1. Background
Recently, rhinoplasty (septorhinoplasty) is one of the most common cosmetic surgeries, with an increasing demand and bleeding is one of the common complications, during this surgery (1). Besides causing problems in surgeon's vision and disturbance during the surgery, bleeding in the field also induces discomfort for the patient, during surgery with local anesthesia by sedation, and even causes hematoma and dissatisfaction for both patient and surgeon (2). In order to reduce intraoperative bleeding, various techniques are used, which include maintaining patents' head in upwards position, cold compression, creating controlled hypotension during operation, as well as prescribing topical vasoconstrictor and antifibrinolytic factors (2-4). Effective factors for reducing bleeding in the surgical field include systemic blood pressure (BP), patient's heart rate (HR), and coagulation status, which must be controlled from the beginning, to reduce the amount of bleeding. For the adequate control of BP and HR during operations, it is required to prevent sudden changes in these factors, from the beginning; i.e. the factors that stimulate the sympathetic system and release of neurotransmitters, catecholamines and increase the BP and HR (4, 5). One of these factors is direct laryngoscopy that induces the pressor response and sympathetic stimulation. Therefore, by inhabiting the hemodynamic changes induced by direct laryngoscopy and tracheal intubation, it is possible to have a better control over patients' hemodynamic responses during surgery and, therefore, besides reducing the amount of intraoperative bleeding, it also provides a more appropriate condition for surgery.
Gabapentin is the structural analog for the neurotransmitter of gamma-amino butyric acid (GABA) and an anticonvulsant drug, which is also effective for treating neuropathic pain. The peak effect occurs within 4 - 6 hours (6, 7). This drug is not metabolized in humans, does not establish bonds with plasma proteins and is excreted through urine, without any changes. Gabapentin is well tolerated by the patients, with low rate of complications, such as somnolence (15%), dizziness (11%), asthenia (6%), headache (4.8%), and nausea (3.2%). A study conducted in 2012, in the USA, showed that gabapentin reduced the release of catecholamine from adrenal chromafin cells (7). In recent investigations, several pieces of evidence have been obtained, which imply that premedication with gabapentin may be effective for providing postoperative analgesia, reducing anxiety before surgery, maintaining hemodynamic stability during direct laryngoscopy and tracheal intubation and reducing postoperative chronic pain, vomiting, as well as delirium (6, 8-10). This drug inhibits voltage-dependent membrane calcium channels, which may act as a calcium channel blocker (11), that may trigger decreases in BP.
2. Objectives
This study aimed to examine the effects of oral gabapentin on hemodynamic changes during direct laryngoscopy and the amount of bleeding in the patients undergoing septorhinoplasty.
3. Patients and Methods
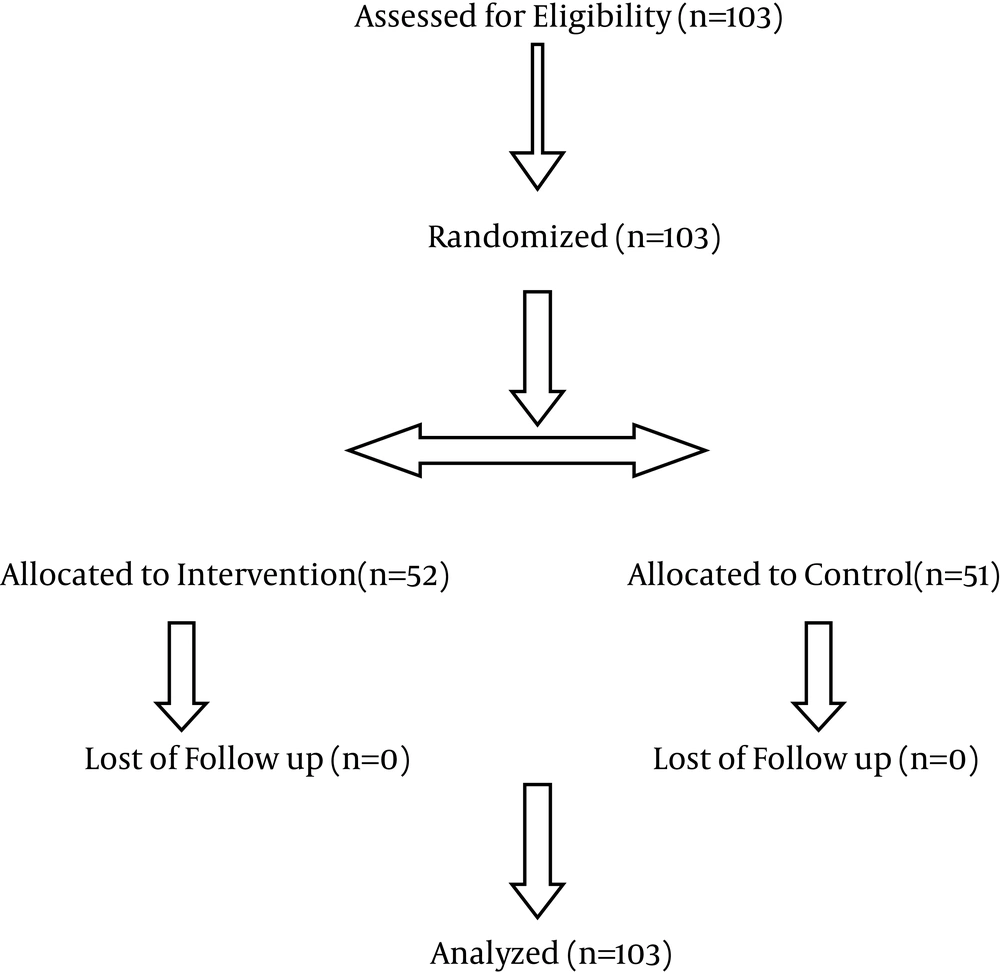
After approval of the research proposal by The Vice Chancellor for Research and Technology and ethics committee of Guilan university of medical sciences, Rasht, Iran, and registration in the Iranian registry of clinical trials (IRCT201409288677N3), this study was conducted as a prospective, clinical randomized double-blind trial, on 103 patients aged 18 - 45 years, with American Society of Anesthesiologists (ASA) class I‒II, who were hospitalized during 2014, for septorhinoplasty operation in Amir-al-Momenin academic hospital, Rasht, Iran. The stages of the study were explained to all the participants and the written informed consent was collected from the patients, after they agreed to enter the research (Figure 1).

S1 = 6.6, S2 = 7.3, α = 0.05, β = 0.1, d = 3 (12). N = 50 (N = 100).
The subjects with hypertension, morbid obesity, difficult intubation (Mallampatti Grade 3, 4), diabetes mellitus, cardiac disease or severe hepatic/renal dysfunction and those with medical history of dizziness and frequent headaches, or who were receiving sedative and anticonvulsant drugs, were not included in this study. Before surgery, the patients’ laboratory parameters was evaluated, including complete blood count, renal function (blood urea nitrogen, creatinine) and coagulation tests (prothrombin time, partial thromboplastin time, international normalized ratio). All of the participants kept on fasting for 8 hours. The patients were classified into two groups, gabapentin (G) or placebo (P), using random fixed block method. Patients in gabapentin group received 900 mg gabapentin orally [three 300 mg capsules (Daru Co., Tehran, Iran)], 2 hours before being transferred to the operating room (6). Patients in placebo group received three placebo capsules orally, 2 hours before the surgery. After entering the operating room, the patients underwent the standard monitoring, including lead II electrocardiography, pulse oximetry, noninvasive BP and capnograph (Aria, Saadat, Tehran, Iran). Baseline values of (HR, systolic BP (SBP), diastolic BP (DBP), mean arterial blood pressure (MAP), and percentage of arterial oxygen saturation (SpO2) were recorded. The anesthetic technique was similar for all the patients, with 2 μg/kg fentanyl, 20 - 40 mg lidocaine, 2 - 2.5 mg/kg propofol and 0.5 mg/kg atracurium and, after the tracheal intubation, anesthesia was preserved by total intravenous anesthesia (50 μg/kg/minutes propofol and 0.1 μg/kg/minutes remifentanil) and oxygen and N2O, with 50% ratio. Then, the patients were kept under the controlled ventilation (tidal volume = 8 - 10 cc/kg, respiratory rate = 10/minute, inspiration to expiration ratio = 1:2). Patients’ systemic BP was preserved in the range of 85 - 90 mm/Hg for SBP, and, for maintaining these values, we used beta blockers and small doses of remifentanil (3). The HR, SBP, DBP, MAP, and SpO2 were measured and recorded, before induction of anesthesia and 3, 5, 10, and 15 minutes after the intubation, after tracheal extubation and in post-anesthesia care unit. The amount of intraoperative bleeding was measured, based on the amount of blood present in the suction line, minus the washing serum and the blood gauze counting (mL) was also measured. Patients with surgery lasting longer than 2 hours were excluded from study. In the recovery period, the postoperative nausea, vomiting, and pain were recorded for each individual based on the 10-score visual analog scale VAS. Nausea and vomiting were treated with 0.1 mg/kg intravenous ondansetron and VAS > 3 points with 0.5 mg/kg intravenous pethidine. Finally, the collected data were analyzed by SPSS (v. 16) software (SPSS Inc., Chicago, IL, USA).
4. Results
The present study was conducted on 103 candidate patients for septorhinoplasty operation, in Amir-al-Momenin academic hospital, in 2014. The patients were randomly allocated into two groups, namely the group receiving oral gabapentin (52 subjects) and the placebo group (51 subjects). Afterwards, the amount of bleeding and hemodynamic changes during the operation were examined (before induction of anesthesia; 3, 5, 10, 15 minutes after the intubation, and after the tracheal extubation).
In perusing the patients, in terms of the distribution of frequency and gender for the two groups, i.e. gabapentin and placebo groups, by using Chi-square test and t-test, there was no statistically significant relationship between two groups (Table 1).
| Group | Recipient of Gabapentin | Recipient of Placebo | Total |
|---|---|---|---|
| Age, y | |||
| < 20 | 5 (9.6) | 14 (27.5) | 19 (18.4) |
| 21 - 30 | 32 (61.5) | 24 (47.1) | 56 (54.4) |
| > 30 | 15 (28.8) | 13 (25.5) | 28 (27.2) |
| Total | 52 (100) | 51 (100) | 103 (100) |
| Mean ± SD | 28.17 ± 6.8 | 25.96 ± 7.96 | 27.08 ± 7.32 |
| Gender | |||
| Male | 11 (21.2) | 4 (7.8) | 15 (14.6) |
| Female | 41 (78.8) | 47 (92.2) | 88 (85.4) |
| Total | 52 (100) | 51 (100) | 103 (100) |
a The values are presented as No. (%).
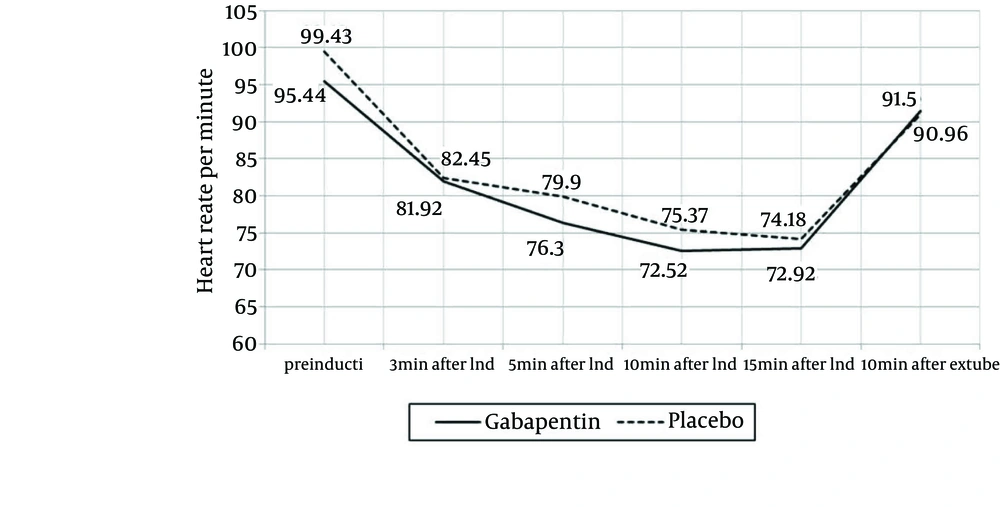
When comparing both groups, in terms of changes in the HR, during the desired time periods, no statistically significant difference was found (P = 0.43; F = 0.9), using Analysis of Variance with repeated measurements (Figure 2).
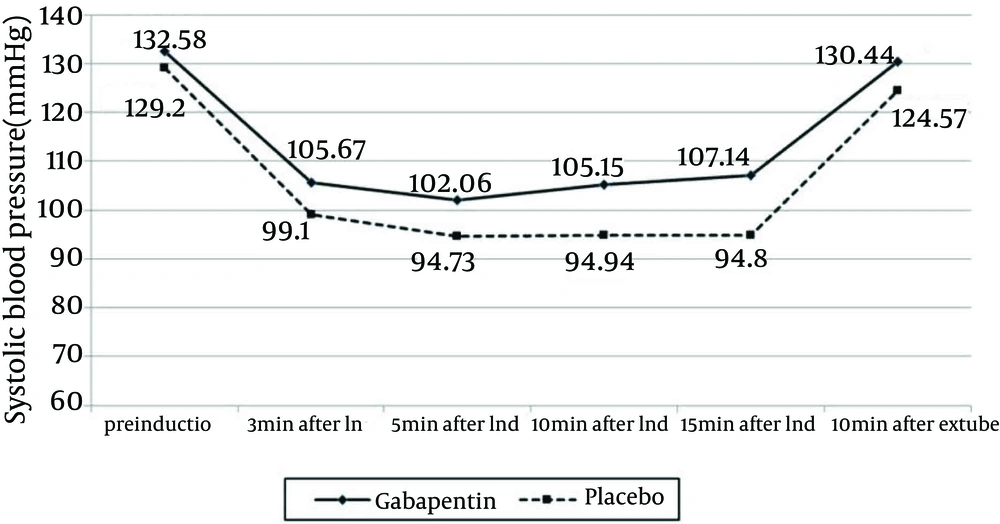
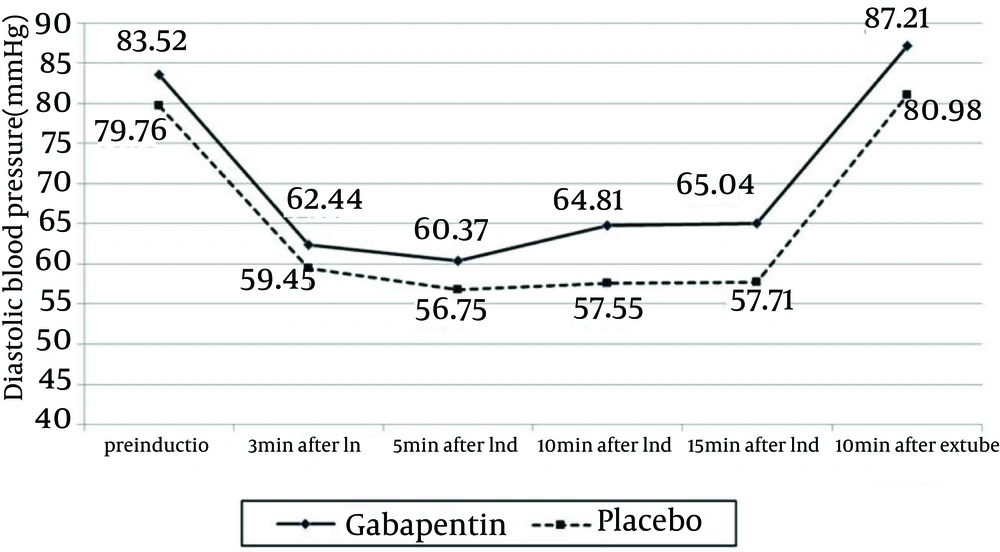
In addition, the change trend of the SBP in each group showed a statistically significant difference (gabapentin group: P < 0.0001, F = 86.2 and placebo group: P < 0.0001, F = 160.9) and the difference was also significant between the two groups (P = 0.034, F = 2.61); however, the comparison of the changes in DBP demonstrated no significant difference (P = 0.337, F = 1.14) (Figures 3 and 4).
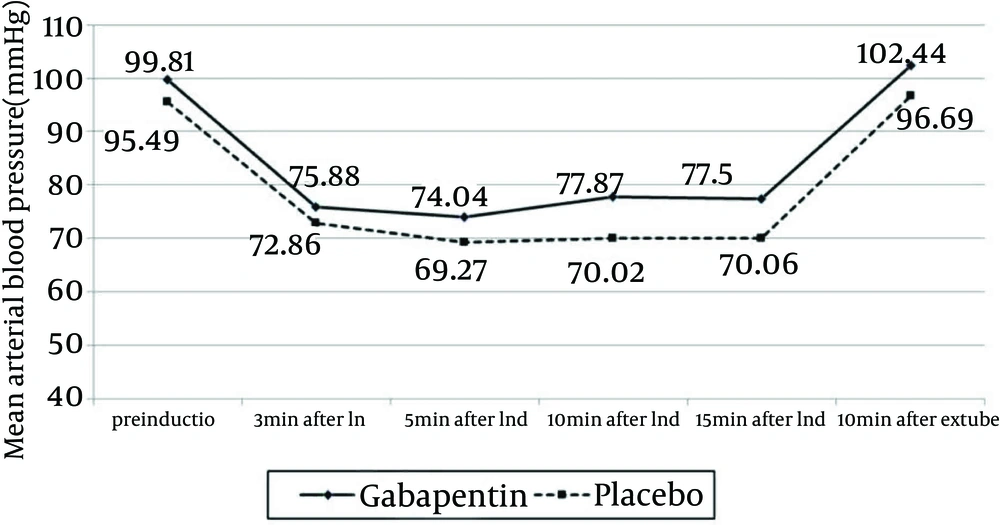
Comparing the trend of changes in MAP and SpO2 showed no statistically significant difference in the MAP and mean arterial oxygen saturation in both groups (P = 0.364, P = 0.364) (Figure 5).
Average bleeding volume was lower in the gabapentin (85.77 ± 64.35 ml) compared with placebo (91.37 ± 59.06 mL) groups (P > 0.05). Regarding nausea, vomiting, and other complications, such as shivering and digestive problems, there was no statistically significant difference between the two groups. When comparing the patients' pain by VAS, no statistically significant difference was observed between the two groups using Mann-Whitney Uf test. The VAS average value for groups G and P was equal to 2.5 ± 2.11 and 2.55 ± 1.74, respectively (P = 0.55) and, regarding the frequency distribution of receiving pethidine after the surgery (P = 0.88) and the amount of received pethidine (mg) (P = 0.42), there was no statistically significant difference between the two groups.
5. Discussion
In this double blinded randomized clinical trial, the effect of 900 mg oral gabapentin on cardiovascular responses to direct laryngoscopy and tracheal intubation and the amount of intraoperative bleeding were compared with the placebo, 2 hours before the surgery. Results of the study showed no statistically significant difference in bleeding between both groups and, in terms of changes in HR, DBP, MAP, and SaO2 in specified time intervals between the two groups. Regarding the average amount of bleeding, although there was clinically lower amount of bleeding in the gabapentin group, the difference was not statistically significant. With comparing the changes of systolic blood pressure between groups during the time intervals, SBP was more in intervention group, although the trend of changes in the SBP in each group showed a statistically significant difference.
Memis et al. showed that the prescription of 800 mg gabapentin within 1 hour before the surgery could blunt the cardiovascular responses, such as BP and HR, within the first 10 minutes after the tracheal intubation (8). Although, in the present study, changes in the BP (SBP, DBP) and HR demonstrated a statistically significant difference within each group (P < 0.0001), variations in SPB were significantly different between the two groups (P = 0.034). We could not find any reason for the higher SBP in the gabapentin group.
In the study on 60 patients, Neogi et al. prescribed gabapentin premedication during the laparoscopic cholecystectomy and found that MAP, average HR after the intubation, and pneumoperitoneum were significantly lower than in the control group and also, more stable during the operation (12). In the present study, changes in SBP were significantly different between the two groups (SBP was higher in intervention group). However, no significant difference was observed among other hemodynamic variables even though HR was lower in the gabapentin group.
In another study by Montazeri et al. on 96 patients, who received 800 mg gabapentin 90 minutes before the elective operation, there was a less significant change in HR, SBP, DBP, and MAP at 3, 5, 10, and 15 minutes after the laryngoscopy (9). However, in the present study, although the mean HR at each of the studied time was lower in the gabapentin group, there was no significant difference between the two groups. The trend of changes in SBP and DBP was significantly different within each group (P < 0.0001). However, when the two groups, SBP was lower in the placebo group (P = 0.034).
In the study in 2006, Fassoulaki et al. examined the effect of gabapentin (1600 mg, in four doses from 24 hour before the operation) on pressure responses to the laryngoscopy and tracheal intubation, in 46 candidate patients for hysterectomy, because of the benign disease. In this research, the SBP and DBP after the intubation and in the first 10 minutes were lower in the gabapentin group than the placebo group (P < 0.004). However, no effect was observed on the HR and no patient had a severe drop in the BP (13). However, in the present study, no statistically significant difference was found between the two groups, and even SBP was higher, which might be the consequence of the lower dosage and shorter duration of the drug intervention.
In another study, this time from 2011, by Misra et al. the effect of gabapentin premedication (900 mg, 2 hours before the operation) was studied in the candidate patients for craniotomy and the hemodynamic responses to implanting a pin in the patients were examined. It was finally found that the patients receiving gabapentin had lower SBP and MAP. However, their HR was variable (14). In the current study, hemodynamic changes in response to the laryngoscopy were examined; although there was a significant reduction in each group, there was no significant difference between the two groups. Nevertheless, SBP was higher in the gabapentin group.
In another study, in 2011, Bafna et al. compared the effect of different doses of gabapentin for reducing hemodynamic response to the laryngoscopy and tracheal intubation in the patients with normal arterial BP. They divided the patients into three groups, each with 30 subjects. The first group received 600 mg gabapentin, the second group received 1000 mg gabapentin, while the third group was the placebo group. The MAP and HR were higher in the placebo and 600 mg gabapentin groups than in the 1000 mg gabapentin group (15). In the present study, there was no significant clinical difference between the two groups. However, the amount of intraoperative bleeding was lower in the gabapentin group, which was not examined in the above-mentioned study.
In the present study, a significant decrease in the hemodynamic variables was observed in both groups; however, it was not significant between the two groups, which might be due to the use of propofol during the induction of anesthesia and prescription of propofol infusion and remifentanil, during the anesthesia. The SBP was higher in intervention group and we were unable to find any reason for this event, which can be regarded as a limitation of this study. In fact, the mechanism of decrease in the blood pressure by gabapentin following laryngoscopy and intubation was not determined. This drug inhibits voltage-dependent membrane calcium channels and may act as a calcium channel blocker (12), which may be decreased BP.
The current study emphasized the observation that a decrease in the amount of bleeding was observed in the gabapentin group (non-statistically significant), which has not been examined in the previous studies. The present study showed that premedication with 900 mg gabapentin did not affect the hemodynamic changes induced by laryngoscopy and the amount of bleeding. However, the decreased amount of bleeding was observed in the gabapentin group, although this decrease was not statistically significant in the above-mentioned variables.
In sum, it seems reasonable to consider that a larger study group could be useful to evaluate the effect of premedication by oral gabapentin on hemodynamic variables and surgical field.