1. Background
Numerous studies demonstrate patients have improved immediate recovery characteristics following desflurane anesthesia compared to other volatile agents, including sevoflurane. There is limited evidence in the literature to suggest that patients undergoing sevoflurane, compared to desflurane anesthesia, may suffer from limitation in function and cognitive ability for an undetermined period of time following surgery (1-3). These differences are not explained pharmacokinetically and may be a result of a direct neurotoxic effect of sevoflurane. An unresolved question is the time required for the ability to return to complex tasks following anesthesia and if any difference exists depending on volatile anesthetic agent used. Commonly, patients are advised not to drive or make important decisions for 24 hours following anesthesia, but this is not well-studied and proscribed on an empiric, rather than scientific, basis with very limited data available (4). This study aims to better define recovery characteristics and characterize the severity and duration of cognitive impairment following sevoflurane or desfluane anesthesia after brief outpatient urologic surgery in elderly females using tests of cognitive ability to objectively testing performance.
2. Objectives
The primary endpoint was time to opening of eyes following discontinuation of volatile anesthetic, i.e. vaporizer shut-off. Secondary endpoints include performance on cognitive tests, time to fitness for discharge from PACU and return to full activity of daily livings (ADL) the following day.
3. Patients and Methods
In this randomized, blinded trial 63 patients were enrolled. Following approval from the institutional review board all patients provided written informed consent. Potential subjects were identified during the clinic visit in the Urology Department and pre-admission testing appointments. Study inclusion criteria consisted of age greater than 65, female subjects scheduled for brief urologic surgery (Cyctoscopy, Ureteral stent, Laser lithotripsy, Ureteroscopy, Vaginal sling, Bladder injury repair, Rectocele repair and Stone extraction), ability to read, write and speak English language. Exclusion criteria consisted of preexisting neurological impairment in thinking process, renal insufficiency or failure, and lack of command of English language. This study is a double blinded randomized controled trial. Patients were randomized to receive either a desflurane or sevoflurane-based anesthetic. The selection of the anesthetic gas (sevoflurane or desflurane) was determined by computer generated randomization. Only the anesthesiology provider had knowledge of which gas had been administered to the subject. The anesthesiology provider was not involved in the data collection. All the investigators and co-investigators who collected the research data were blinded to the gas selection. On the morning of the surgery the study investigator asked the subjects to perform a baseline cognitive task tests to determine the baseline thinking process. A detailed description of the cognitive task is as following:
a) Mini-Mental Status Exam (MMSE): (10-15 minutes). This is a 30-item measure of global cognition (Folstein, Folstein and McHugh, 1975) that tests orientation to time and place, object naming, repetition, attention, recall, and following complex commands.
b) Trail Making Test Part A and Part B: Part A (3 minutes) of this measure (Army Individual Test Battery, 1944; Reitan and Wolfson, 1985) is a test of visual attention where the subjects must draw lines on a page connecting 25 consecutive numbers as quickly as possible. Part B (5 minutes) requires the subject to alternately sequence numbers and letters randomly distributed on a page into their ascending and alphabetical order as quickly as possible.
c) Digit Symbol Coding: (2 minutes). This subtest of the WAIS-III (Wechsler, 1997) consists of nine digit-symbol pairs followed by a list of digits. Under each digit the subject must write down the corresponding symbol as quickly as possible.
d) Hopkins Verbal Learning Test-Revised (HVLT-R): (8 minutes) Memory for verbal information will be assessed with this list learning task assessing immediate and delayed recall.
e) Stroop Color and Word Test: (5 minutes). This test (Stroop, 1935; Golden, 2002) measures cognitive control by asking subjects to suppress a habitual response in favor of an alternate response. Participants are shown a word and asked to name the color in which the word is written.
Total time expected for cognitive task tests is 28-33 min. After testing, the subjects underwent their planned procedure. The selection of the anesthetic gas was determined by a computer generated randomization list. The investigators and the subjects were blinded to the anesthetic gas given. At the conclusion of the surgery, the anesthetic gas was discontinued and the time to eye opening after cessation of the gas was documented. At 30 minutes and 2 hours after discontinuation of the anesthetic gas, the subjects were asked to repeat the same sets of cognitive task tests. On post-operative day 1 the co-investigator had telephone conversation with the subjects who were discharged home after surgery. Modified Telephone Interview for Cognitive Status (TICS-M) and Memory Aging Telephone Screen (MATS) were used to collect data (10 minutes). TICS-M is a 13-item telephone interview (Welsh, Breitner, and Magruder-Habib, 1993) for late-life cognitive assessment that includes tests of orientation, attention, working memory, praxis, sentence repetition, naming to verbal description, recent memory, word opposites, and an additional immediate and delayed recall of a 10-word list. MATS consists of a subjective cognitive complaints questionnaire on subjects' perceived cognitive decline and 10 cognitive items assessing verbal memory (Rabin et al., 2007). The subjects’ participation concluded after follow-up telephone conversation. On arrival in the OR, a peripheral IV was placed and patients received metoclopramide 10 mg, fentanyl 50 ug and propofol 2 mg/kg. Patients were randomly assigned to receive either desflurane or sevoflurane, breathing spontaneously via laryngeal mask airway, with end-tidal concentration recorded every 5 minutes. Concentration was initially set to 6 volume% for desflurane and 2 volume% for sevoflurane in oxygen. Before the conclusion of surgery, patients received 4 mg of ondansetron, IV and 30 mg of ketorolac, IV. At the conclusion of the surgery, identified as completion of last skin suture, volatile anesthetic discontinuation occurred and a blinded observer entered the operating room to record time to eye opening when prompted by the anesthesia practitioner every 10 seconds. Removal of the LMA preceded patient transport to the PACU while monitoring by the same blinded observer continued. Cognitive testing at the specified time intervals occurred in PACU. Testing and data were subsequently collected before hospital discharge and in the surgeon’s office the following day. In the PACU patients received 12.5 to 25 ug fentanyl, as necessary for breakthrough pain.
3.1. Statistical Methods
This study was powered off of Mahmoud et al. with a sample size of (n = 60) and with the primary endpoint being time to opening of eyes following discontinuation of volatile anesthetic (1). The data was analyzed using Student’s t-test for patient characteristics and Mann-Whitney for nonparametric data. This is similar to the anesthetic technique and data analysis in Mahmoud et al. (1) A sample size of 30 subjects in each treatment group provided at least 80% power to detect a difference of 4 minutes in time to eye opening, assuming a standard deviation of 5.0 minutes (α = 0.05, 2-tailed). The detectable difference in time to eye opening of 4 minutes is taken from the Mahmoud et al. (1) where 16-75 year old females scheduled for minor day-case gynecological procedure (2.8 minutes for desflurane, 7.0 minutes for isoflurane). The standard deviation estimate of 5 minutes is a conservative estimation, which is based on the quoted observed range of time to eye opening (1 to 12 minutes) in Mahmoud et al. Additionally, this conservative estimation of the standard deviation was selected to reflect the older population in this study as that compared to Mahmoud et al. (1).
3.2. Statistical Analysis
Data entry and analysis was performed with SPSS (version: 20.0, SPSS Inc, Chicago, USA). Demographic and patient characteristics were obtained for all enrolled subjects. Mean ± SD were obtained for age, time to open eyes, and time to discharge from PACU. Number of observations and percentages were obtained for ethnicity, marital status, education level and medical history (physical disability, cognitive disability, visual difficulties, assistance with Activities of Daily Living (ADL), neurological disorders, traumatic brain injury, psychiatric disorders, and depression/anxiety). Median and range were obtained for time to eye opening, time to discharge from PACU and scores from neurocognitive test battery. Comparison between the study groups for anesthesia recovery time and scores of 24-hours follow-up tests were done by performing Mann Whitney U Test. The differences in scores of pre and post-surgery neurocognitive tests were compared by performing Wilcoxon Signed Rank test. Statistical significance was set at 0.05 and test statistics, effect size and P values were reported.
4. Results
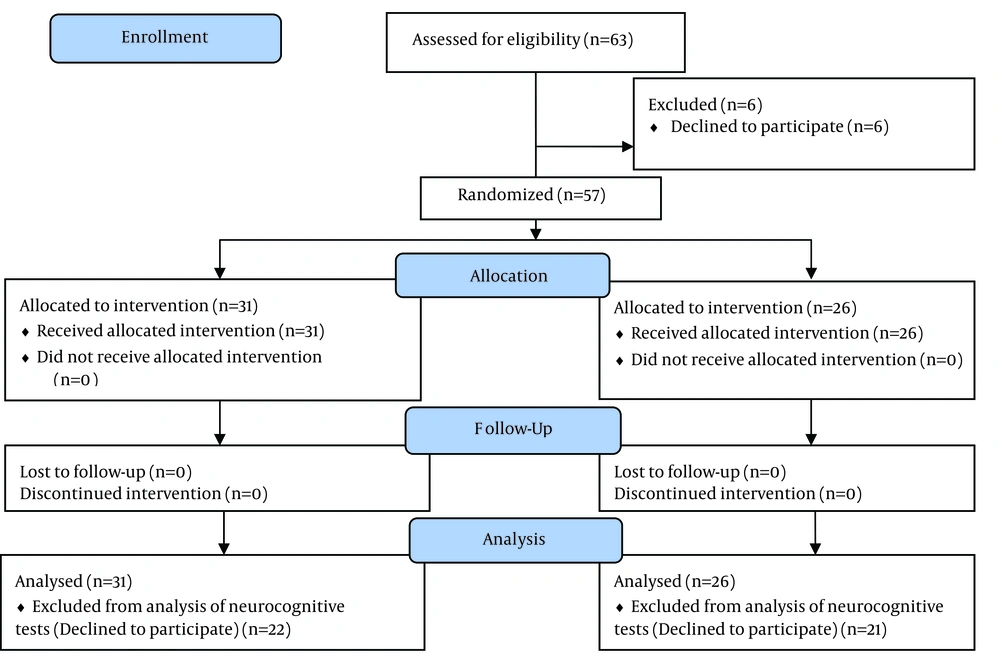
A total of 63 subjects were enrolled and randomized into two groups, 31 subjects in desflurane Group and 32 in sevoflurane Group. Six patients were not included due to cancelation or postponement of surgery or changes in the anesthesia care plan. The remaining 57 subjects were enrolled and 51 subjects agreed to complete a study questionnaire (background information and impairments) and participate in neurocognitive testing. A total of 15 subjects managed to complete at least one test from the test battery at either pre-surgery, 30-minutes post-surgery, 2-hours post-surgery or 24 hours follow-up tests. Only one subject was able to complete all the tests in the battery at all the designated times (Figure 1) Demographic and patient characteristics are presented in Table 1. Anesthesia recovery time was recorded for all enrolled subjects, mean ± SD of time to eye opening and time to discharge from PACU (Aldrete > 9) are presented in Table 2. Comparisons of anesthesia recovery time and 24-hours follow-up neurocognitive test scores were presented in Table 3. Time to eye opening and time to discharge from PACU were slightly faster in subjects who were randomized into desflurane group. These differences did not reach statistical significance. Scores of neurocognitive tests performed at pre and post-surgery are presented in Table 4 (desflurane group) and Table 5 (sevoflurane group). Subjects in desflurane group performed slightly better than the subjects in sevoflurane group in most of the neurocognitive tests. Comparison of these scores showed no statistically significant differences between the study groups. A statistically significant difference was seen in comparison of pre-surgery and post-surgery scores of Trail Making Test Part B. This difference was only seen in the desflurane group. However, the scores for this test and all the other tests were within average score range for elderly females without cognitive impairment. No other statistically significant differences were seen between pre and post-surgery scores for both study groups.
| Desflurane Patients | Sevoflurane Patients | |
|---|---|---|
| Age, y | 68.2 ± 6.43 | 67.1 ± 6.11 |
| Ethnicity | ||
| Caucasian | 13 (14.9) | 12 (37.5) |
| Black | 14 (45.2) | 15 (46.9) |
| Hispanic | 4 (12.9) | 5 (15.6) |
| Marital Status | ||
| Married | 13 (48.1) | 3 (12.0) |
| Single | 4 (14.8) | 15 (60.0) |
| Widow | 5 (18.5) | 6 (24.0) |
| Divorced | 4 (15.4) | 1 (4.0) |
| Education level | ||
| Grade School | 3 (11.5) | 3 (12.0) |
| High School | 16 (61.5) | 15 (60.0) |
| College | 7 (26.9) | 6 (24.0) |
| Post-graduate | 0 | 1 (4.0) |
| Physical disability | 0 | 3 (12.0) |
| Cognitive Disability | 1 (3.8) | 0 |
| Visual Difficulties | 11 (42.3) | 12 (48.0) |
| Assistance with ADL | 0 | 2 (8.0) |
| Neurological Disorder | 1 (3.8) | 2 (8.0) |
| Traumatic brain injury | 0 | 1 (4.0) |
| Psychiatric Disorder | 2 (7.7) | 1 (4.0) |
| Depression/Anxiety | 3 (11.5) | 2 (14.3) |
Demographic and Patient Characteristics of Study Population (n = 63) a
| Desflurane Patients | Sevoflurane Patients | U Value | Z Value | r Value | P Value | |||
|---|---|---|---|---|---|---|---|---|
| No. (%) | Median (Range) | No. (%) | Median (Range) | |||||
| Time to eye opening, sec | 31 (100) | 340 (60-1440) | 26 (100) | 395 (60-1080) | 322 | -1.30 | 0.2 | 0.194 |
| Time to discharge from PACU, min | 31 (100) | 85 (40-180) | 26 (100) | 109.5 (33-247) | 366.5 | -0.59 | 0.1 | 0.558 |
| TICS-M Total Score, ( /39) | 8 (25.8) | 25 (15-33) | 6 (23.1) | 20 (10-30) | 15 | -1.16 | 0.3 | 0.244 |
| MATS Total Score of memory complaints, ( /12) | 8 (25.8) | 3.5 (0-7) | 6 (23.1) | 6 (0-8) | 15 | -1.17 | 0.3 | 0.241 |
Comparison Between Study Groups
| Pre Surgery | 30 min Post Surgery | 2 hours Post-Surgery | Z Value | r Value | P Value | ||||
|---|---|---|---|---|---|---|---|---|---|
| No. (%) | Median (Range) | No. (%) | Median (Range) | NO. (%) | Median (Range) | ||||
| HVLT | |||||||||
| (Delayed recall score/ highest recall score, %) | 8 (25.8) | 85 (57-160) | 2 (6.5) | 82 (50-113) | 5 (16.1) | 63 (0-70) | -1.07 | 0.3 | 0.285 |
| MMSE | |||||||||
| Total score, (/30) | 9 (29.0) | 29 (23-30) | 2 (6.5) | 29 (27-30) | 6 (19.4) | 30 (20-30) | 0 | - | - |
| Trail making part A | |||||||||
| Total time, sec | 9 (29.0) | 40 (24-65) | 2 (6.5) | 39 (38-40) | 6 (19.4) | 40 (30-60) | -0.67 | 0.2 | 0.500 |
| Trail making part B | |||||||||
| Total time, sec | 8 (25.8) | 74 (42-155) | 2 (6.5) | 88 (66-110) | 6 (19.4) | 103 (60-175) | -2.02 | 0.6 | 0.043 |
| Stroop color and word Test | |||||||||
| Interference ratio (color word score/ color score) in 45 seconds | 8 (25.8) | 0.5 (0.51-0.80) | 2 (6.5) | 0.4 (0.36-0.43) | 5 (16.1) | 0.4 (0.32-0.80) | -0.73 | 0.2 | 0.465 |
| Digit symbol coding | |||||||||
| Score in 90 seconds | 4 (12.9) | 23 (19-32) | 2 (6.5) | 33 (18-48) | 5 (16.1) | 35 (21-37) | -1.34 | 0.4 | 0.180 |
Comparison of Pre and Post-Surgery Test Scores in Desflurane Group (n = 31) a
| Pre Surgery | 30 mins Post Surgery | 2 hours Post-Surgery | Z Value | r Value | P Value | ||||
|---|---|---|---|---|---|---|---|---|---|
| No. (%) | Median (Range) | No. (%) | Median (Range) | NO. (%) | Median (Range) | ||||
| HVLT | |||||||||
| (Delayed recall score/ highest recall score, %) | 4 (15.4) | 38 (0-40) | 0 | - | 2 (7.7) | 25 (0-50) | -0.45 | 0.2 | 0.655 |
| MMSE | |||||||||
| Total score, (/30) | 6 (23.1) | 28 (20-30) | 0 | - | 3 (11.5) | 29 (21-30) | -0.45 | 0.2 | 0.655 |
| Trail making part A | |||||||||
| Total time, sec | 6 (23.1) | 54 (27-113) | 0 | - | 2 (7.7) | 47 (42-52) | -1.34 | 0.5 | 0.180 |
| Trail making part B | |||||||||
| Total time, sec | 6 (23.1) | 112 (38-188) | 0 | - | 2 (7.7) | 96 (90-101) | -0.45 | 0.2 | 0.665 |
| Stroop color and word test | |||||||||
| Interference ratio (Color Word Score/ Color Score) in 45 seconds | 5 (19.2) | 0.4 (0.36-0.59) | 0 | - | 2 (7.7) | 0.3 (0.04-0.45) | -1.34 | 0.5 | 0.180 |
| Digit symbol coding | |||||||||
| Score in 90 seconds | 6 (23.1) | 27 (12-40) | 0 | - | 2 (7.7) | 35 (34-36) | -1.34 | 0.5 | 0.180 |
Comparison of Pre and Post-Surgery Test Scores in Sevoflurane Group (n = 26) a
5. Discussion
This study questioned the difference between volatile anesthetic agent’s effects on patients completing a battery of neurocognitive tests attempting to answer the question if one agent has a more profound effect verse the other. These tests were completed both immediately following surgery and on postoperative day 1. Our results did not reach statistical difference. This included the testing done the following day, TICS-M and MATS. While these cognitive tests have been proven to be reliable and valid screening tools for dementia, question still remain regarding use in anesthetized patients. Of note, in the desflurane group, the trail making part B (TMP-B) test result in seconds did prove to be longer versus pre-surgery testing. TMP-B is a well validated test to differentiate between normal and pathological aging (5). TMP-B requires cognitive flexibility, working memory, set-shifting abilities, the ability to maintain two response sets as well as inhibitory functions (5). This specific test focuses on not just cognitive processing speed but also considers attention switching difficulties (6). No difference was seen in the pre and post-operative values in the sevoflurane group. This is a very common tool used to assess cognitive fitness to drive in people with possible dementia (7) and as a critical piece in an assessment of executive function in neurodegenerative disorders (5). More study is needed to assess if desflurane has a greater impact on the neurocognitive test TMP-B than sevoflurane. The significance of this finding, effect on driving or executive function, remains to be answered. This study has several limitations which centers on the case type and setting in which the surgery took place. Short procedure or same day surgery units are inherently dependent on both rapid room turn over and short post anesthesia care unity time stays. This precluded neurocognitive testing completion. Because of this, while the study design was novel and provides what could be a good framework for future studies, the final results lacked power to show the statistical significance proving or disproving our hypothesis. However; several key inferences can be made. There was no statistical difference in time from vaporizer shut off to eye opening between the two groups. This is contradictory to previously reported findings (1, 8). The data was trending, but no real definitive conclusion can be made due to lack of statistical significance. Our findings are consistent with previously published reports which show no difference in time to discharge from the post-operative care unit (3, 8-11). Postoperative cognitive dysfunction (POCD) will continue to become more of a concern as the average lifespan continues to lengthen. POCD, while classically associated with cardiac surgery, is present in 30-40% of all adult patients regardless of age (12, 13). In patients over 60 years old it can persist for up to 3 months (14). This was not shown to be associated with length or procedure or anesthetic type (15-17). Instead, inflammation caused by the stress of surgery was implicated as the cause of cognitive decline (18, 19). Volatile agents themselves have been implicated as causative factors in cognitive decline but no difference in incidence was seen between sevoflurane and desflurane (20-23). Our study shows no statistically significant cognitive decline in any testing group except for those in the trail making part B desflurane group. This conclusion is limited by the inherent limitations of the study, but does reinforce the theory that the systemic inflammatory response from the surgery causes POCD (18, 19). Our patient population underwent same day urology procedures which cause minimal systemic inflammation and therefore would cause minimal POCD regardless of volatile anesthetic choice. Further study is needed to define impact.