Abstract
Background:
One of the main challenges in anesthesiology is difficult intubation. There are many anatomical parameters for evaluating the feasibility of tracheal intubation; one that can reliably predict a difficult intubation is the Cormack-Lehane classification obtained during direct laryngoscopy. This is an invasive procedure that cannot be performed in an awake patient or for pre-anesthetic airway assessments in patients with no prior history of tracheal intubation. Recently, ultrasound has been successfully used for several airway-related applications.Objectives:
The aim of this study was to compare and correlate the ultrasound view of the larynx with the Mallampati classification before anesthesia and the Cormack-Lehane classification during direct laryngoscopy under general anesthesia.Methods:
This cross-sectional descriptive-analytic study included 53 ASA class I - III patients aged 18 - 70 years who were scheduled for tracheal intubation under general anesthesia. Before anesthesia, an oblique transverse ultrasound view of the airway was obtained; in addition, the total time taken to achieve the final plane, the depth of the pre-epiglottic space, and the distance from the epiglottis to the mid-point between the vocal cords were all recorded. The ultrasound measurements were then compared with the Mallampati class on the preoperative evaluation and with the Cormack-Lehane grade during direct laryngoscopy under general anesthesia.Results:
It was observed that correlations between the pre-epiglottic space (PE) and Cormack-Lehane grades I, II, and III were weak. Correlations between the distance from the epiglottis to the vocal cords (E-VC) and Cormack-Lehane grades I, II, and III were also weak. The PE/E-VC ratio for correlations between the sonographic view and laryngoscopy had 87.5% sensitivity and 30% specificity. There was no correlation between Mallampati class and the PE/E-VC ratio (P = 0.566).Conclusions:
Our study revealed weak correlation between PE/E-VC and Cormack-Lehane grade, with 87% sensitivity and 30% specificity. Therefore, we concluded that sonographic measurement criteria are not accurate in airway evaluations before anesthesia.Keywords
Cormack-Lehane Classification Direct Laryngoscopy Endotracheal Intubation Mallampati Classification Ultrasonography
1. Background
One of the main challenges in anesthesiology is difficult intubation. Many clinical criteria have been introduced with regard to evaluation of the patient’s airway before induction of anesthesia, including Mallampati classification, mouth-opening size, thyromental distance, neck extension, jaw protrusion, and the upper-lip bite test (1).
A method that can rather reliably predict difficult intubation is the Cormack-Lehane classification, which is done with direct laryngoscopy. However, laryngoscopy is an invasive procedure that is almost impossible to perform in an awake patient, and it cannot be used to predict difficult tracheal intubations in patients undergoing general anesthesia for the first time (2, 3).
On the other hand, ultrasonography is a non-invasive, safe, and painless modality for evaluating the soft tissues. Different sonographic techniques for airway evaluations have been used in prior studies (4-6). Using 24 healthy volunteers, Singh et al. performed systematic sonographic examinations of the upper airway from the floor of the mouth to the suprasternal notch, and concluded that this technique was capable of providing detailed anatomic information, with numerous potential clinical applications (6).
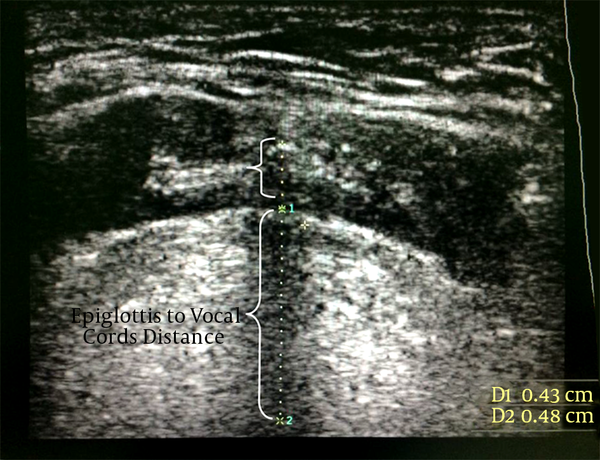
In a study by Gupta et al. on 72 patients scheduled for tracheal intubation under general anesthesia, the following measurements were obtained on oblique-transverse ultrasound views of the airway: (a) the distance from the epiglottis to the midpoint of the distance between the vocal folds, (b) the depth of the pre-epiglottic space (PE), and (c) the total time taken by the operator to achieve the final ultrasonic image. These data were compared with the Cormack-Lehane classification obtained during direct laryngoscopy in the operating room. It was found that Cormack-Lehane (CL) grade can be adequately (with 67% - 68% sensitivity) predicted by the ratio of PE and E-VC distances (PE/E-VC) {0 < [PE/E-VC] < 1 ≈ CL grade 1; 1 < [PE/E-VC] < 2 ≈ CL grade 2; and 2 < [PE/E-VC] < 3 ≈ CL grade 3} (7).
2. Objectives
The primary endpoint of our study was to compare and correlate the ultrasound view of the larynx before anesthesia with Cormack-Lehane classification during direct laryngoscopy under general anesthesia. The secondary endpoint was to compare and correlate the ultrasound view of the larynx with Mallampati classification, evaluated before anesthesia induction.
3. Methods
This cross-sectional descriptive-analytic study was performed in 2015 at Dr. Shariati hospital of Tehran University of Medical Sciences. The study included 53 ASA class I–III patients aged 18 - 70 years, who were scheduled for elective surgery under general anesthesia with direct laryngoscopy and endotracheal intubation.
The exclusion criteria were edentulousness, anatomical abnormalities of the craniocervical region, a mouth opening of < 4 cm, inability to hyperextend the neck, body mass index of ≥ 40, and fractures of the maxillofacial or cervical bones.
After obtaining informed oral consent from each patient, pre-anesthetic assessment of the airway was documented based on Mallampati classifications as follows:
Class 1: Full visibility of tonsils, uvula, and soft palate.
Class 2: Visibility of hard and soft palate, upper portion of tonsils, and uvula.
Class 3: Visibility of soft and hard palate and base of the uvula.
Class 4: Only hard palate visible.
Next, ultrasound views of the airway were obtained by an anesthesiology resident under the supervision of the attending anesthesiologist, using a high-frequency linear probe (Medison L5-12EC). Each patient was placed in the supine position with active maximal head-tilt and chin-lift, and the probe was placed in the midline aspect of the submandibular region. The position of the probe was kept unchanged, only rotating from cephalad (plane A, a coronal plane to see the mouth opening) to caudal (plane G, an oblique transverse plane bisecting the epiglottis and posterior-most part of the vocal folds with arytenoids) in a single two-dimensional view. Further rotation of the ultrasound probe was stopped upon visualization of plane G (Figure 1).
Ultrasonic Planes for Airway Assessment
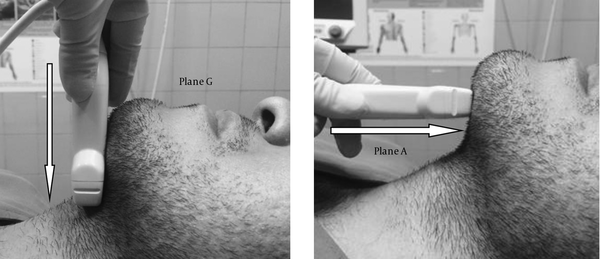
Plane G was used for sonographic measurements, including (I) the distance from the epiglottis to the midpoint distance between the vocal folds and (II) the PE depth (Figure 2). The total time taken to obtain plane G was also recorded.
Ultrasonic View in Plane G for Measurement of the Distance From the Epiglottis to the Midpoint of the Distance Between the Vocal Folds, and the Depth of the Pre-Epiglottic Space
Subsequently, the patient was taken to the operating room, where standard general anesthesia procedures were performed by the anesthesiologist. The anesthesiologist was asked to document the Cormack-Lehane grade of the vocal-cord view by direct laryngoscopy performed intra-operatively, as follows:
Grade I: Visualization of the entire laryngeal aperture.
Grade II: Visualization of parts of the laryngeal aperture of the arytenoids.
Grade III: Visualization of only the epiglottis.
Grade IV: Visualization of only the soft palate.
Correlations between pre-operative Mallampati classifications and Cormack-Lehane grades were assessed. The regression coefficients for correlating the ultrasound measurements and Cormack-Lehane grade were then determined, and a P value of < 0.05 was considered significant.
3.1. Statistical Analysis
Statistical analysis was performed using SPSS (version 22, SPSS, Chicago, IL, USA). The correlation between nominal and qualitative variables was assessed using the Chi-square test. The correlation between independent quantitative and qualitative variables was assessed with the t-test. Correlation coefficient and regression analyses were used for quantitative variables. Receiver operating characteristic (ROC) was used for calculation of sensitivity and specificity.
4. Results
Of the 53 consecutive patients who were enrolled in this study, three were excluded due to regional anesthesia and another three were excluded because the related technical data collection was incompletely recorded. A total of 47 patients were finally analyzed.
The demographic data of the patients are presented in Tables 1 and 2. We had no cases of Cormack-Lehane grade IV in our patients. The average time of laryngeal sonography was 27 ± 1.14 seconds.
The correlation between PE and Cormack-Lehane grade I was weak, with a regression coefficient of -0.261 (95% CI, -0.77 to 1.484; P = 0.076). The correlation between the distance from the epiglottis to the vocal cords (E-VC) and Cormack-Lehane grade I was weak, with a regression coefficient of 0.029 (95% CI -1.744 to -2.114; P = 0.847). The correlation between PE and Cormack-Lehane grade II was weak, with a regression coefficient of -0.354 (95% CI 1.759 to 0.204; P = 0.051). The correlation between the distance from the epiglottis to the vocal cords (E-VC) and Cormack-Lehane grade II was weak, with a regression coefficient of -0.074 (95% CI -1.489 to -2.469; P = 0.62). The correlation between PE and Cormack-Lehane grade III was weak, with a regression coefficient of 0.125 (95% CI -0.698 to 1.705; P = 0. 403). The correlation between the distance from the epiglottis to the vocal cords (E-VC) and Cormack-Lehane grade III was weak, with a regression coefficient of 0.151(95% CI -1.402 to 4.313; P = 0.310).
Demographic Data of the Study Patient Population
| Variable | Valuesa |
|---|---|
| Male/female | 34/13 |
| Age, y | 39.1 ± 11.3 |
| Weight, kg | 71.9 ± 1.1 |
| Height, cm | 165.2 ± 9.1 |
| BMI, kg/m2 | 26.4 ± 4.7 |
| ASA Class I/II/III | 15/30/2 |
Frequency of Cormack-Lehane Grades in the Study Population
| Cormack-Lehane Grade | Number of Patients |
|---|---|
| I | 23 |
| II | 18 |
| III | 6 |
| IV | 0 |
The correlation between the PE/E-VC ratio and Cormack-Lehane grade I was weak, with a regression coefficient of 0.131 (95% CI -0.052 to 0.133; P = 0.310). The correlation between the PE/E-VC ratio and Cormack-Lehane grade II was weak, with a regression coefficient of -0.110 (95% CI -0.130 to 0.060; P = 0.461). The correlation between the PE/E-VC ratio with Cormack-Lehane grade III was weak, with a regression coefficient of -0.035 (95% CI -0.156 to 0.133; P = 0.813).
The PE/E-VC ratio for the correlation between the sonographic view and laryngoscopy showed 87.5% sensitivity and 30% specificity. There was no correlation between Mallampati class and the PE/E-VC ratio (P > 0.05).
5. Discussion
Evaluation of the patient’s airway and prediction of difficult intubation before induction of anesthesia is performed using a constellation of criteria, including Mallampati classification, mouth-opening size, thyromental distance, neck extension, jaw protrusion, and upper-lip bite test. These criteria are not applicable in emergency settings or in patients with decreased consciousness and who are uncooperative. Furthermore, the Cormack-Lehane grade does not always correlate with the abovementioned criteria. Therefore, the use of another non-invasive and more accurate method is necessary (1-3).
In prior studies, sonography has been proven to be a non-invasive and reliable method for evaluation of the airway (5, 8 and 9). In a study by Adhikari et al. in 2011, performed on 51 patients undergoing elective surgery under general anesthesia, airway evaluation tests were done before anesthesia. Afterward, the anteroposterior diameters of the geniohyoid muscle and soft tissues of the anterior neck were measured at the level of the hyoid bone, then correlated with Cormack-Lehane grade during anesthesia with direct laryngoscopy. The results showed that sonographic measurements could predict difficult intubation. This was different from our results, which could be partly due to the different sonographic measurement criteria used in our study. On the other hand, the previous study revealed no correlation between Mallampati classification and sonographic measurements, which was in accordance with our study (10).
In a study by Gupta et al. in 2012 on 72 patients undergoing general anesthesia, significant correlations were found between Cormack-Lehane grade and sonographic measurements, PE, and the distance from the epiglottis to the vocal cords (PE/E-VC). They showed that the higher the PE/E-VC ratio, the stronger the possibility of a higher Cormack-Lehane grade on direct laryngoscopy and of difficult intubation. Although the sensitivity of our study was higher than that of Gupta et al. (87% versus 68%), no significant correlation was found between PE/E-VC and Cormack-Lehane grade in our study (7). The reason for this difference could be explained by the different airway anatomies in patients of different races, the smaller sample size in our study, and different levels of experience in performing airway sonography. We also found no correlation between Mallampati class and PE/E-VC ratio, which was not evaluated in Gupta et al.’s study.
Our study revealed a weak correlation between PE/E-VC and Cormack-Lehane grade, with 87% sensitivity and 30% specificity. Therefore, we concluded that sonographic measurement criteria are not accurate for evaluation of the airway before anesthesia.
5.1. Limitations
Forty-seven patients with a maximum age of 50 years were included in our study, which may explain the absence of patients with Cormack-Lehane grade IV. Therefore, it is recommended that the study be repeated with larger sample sizes.
References
-
1.
Shiga T, Wajima Z, Inoue T, Sakamoto A. Predicting difficult intubation in apparently normal patients: a meta-analysis of bedside screening test performance. Anesthesiology. 2005;103(2):429-37. [PubMed ID: 16052126].
-
2.
Adnet F, Racine SX, Borron SW, Clemessy JL, Fournier JL, Lapostolle F, et al. A survey of tracheal intubation difficulty in the operating room: a prospective observational study. Acta Anaesthesiol Scand. 2001;45(3):327-32. [PubMed ID: 11207469].
-
3.
Lundstrom LH, Vester-Andersen M, Moller AM, Charuluxananan S, L'Hermite J, Wetterslev J, et al. Poor prognostic value of the modified Mallampati score: a meta-analysis involving 177 088 patients. Br J Anaesth. 2011;107(5):659-67. [PubMed ID: 21948956]. https://doi.org/10.1093/bja/aer292.
-
4.
Fulkerson JS, Moore HM, Anderson TS, Lowe RJ. Ultrasonography in the preoperative difficult airway assessment. J Clin Monit Comput. 2016. [PubMed ID: 27156094]. https://doi.org/10.1007/s10877-016-9888-7.
-
5.
Hui CM, Tsui BC. Sublingual ultrasound as an assessment method for predicting difficult intubation: a pilot study. Anaesthesia. 2014;69(4):314-9. [PubMed ID: 24641637]. https://doi.org/10.1111/anae.12598.
-
6.
Singh M, Chin KJ, Chan VW, Wong DT, Prasad GA, Yu E. Use of sonography for airway assessment: an observational study. J Ultrasound Med. 2010;29(1):79-85. [PubMed ID: 20040778].
-
7.
Gupta D, Srirajakalidindi A, Ittiara B, Apple L, Toshniwal G, Haber H. Ultrasonographic modification of Cormack Lehane classification for pre-anesthetic airway assessment. Middle East J Anaesthesiol. 2012;21(6):835-42. [PubMed ID: 23634565].
-
8.
Bajracharya GR, Truong AT, Truong DT, Cata JP. Ultrasound-Assisted Evaluation of the Airway in Clinical Anesthesia Practice: Past, Present and Future. Int J Anesthesiol Pain Med. 2015.
-
9.
Kundra P, Mishra SK, Ramesh A. Ultrasound of the airway. Indian J Anaesth. 2011;55(5):456-62. [PubMed ID: 22174461]. https://doi.org/10.4103/0019-5049.89868.
-
10.
Adhikari S, Zeger W, Schmier C, Crum T, Craven A, Frrokaj I, et al. Pilot study to determine the utility of point-of-care ultrasound in the assessment of difficult laryngoscopy. Acad Emerg Med. 2011;18(7):754-8. [PubMed ID: 21707828]. https://doi.org/10.1111/j.1553-2712.2011.01099.x.