1. Background
Coronary artery disease (CAD) is one of the leading causes of death worldwide. Patients with CAD require coronary artery revascularization as well as other medical treatments (1). Coronary artery bypass grafting (CABG) is a common interventional surgery in order to treat end-stage coronary artery occlusion disease. Although CABG is an effective method, it may also come with particular complications during and after the surgery (1, 2). CABG may lead to disorders in platelet count, coagulation, and fibrinolysis. Excessive amounts of bleeding after surgery is a common problem that sometimes requires blood transfusions or even reoperation (3-6).
Desmopressin is an artificial form of vasopressin which is commonly used to prevent bleeding in hemophilia and Von Willebrand disease (7, 8). Previous investigations have shown that desmopressin can decrease the amount of blood products needed in transfusion for cardiac surgery (9). However, some studies have indicated that desmopressin was not effective when used as a prophylaxis (10, 11). Still, some other studies have shown that using desmopressin could reduce bleeding in post-CABG patients, patients with long cardiopulmonary bypass pump (CPBP) times, and high-risk patients who had taken anti-platelet medication (9, 12-16).
2. Objectives
According to the general importance of the issue and the conflicting results on the effects of desmopressin on bleeding after cardiac surgery, and also concerning the lack of previous studies which have assessed the effects of intranasal desmopressin on bleeding after cardiac surgery, we aimed to investigate the effects of desmopressin on the bleeding rates in patients who had undergone CABG with a CPBP after taking anti-platelet medicine.
3. Methods
We conducted a randomized double-blind clinical trial in the anesthesiology research center of Guilan University of Medical Sciences (GUMS) in Rasht, Iran. This study was approved by the ethics committee of GUMS with the reference number of 1930252810 and registered in the Iranian registry of clinical trials (IRCT) under the number IRCT201409304345N3.
Inclusion criteria were Class II-III status according to the American society of anesthesiologists’ physical status classification system, 3-vessel coronary artery disease, ejection fraction of ≥ 40%, reception of anti-platelet medicines including aspirin of 80 mg/day and clopidogrel of 75 mg/day before surgery, no history of coagulopathy or renal impairment, and having been scheduled for CABG with a CPBP.
Exclusion criteria were a pump time > 120 minutes, concomitant valve procedure and CABG, inotrope administration for separating the patient from the cardiopulmonary pump, need for anticoagulant therapy during and/or in the post-operative period, and coronary endarterectomy.
The sample size was determined according to the following formula derived from the study by Gratz et al. (17):
α = 0.05
Z1-α/2 = 1.96 (95% confidence interval was noted)
β = 0.20
Z1-β = 0.85
µ1 = 1176, S1 = 674
µ2 = 833, S2 = 311

n = 50 Patients in each group.
Using the method of random blocking, 100 patients were divided into two groups (desmopressin: group D and placebo: group P) with 50 patients in each group. At the time of hospitalization, the type of surgery and anesthesia method were explained for patients, and written informed consent was obtained.
In the preoperative period, blood levels of hemoglobin (Hb), platelets, prothrombin time (PT), partial thromboplastin time (PTT), international normalized ratio (INR), and fibrinogen were measured and recorded. The anesthesiologist advised patients to fast the night before surgery. For premedication, oral lorazepam of 1 mg was administered the night before and one hour prior to surgery. An hour before induction of anesthesia, intramuscular morphine sulfate of 0.1 mg/kg was injected into all patients. Thirty minutes before anesthesia, the desmopressin or placebo was administered. In group D, two puffs of intranasal desmopressin (Sina Vista Daroo manufacturing, Tehran, Iran) were sprayed. Each puff contained 10 μg of desmopressin. In group P, 2 puffs of intranasal saline (normal saline in a desmopressin container) were sprayed.
The patients and the anesthesiologist had no awareness about the drug type administered during and after surgery. Also, the laboratory technician was unaware of the drug type. The researcher was the only one who was aware of the medication so that he could take any necessary actions if complications occurred.
Patients were monitored under standard protocols including 7-lead electrocardiography (EKG), pulse oximetry, and bispectral indexing (BIS) in the operating room.
Before induction of anesthesia, the cardiac anesthesiologist inserted one peripheral venous catheter, a left radial artery catheter, and a central venous catheter under local anesthesia with lidocaine of 1%.
Patients received 5 - 7 ml/kg isotonic saline before induction of anesthesia. After preoxygenation, anesthesia was induced by slow injection of midazolame of 0.05 mg/kg and sufentanil of 1 μg/kg (over the course of 10 minutes) intravenously, followed by infusion of 0.2 mg/kg cisatracurium for muscle relaxation.
After intubation, anesthesia was maintained by propofol of 50 - 75 μg/kg/min, sufentanil of 0.2 μg/kg/h, and atracurium of 0.6 μg/kg/h. Then, a nasopharyngeal thermometer was inserted, and in order to maintain the depth of anesthesia, BIS during surgery was maintained between 40 and 60. Then, patients underwent median sternotomy, a standard technique was used to establish a CPBP.
Activated clotting time (ACT) was also measured following the administration of 300 μg/kg heparin. Cardiopulmonary bypass was initiated if ACT ≥ 480 seconds. Upon completion of the grafts, if vital signs were stable, patients were separated from the pump, and the circulating heparin was antagonized by protamine sulfate.
After the surgery, patients were transferred to the intensive care unit (ICU), resuming ventilation under close observation. Patients were extubated about six to eight hours after operation if they were awake, calm, had normal arterial blood gas analysis, and acceptable breathing status.
If the patients had VAS > 3, intravenous morphine of 0.1 mg/kg was injected. Six hours after transferring the patients to the ICU, in group D, two puffs of intranasal desmopressin equivalent to 20 μg, and in group P, two puffs of intranasal placebo (isotonic saline), were sprayed. If the patients had nausea and vomiting (desmopressin complications), metoclopramide of 0.1 mg/kg was injected.
In the ICU, the amount of blood in the chest bottle, Hb level, and platelet count were observed. If the Hb level reduced to less than 10gr/dL, or if the platelet level was less than 100,000/mm3, packed red blood cells (PRBC) or platelet concentrate were injected, respectively.
Investigators measured the levels of Hb, platelets, fibrinogen, PT, PTT, and BT 24 hours after surgery.
3.1. Statistical Analysis
After collection, data were entered into SPSS software version 17. Data were reported by descriptive statistics (number, percent, mean, and standard deviation) and analyzed with a chi-squared test, an independent T-test, a Mann-Whitney U test, and a paired T-test. For intragroup comparison of variables after surgery, ANCOVA was used. A P value < 0.05 was considered as statistically significant, and a 95% confidence interval was noted.
4. Results
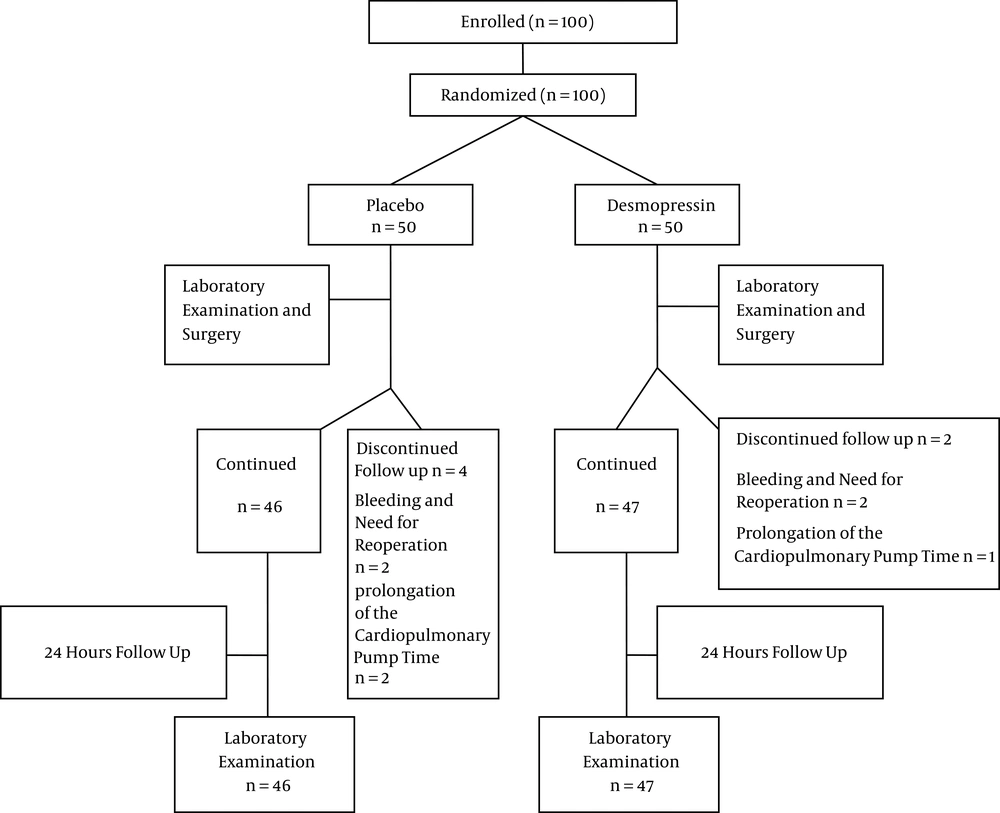
Of the 100 patients initially enrolled in this study, seven patients were excluded. Therefore, 47 and 46 patients participated in groups D and P, respectively. Two patients in group D and two patients in group P were excluded as a result of bleeding and reoperation required to control it. A prolonged cardiopulmonary pump time resulted in the exclusion of one patient in group D and two patients in group P (Figure 1).
There were no significant differences between the groups regarding age, gender, body mass index (BMI), ejection fraction (Table 1), duration of surgery, pump time, and aortic clamp time (Table 2). Also, there was no significant difference between the groups regarding the outbreak of complications such as nausea, vomiting, blood pressure alteration, and the amount of bleeding (P > 0.05).
aIndependent T-test.
bChi-squared test.
| Variables | Group D | Group P | P Valuea |
|---|---|---|---|
| Duration of surgery, h | 2.89 ± 0.42 | 2.92 ± 0.44 | 0.73 |
| Pump time, min | 57.2 ± 9.01 | 56.7 ± 8.83 | 0.79 |
| Aortic clamp time, min | 37.34 ± 9.43 | 36.08 ± 9 | 0.51 |
aIndependent T-test.
Thirty-nine patients received PRBC, and 13 patients received platelet concentrate. The results showed no significant difference between these groups (p=0.472) (Table 3).
| Variables | Group D | Group P | P Value |
|---|---|---|---|
| Hypotension | 0.533a | ||
| Yes | 6 (12.8%) | 8 (17.4%) | |
| No | 41 (87.2%) | 38 (82.6%) | |
| Nausea | 0.109a | ||
| Yes | 11 (23.4%) | 5 (10.9%) | |
| No | 36 (76.6%) | 41 (89.1%) | |
| Vomiting | 0.57a | ||
| Yes | 2 (4.3%) | 1 (2.2%) | |
| No | 45 (95.7%) | 45 (97.8%) | |
| Bleeding volume, mL | 359.3 ± 266.2 | 406.3 ± 341.6 | 0.208b |
| Blood transfusion, packed cell | 0.472a | ||
| Yes | 18 (38.3%) | 21 (45.7%) | |
| No | 29 (61.7%) | 25 (54.3%) | |
| Platelet transfusion | 0.797a | ||
| Yes | 7 (14.9%) | 6 (13%) | |
| No | 40 (85.1%) | 40 (87%) | |
| Packed red blood cell transfusion, U | 0.65 ± 1.06 | 0.82 ± 1.32 | 0.596b |
aChi-squared test.
bMann-Whitney U test.
| Variables | Group D | Group P | Estimate Within Group , P Valuea | Estimates Between Groupsb |
|---|---|---|---|---|
| Hemoglobin | 0.134 | |||
| Preoperative | 13.63 ± 1.78 | 13.12 ± 2.18 | 0.221 | |
| Postoperative | 11.71 ± 1.45 | 11.15 ± 1.31 | 0.058 | |
| Estimate within group, valuec | 0.0001 | 0.0001 | ||
| Platelets | 0.012 | |||
| Preoperative | 243489 ± 74577 | 240239 ± 46991 | 0.802 | |
| Postoperative | 226176 ± 91502 | 194456 ± 46514 | 0.038 | |
| Estimate within group, P valuec | 0.042 | 0.0001 | ||
| INR | 0.665 | |||
| Preoperative | 1.0 ± 0.21 | 1.05 ± 0.14 | 0.86 | |
| Postoperative | 1.11 ± 0.19 | 1.14 ± 0.22 | 0.964 | |
| Estimate within group, P valuec | 0.005 | 0.011 | ||
| PT | 0.463 | |||
| Preoperative | 12.85 ± 0.71 | 12.82 ± 0.62 | 0.88 | |
| Postoperative | 13.28 ± 1.29 | 13.55 ± 2.12 | 0.941 | |
| Estimate within group, P valuec | 0.017 | 0.011 | ||
| PTT | 0.588 | |||
| Preoperative | 30.97 ± 5.96 | 30.98 ± 7.47 | 0.134 | |
| Postoperative | 29.73 ± 8.63 | 28.77 ± 8.55 | 0.517 | |
| Estimate within group, P valuec | 0.029 | 0.085 | ||
| BT | 0.129 | |||
| Preoperative | 1.3 ± 0.39 | 1.42 ± 0.42 | 0.223 | |
| Postoperative | 1.69 ± 0.56 | 1.55 ± 0.58 | 0.173 | |
| Estimate within group, P valuec | 0.0001 | 0.285 | ||
| Fibrinogen | 0.265 | |||
| Preoperative | 302.9 ± 34.3 | 288.7 ± 45.6 | 0.091 | |
| Postoperative | 261.4 ± 37.4 | 247.8 ± 35.1 | 0.075 | |
| Estimate within group, P valuec | 0.0001 | 0.0001 |
Abbreviation: BT, bleeding time; INR, international normalized ratio; PT, prothrombin time; PTT, partial thromboplastin time.
aIndependent T-test.
bANCOVA.
cPaired T-test.
A paired T-test revealed that the Hb levels decreased significantly in each group after surgery (P = 0.0001), but the difference was not statistically significant between the groups (0.134).
The alterations of platelets in the D and P groups were statistically significant (P = 0.042, P = 0.0001, respectively). A T-test showed no significant difference in mean platelet levels between the groups before surgery (P = 0.802), but there was a significant difference between the groups in terms of the mean platelet levels after surgery (P = 0.038). The PT, PTT, INR, BT, and fibrinogen changes before and after surgery showed no significant differences between the groups (P > 0.05).
5. Discussion
Severe bleeding after cardiac surgery consistently remains a challenge for cardiac surgeons and anesthesiologists. Using a cardiopulmonary pump in cardiac surgery may induce blood coagulation disorders and platelet dysfunction, requiring transfusion of proper functioning platelets or the administration of other medicines (3-6). Up until now, diverse products including desmopressin, albumin, recombinant factor VII, and tranexamic acid have been used to reduce bleeding after cardiac surgery (12, 15, 18-20). Desmopressin is an artificial form of vasopressin or an antiduretic hormone (ADH) analogue that exerts its anti-hemorrhagic effects through increased plasma levels of factor VΙΙΙ and increased activity of the Von Willebrand factor. It also has a direct effect on the blood vessel.
Our study showed no significant differences between the groups regarding the demographic characteristics, pump times, clamp times, and durations of surgery. Also, the frequency of complications such as nausea, vomiting, and hypotension was not significantly different between the groups. Furthermore, no significant difference was noted between the groups regarding the amount of blood collected in the chest bottle and the number of transfused PRBC units.
Pleym et al. observed no significant difference in the amount of blood loss after prescribing 0.3 mcg/kg of desmopressin in patients undergoing CABG (21). They reported 606 and 601 cc of blood loss in the desmopressin and saline groups, respectively. They finally declared that taking desmopressin had no significant effect on bleeding after CABG in patients treated with aspirin the day before surgery. Their finding was consistent with our study, but with increasing doses of desmopressin, different results might be achieved. Cattaneo et al. showed that although the use of desmopressin reduced postoperative bleeding, it did not reduce the need for blood transfusions (12). In both groups, the same amount of blood was transfused. Also, in this study, researchers noted that the effectiveness of desmopressin depended on the amount of bleeding, and by an increase in bleeding of about 1.1 liters, the effect of desmopressin on reducing blood loss could be more apparent (12). It seems that low rates of bleeding could indicate the supposed ineffectiveness of desmopressin in our study (359.3 ± 266.2 mL in group D, and 406.3 ± 341.6 in Group P).
In our study, it was observed that Hb levels dropped after surgery in each group, and this amount was significant. However, comparing Hb levels before and after surgery in both groups indicated no significant difference. Also, Pleym et al. noted similar results (21). Furthermore, platelet counts after surgery decreased significantly in both groups in our study. Platelet counts in group P were lower than those of group D, but this difference was not clinically considerable, and in both groups, postoperative platelet counts were enough to maintain homeostasis. In contrast to our study, Pleym et al. reported a different result (21). They indicated that despite a decrease in platelets after surgery in both groups, the rate of thrombocytopenia was higher in the desmopressin group. This different result might be due to other factors such as the cardiopulmonary pump effect.
In addition, there was no significant difference between groups in BT before and after surgery (P = 0.129). In a study by Keyl et al. which examined the effects of aspirin and intravenous desmopressin of 0.4 μg/kg on platelet function in patients undergoing CABG, they observed that desmopressin did not affect platelet activity (22). In our study, 40 μg of intranasal desmopressin in the form of four puffs was administered before (two puffs) and six hours (two puffs) after surgery. Intranasal desmopressin at high dosages may produce an elevation of blood pressure, which disappears with reduction in dosage. Therefore, this drug should be used with caution in patients with coronary artery insufficiency and/or hypertensive cardiovascular disease and heart failure. For this reason, in our study, the lower dosage of desmopressin was used. In Keyl et al.’s study, similar to ours, desmopressin did not improve platelet function. However, their study focused on platelet activity more than platelet count. In our study, platelet count and BT were also investigated.
Our results showed that PT and INR increased after surgery, but this difference was not significant when comparing the two groups. The only variable with a downward trend in coagulation parameters was PTT. However, a significant difference in this variable was not observed between the groups. Generally, desmopressin did not improve platelet count or function, nor did it improve coagulation status. In a review study, Wademan and Galvin (23) examined the effects of desmopressin in reducing bleeding after heart surgery. They announced that desmopressin could not induce beneficial effects either before or after heart surgery. In their study, desmopressin improved the hemostatic status in those patients consuming aspirin for seven days prior surgery, having a pump time of more than 140 minutes, or having preoperative platelet dysfunction. Also, in a meta-analysis, Levi et al. (24) showed that desmopressin might cause a slight reduction in the amount of bleeding after heart surgery without any clinical improvements.
5.1. Limitations
In this study, we investigated the platelet counts and BT. It is recommended that in future studies, further platelet function tests such as optical aggregometry, flow cytometry, or PFA-100 could be used. Also, it seems that measuring the Von Willebrand factor and factor VΙΙΙ levels before and after surgery could prove to be valuable.
5.2. Conclusion
Our study showed that desmopressin could not reduce the amount of blood loss after CABG surgery. Also, desmopressin did not have a significant effect on coagulation status. Therefore, based on our study, it seems that the use of this medication cannot be considered as helpful in candidates for CABG surgery.