and Doursounian criteria (1) may aid to diagnose: unilateral low back pain referred to the iliac crest and buttock, a trigger point located over the posterior iliac crest 7 cm from the midline, and relief of symptoms with nerve blockade.
The current paper presents a case report of a patient with long-standing, severe pain over the iliac crest donor site six years after lumbar fusion, unresponsive to therapy and oral medications, successfully treated with superior cluneal nerve blocks.
2. Case Presentation
At the time of the patient’s initial presentation to the office, the patient was a 44-year-old male who had long-standing low back following an injury that occurred seven years ago. He had undergone an unsuccessful micro-discectomy in 2005, followed by an L4-5 laminectomy and fusion with right iliac crest bone harvest later that year. His axial low back pain significantly improved following the fusion; however he developed severe pain over the iliac crest donor site, steadily worsening in intensity. He described a sharp, stabbing pain located over the right iliac crest and radiating to the buttock, unchanged by position or activity. There was no radiation of pain into the right lower extremity. He had tried physical therapy, as well as multiple oral medications, with no relief. Physical examination revealed tenderness to palpation over the top of the right iliac crest, just medial and lateral to the vertical donor site scar. Deep palpation over this area reproduced the patient’s typical pain, radiating to the upper buttock. There was some diminished sensation to light touch extending from the crest to the upper and mid buttock region. Plain films and an MRI of the lumbar spine performed in 2009 showed no evidence of hardware failure, recurrent disc herniation, or instability.
The decision was made to follow up with diagnostic, and potentially therapeutic, cluneal nerve blocks.
2.1. Clinical Measures
Patient was clinically evaluated at baseline and every two weeks for several months.
The primary means of evaluation throughout the study were a VAS (2) to assess pain intensity, at baseline and discharge, and a simple dichotomized question (yes/no answer) on quality satisfaction of pain relief achieved. Pain was quantified using a standard 10 cm VAS scale, with the left end marked “0” and “No Pain” and the right end as “10” and “Severe Pain.” Treatment effectiveness was used to measure the patient’s pain relief. Effectiveness at discharge was determined by the proportion of potential improvement achieved with treatment. It was calculated using Equation 1:

According to the formula, the effectiveness is 100% when a patient achieves the maximum scale score (3).
2.2. Procedures
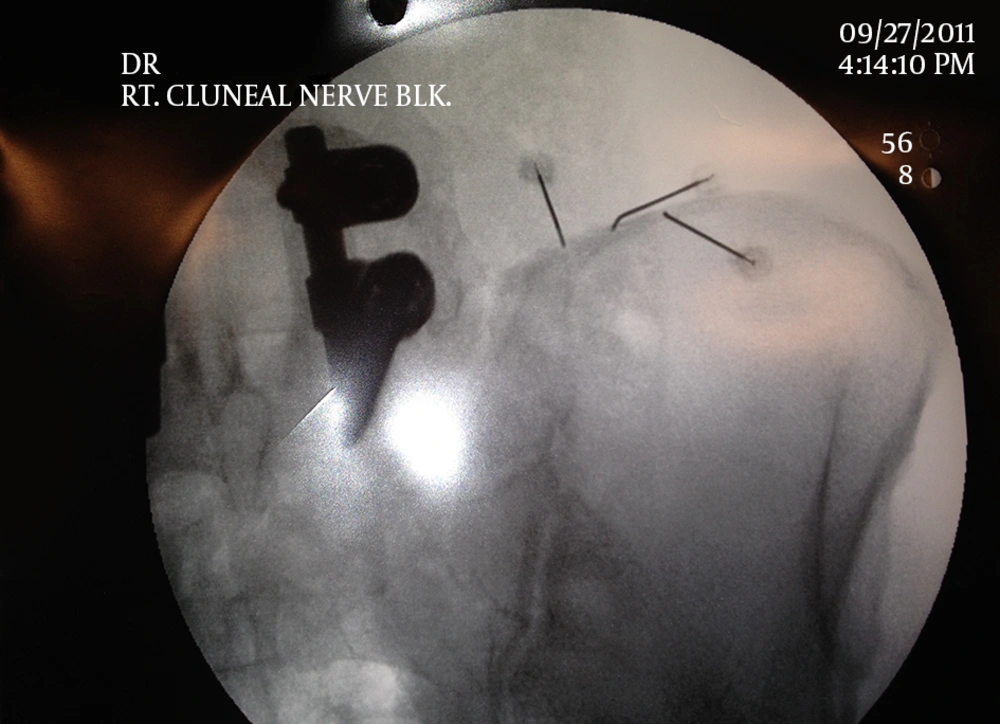
Under fluoroscopy, the right PSIS was identified. The skin overlying the assumed location of the three superior cluneal nerves was marked, at distances of 5 cm, 6.5 cm and 7.3 cm from the PSIS (4-6). After anaesthetizing the skin with 1% lidocaine, a 22 gauge 3.5 cm spinal needle was inserted until contact was made with the iliac crest (Figure 1). It was repeated at each of the three locations, and then a total of 1 mL of kenalog, 1 mL of 1% lidocaine and 1 mL of 0.25% marcaine was injected in divided doses. The needles were withdrawn and no complications were reported during or after the procedure.
Immediately following the procedure, the patient reported more than 80% resolution of his pre-procedural right sided low back pain, with 100% relief of the pain radiating to the buttock. His residual symptoms were localized over his surgical scar. He presented for follow up two weeks later, reporting sustained relief of 50% - 60%. A second set of cluneal nerve blocks, utilizing the same procedure and medications, was then performed.
At follow up seven months out from his second set of cluneal nerve blocks, the patient had sustained an effective pain relief of more than 80% (3). He had no significant recurrence of his pain since the second set of injections.
3. Discussion
Superior cluneal nerve (SCN) dysfunction or entrapment neuropathy is a poorly understood clinical entity that can produce low-back pain and a recent clinical study reported that patients with suspected SCN disorder constitute approximately 10% of the patients suffering from LBP and/or leg symptoms (7).
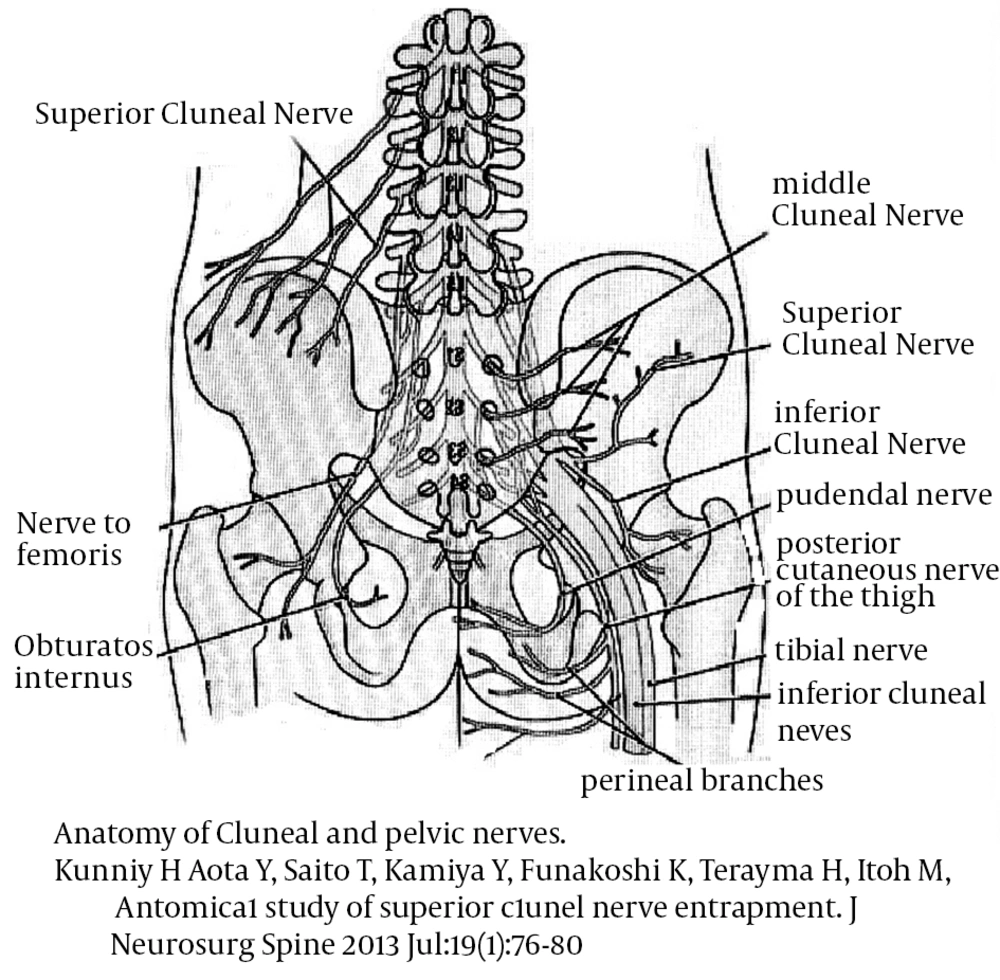
In patients undergoing iliac crest bone harvesting, however, superior cluneal nerve (Figure 2) mediated pain should be considered as one of the most likely etiologies of persistent donor site pain. Blockade of these nerves as they pass over the iliac crest is a technically simple and low-risk procedure that should be offered to patients with chronic donor site pain (6).
Anatomy of Cluneal and Pelvic Nerves (12)
It is known that the most relevant neurological guidelines worldwide do not always recommend nerve blocks to treat entrapment and/or chronic neuropathies but it should also be considered that most of the neurologists are oriented away from procedures and toward non-interventional management at least in part because neurologists do not do interventions and, moreover, it is now widely reported that nerve blocks can be appropriate for patients with radiculopathy that did not experience pain relief after medications, such as NSAIDs (Non-Steroidal Anti-Inflammatory Drugs), gabapentin or opioids. Effective nerve blocks require advanced skills in anatomy Knowledge and imaging techniques because many blocks may be short-lived or useless simply due to imperfect placement of the needles used for the injections and therefore eminent authors still argue against nerve blocks stating that they are often ineffective, whereas others who argued in favor of nerve blocks claim they are just as useful as alternative treatments. The American society of anesthesiologists task force on chronic pain management and the American society of regional anesthesia and pain medicine’s practice guidelines on “chronic pain management” (2010) stated that “peripheral somatic nerve blocks should not be used for long-term treatment of chronic pain (8) and Aetna (9) (Aetna, Inc. is an American managed healthcare company, which sells traditional and consumer directed healthcare insurance plans and related services, such as medical, pharmaceutical, dental, behavioral health, long-term care, and disability plans) consider the use of peripheral nerve blocks (continuous or single-injection) medically necessary to treat acute pain, and chronic pain only as part of an active component of a comprehensive pain management program. In its recent bulletin (8) they recall as “eminent researchers considered nerve blocks evidence insufficient to allow judgement of their effects compared with oral analgesia and that continuous blocks provided less pain compared with single-shot FNB (4 RCTs, 272 participants) at 24 hours at rest and on movement with continuous blocks also demonstrating lower opioid consumption compared with single-shot (8-11).
Performing Superior Cluneal Nerve Blocks, authors always consider that it is often located near the posterior superior iliac spine 13; therefore, it is once again remarked how knowledge of the anatomic locations of these important structures is essential to decrease the complication rate of these procedures (10-12) during which this knowledge may assist to avoid their injury during bone harvest (8, 12). Bone grafted from the iliac crest is often used for maxillofacial and spinal surgeries and chronic donor site pain following autologous iliac crest bone harvest is a commonly encountered complication in the post-operative period, affecting over 30% of the patients at two year follow up (6). There are several proposed etiologies underlying this chronic pain, including trauma to the sacroiliac joint and its overlying ligaments, muscle damage, persistent pain from the periosteum, and dysfunction of/damage to the superior cluneal nerves. In the patient, the iliac crest was previously a common donor site for autologous bone graft due to its accessibility as well as abundance of cortical and cancellous bone. The presenting complaints of the patient, as well as his physical examinations, findings of tenderness over the posterior iliac crest reproducing pain radiating to the ipsilateral buttock with altered sensation over this area led the authors to believe that cluneal nerve dysfunction was the most likely etiology of his persistent donor site pain.
Here is presented a case of persistent donor site pain, more than six years after surgery, successfully treated with two sets of superior cluneal nerve blocks. The patient remains more than 80% improved at seven months follow up. Should his pain return, alternatives for treatment, would include repeating the nerve blocks, or more long-term options such as radiofrequency ablation or alcohol neurolysis of the superior cluneal nerves.