1. Background
During anesthesia, continuous body temperature monitoring is essential, because of the most common risk of perioperative hypothermia, caused by inhibition of thermoregulation during anesthesia, as well as patients’ exposure to a cool environment. Monitoring is also required to detect malignant hyperthermia (1-3). General anesthesia causes a shunt to move from core to peripheral level and this decreases the difference between core and peripheral temperatures. Such a difference remains constant, after reaching the anesthetic steady condition, which lasts for around 10 - 15 min from the start of anesthesia (4). Anesthetic-induced impairment of normal thermoregulatory control and the resulting core-to-peripheral redistribution of body heat represent the primary cause of hypothermia, in most patients (5). Hypothermia, in children, is defined as a lower than 36°C core body temperature (6), which results in increased morbidity and mortality (7). Risk of hypothermia increases with general anesthesia, leading to severe symptoms, in children. During hypothermia, the basal metabolism of the body decreases by up to 30% (8), while vasoconstriction of the skin is impaired (9). The combination of increased sweating thresholds and reduced vasoconstriction increases the inter threshold range ten-fold, from its normal value of 0.2 - 0.4°C to approximately 2 - 4°C. Temperatures, within this range, do not trigger thermoregulatory defense mechanisms. Therefore, by definition, patients are poikilothermic within this temperature range (5). Surgery can also cause loss of body temperature by three to four times (10). Hypothermia can occur in patients who undergo major surgeries, by up to 20%, which is also accompanied by various symptoms that can increase the clinical consequences of patients, especially high-risk patients (11). These consequences include respiratory disorders (12), apnea (13), hypoxia, carbon dioxide retention, metabolic acidosis, hypoglycemia, left shift of oxygenation curve, heart disorders, platelet dysfunction, dysfunction of coagulation enzymes, increased bleeding, increased transfusion requirements (14), increased lesion infection, change in drug metabolism (15) and thermal discomfort (16). A more severe loss of temperature, inability to generate heat inside the body and lack of thermoregulatory response, in children, make them more susceptible to hypothermia than adults (13). Therefore, correct and continuous measurement of the core body temperature, during surgery, is very important for controlling temperature conditions in patients, especially children. Since measurement points of the core body temperature (e.g. tympanic membrane, pulmonary artery, distal esophagus and nasopharynx) are not easily accessible, near core sites are used. These include the mouth, axilla, bladder, skin surface, and rectum (5). Measuring temperature in rectum, as a method of measuring the core body temperature, has remained unchallenged for a century (3). Although it has also been considered a golden standard for the routine determination of body temperature, this method is a frightening method for children and may cause psychological consequences, in older children. Furthermore, this method can cause discomfort and pain for patients with infection or pre-rectal mobility. The rectum is an unsanitary region with high contamination risk (14). Also, this method could be related to the transmission of HIV (17). Rectal and tympanic temperatures were not representative of cardiac temperature, whereas esophageal temperature was representative of cardiac temperature (18). In short, considering rectum temperature measurement, as a golden standard for measuring the core body temperature, is questionable (3). Continuous measurement of skin temperature is also a safe method. Skin temperature is lower than the body temperature. Axiliary temperatures, as well as those measured on the forehead (19), foot, and upper part of the abdomen (20), in infants, are considerably different from the core body temperature. If the temperature difference between the core body temperature and skin temperature is measured, a correction factor can be used to estimate the core body temperature in infants (21).
2. Objectives
The primary aim of this study is to measure skin temperature over the carotid artery and compare it with rectum temperature, to propose a model for the accurate estimation of near core body temperature in children. The secondary aim of the study was the determination of skin temperature over the carotid artery and its comparison with the rectum temperature, according to age, type of operation and duration of operation, in children.
3. Patients and Methods
3.1. Sample Size
After having the study approved by local ethic committee, 124 patients within the age range of 2 - 6 years old, admitted to Children’s Medical Center, Tehran, Iran, for the purpose of surgery, were selected. All patients had an American Society of Anesthesiologists physical status of I or II and were scheduled to undergo standardized general anesthesia. Patients with any medical condition precluding the placement of any temperature probe, or any neurological conditions affecting thermoregulatory functions (e.g. cerebral palsy) were excluded.
After installing the monitoring equipment, 1 µg/kg fentanyl was administered, as the pre-medication. The anesthetics were administered initially by face mask application, in incremental doses to deliver maximum inspired concentrations of 8% - 7% sevoflurane. Then, tracheal intubation was performed. Anesthesia was continued by isoflurane anesthetic inhalation and oxygen. The respiratory system was set in the manner that carbon dioxide blood (CO2) was equal to 35 - 45 mmHg, at the end of the exhalation. The flow rate of fresh gas was set at three litters per minute. Intravenous fluids were at room temperature and the prescribed ringer serum followed the 4/2/1 rule. First, we inserted the rectal probe and then, the orthopedists or urologists and their colleagues sterilized the operation site. The rectal probe was connected to the monitoring system continuously, during the operations, and we monitored the patients’ temperature constantly. However, we only recorded its average every 10 minutes. All the data were measured and recorded under steady anesthetic conditions. Temperature of the operating room was constantly set at 23 ± 1°C, by a central thermostat. The patients’ clothing, during the operation, was the conventional disposable operating room clothing. Required actions were taken in case of observing hyperthermia or hypothermia. In order to measure the temperature, one probe was placed inside the rectum and the other was installed on the skin surface, above the point with maximum carotid artery pulse. Since general anesthesia distributed core body heat toward the periphery and reduced core temperature, we measured these temperature differences, upon reaching an anesthetic steady state. The temperature differences, upon reaching an anesthetic steady state, have been calculated as mean “three” (two - four) centigrade differences. The patients reached the anesthetic steady state in 30 minutes and we started documenting the temperatures from the 30th minute. The temperatures of rectum and skin over the carotid artery were measured and recorded, every 10 min. The thermometers, Temperature Channel 2 Probe Type YSI 400 (Pooyandegan Rah Saadat Co. Ltd., Tehran, Iran) had the following characteristics: compatible range 0 - 50°C, accuracy ± 0.2°C, alarm sources error messages. Then, the patients were randomly divided into two groups (each including 62 subjects), namely modeling (MG) and validation groups (VG).
3.2. Data Analysis
First, in the modeling group, the average temperature of the rectum and skin over the carotid artery were separately calculated. Then, age, sex, and average temperature of the rectum and skin over the carotid artery were entered into the linear regression model. The appropriate model was determined, according to the significance of the model’s coefficients. The obtained model was used to predict the rectum temperature in the second group (studying VG group).
The correlation of the predicted values with the real values (the measured rectum temperature) in the second group was investigated. Also, the difference in the average values of these two groups was examined, in terms of significance. The significance level was set at P < 0.05 for the tests. Pearson’s correlation coefficient and paired t-test were used, for data analysis.
4. Results
In the current study, 43 female (34.7%) and 81 male (65.3%) infants were investigated. The mean age of the patients was 3.48 ± 1.41 years old. The mean age of the MG was 3.29 ± 1.42, while it was 3.86 ± 1.3 years old in the VG. There was no significant difference between the two groups, in terms of age (P = 0.663).
A number of 84 (67.7%), 20 (16.1%), and 20 (16.1%) patients referred to the hospital for abdominal surgery, orthopedic surgery, and urology surgery, respectively.
Demographic information of the participants and the duration of surgeries for MG and VG are shown in Tables 1 and 2. In the MG, the mean rectum and carotid temperatures were 36.47 ± 0.54 and 35.45 ± 0.62°C, respectively. Variables of the mean rectum temperature, mean carotid temperature, age and sex, were entered into the regression model. The model’s coefficients for age and sex were not significant. The value of r2, in this model, was 0.39 (Table 3). After excluding age and sex from the model, the final model was obtained, as follows: Carotid temperature × 0.561 + 16.583 = Rectum temperature. The value of r2 in this model was 0.42.
| Modeling Group | Validation | |
|---|---|---|
| Age | 3.43 ± 1.5 | 3.54 ± 1.3 |
| Duration | 46.45 ± 13.3 | 50.2 ± 13.4 |
aData are represented as mean ± SD.
| Variables | Modeling Group | Validation Group |
|---|---|---|
| Gender | ||
| Male | 40 (64.5) | 41 (66.1) |
| Female | 22 (35.5) | 21 (33.9) |
| Surgery | ||
| Abdominal surgery | 42 (67.8) | 42 (67.7) |
| Orthopedic surgery | 10 (16.1) | 10 (16.1) |
| Urology surgery | 10 (16.1) | 10 (16.1) |
aData are presented as No. (%).
| Model | β-Coefficient | Standard Error | P |
|---|---|---|---|
| Constant | 16.729 | 3.123 | 0.000 |
| Mean Carotid | 0.556 | 0.088 | 0.000 |
| Gender | -0.044 | 0.116 | 0.704 |
| Age | 0.023 | 0.037 | 0.542 |
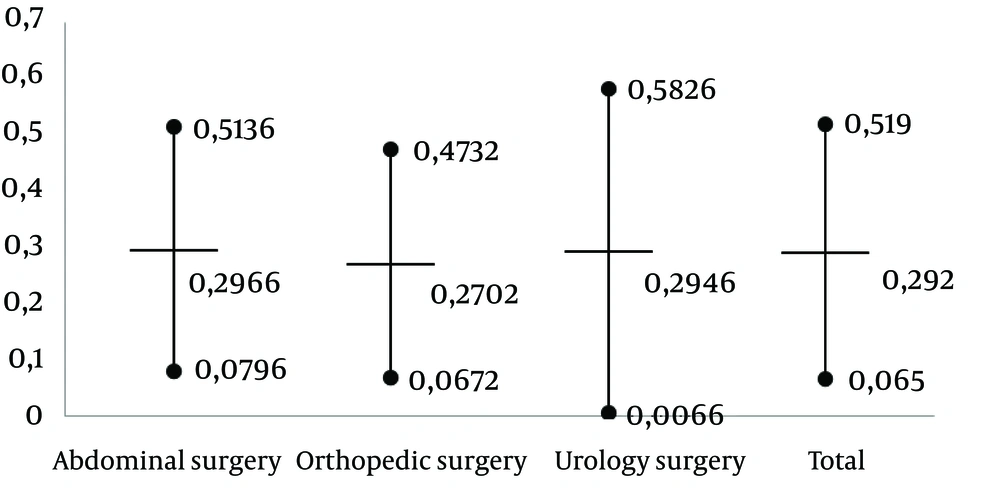
A plot for illustrating the mean bias and confidence interval is shown in Figure 1.
In the next step, the predicted value was calculated based on the regression model and then compared with the measured rectum value, which showed no significant difference (P = 0.361) (Table 4). The correlation between rectum temperature values and the values predicted by the model in the VG was also obtained as r = 0.788 (P < 0.001).
| Variable | Values | T | P |
|---|---|---|---|
| Temperature | 0.92 | 0.361 | |
| Rectal temperature in validation group | 36.41 ± 0.29 | ||
| Temperature predicted by the model | 36.38 ± 0.50 |
aAbbreviation: T value (Student t test).
bData are presented as mean ± SD.
5. Discussion
The present study showed that skin temperature over the carotid artery can be used as a non-invasive method for estimating rectum temperature, which accurately reflects near core temperature, among infants and children undergoing elective surgery with general anesthesia. One advantage of measuring temperature via skin is that this method makes continuous evaluation of the body temperature possible and provides core body temperature measurement much safer than other invasive methods. In the present study, no patient experienced any kind of skin damage. Measuring rectum temperature is not a desirable method for nurses and parents, and many hospitals have discarded this method. This is a cultural reluctance, which especially exists in Britain, Australia, and New Zealand (3). The skin over carotid artery is an appropriate criterion for the core body temperature, because of its proximity to a large artery (21). In the present study, it was shown that the method of measuring skin temperature over carotid artery had an acceptable accuracy, in terms of estimating rectum temperature. This method is completely safe and can be applied for patients on whom invasive methods cannot be used, due to cases with medical complexity.
It is necessary to use alternative methods for estimating core body temperature. Measuring body temperature of infants and children, via the skin over carotid artery, is a simple, accessible, safe and accurate method, which can predict near core body temperature, using a model, and can be practically used for anesthesia in infants and children.