1. Background
Surgical procedures cause acute activation of cellular and hormonal factors clinically termed systemic stress response. Increased cortisol secretion from adrenal cortex is one of the main components of the metabolic response to the surgery (1-5). Major surgeries such as thoracotomy and open-heart surgery trigger maximum cortisol secretion. Open-heart surgery with the use of cardiopulmonary bypass (CPB) is associated with significant inflammation compared to off-pump CABG. In CABG with CPB, hemodilution causes more stress which leads to increased levels of plasma cortisol within 24 hours after the surgery. These endocrine and metabolic changes can cause postoperative adverse effects and complications, such as delirium, cognitive dysfunction, impaired immune system and increased oxygen consumption, catabolism and length of hospital stay (5-11). Several studies with different styles of surgery have indicated the influence of anesthesia methods on the acute stress response to the surgery and have examined the effects of a variety of interventions, pharmacologic or non- pharmacologic, with different outcomes in stress reduction (1, 4-6, 8, 11-19). Therefore, it is still necessary to investigate anesthetic agents and methods to suppress the stress response to surgery. It is clear that measuring stress or nociception level during general anesthesia is challenging since there is not a direct method to measure it (20). To our knowledge, the effects of opioid supplemented propofol and isoflurane on cortisol levels have not been previously evaluated in CABG with CPB.
2. Objectives
This clinical trial aimed to compare the effects of Isoflurane-Sufentanil anesthesia and Propofol-Sufentanil anesthesia on plasma cortisol levels in CABG using CPB technique.
3. Methods
This randomized double blind clinical trial took place at an academic hospital in the North of Iran affiliated to Guilan University of Medical Sciences (GUMS) in 2014 from March to October. Before sampling, the research proposal of current study had been approved by the ethics committee of GUMS and registered in Iranian registry of clinical trials (IRCT) by number of IRCT 2015071713456N5.
Sample size: Based on calculations, a sample comprised 36 patients was required in each group to detect the difference between the two groups using a power of 90% and α = 0.05 and β = 0.1.

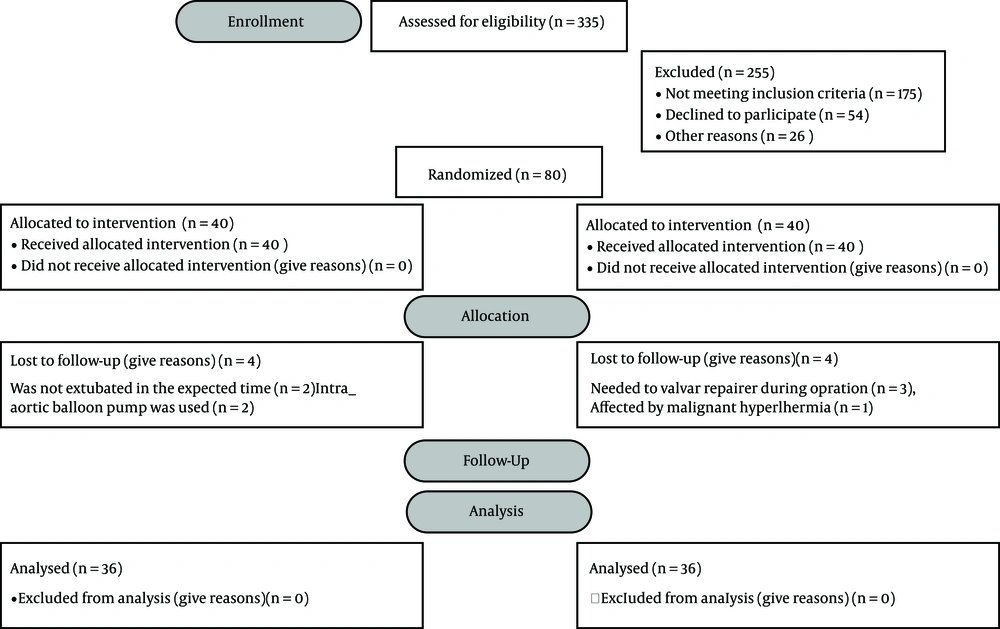
72 Patients aged 18-65 years old, having physical status of II-III according to the guidelines set by the American society of anesthesiologists (ASA), scheduled for elective CABG as an isolated procedure using CPB, were enrolled in the study. The exclusion criteria included: emergency surgery, hepatic or renal failure, neurologic disorders, diabetes, malignancies, BMI (body mass index) > 38 kg/m2, steroid therapy before operation, chronic drug abuse, thyroid dysfunction , redo operation, the need of high dose inotrope infusion or cardiopulmonary resuscitation, hemodynamic instability, long time of surgery, chronic pulmonary disease, Intra-aortic balloon pump (IABP), and extracorporeal membrane oxygenation (ECMO) (21). Before the enrolment, an informed consent form was obtained from every patient. The participants were allocated to one of the two groups using randomized fixed quadripartite blocks. The groups named isoflurane (group I) and propofol (group P), both combined with sufentanil. Our subjects had an equal probability of being assigned to each of the two groups. A responsible anesthesiologist who monitored the patients was aware of the patients’ groups in order to timely intervention in presence of any side effect such as homodynamic changes during and post operation. However, the patient and investigator who recorded the data were blinded. Therefore, this study presented a double blind clinical trial.
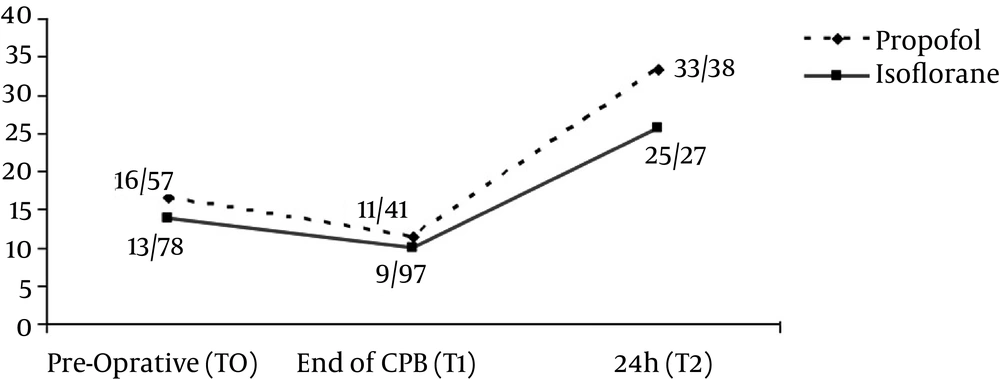
The patients did not receive corticosteroids, before, during, or after the surgery. Patients were recruited one day before the surgery, and venous blood was obtained for baseline biochemical serum measurements, as well as cortisol level. All samples were taken in the morning between 7:30 and 8:30 a.m. Plasma cortisol levels were measured half an hour before operation (T0), at the end of CBP (T1), and 24 hours after the surgery (T2).
Surgery always was started in the morning between 8: 00 and 9: 00 a.m. to avoid bias caused by the circadian rhythm of circulating stress hormones. Our subjects in both groups received oral lorazepam 1 mg, the night before surgery, and one hour before transferring to the operating room, while half an hour before transferring to the operating room they received intramuscular morphine 0.1 mg/kg as premedication. On arrival in the operating room, an 18-gauge intravenous catheter was inserted into a forearm vein and then standard monitoring was applied that included electrocardiography with both leads II and V5 with automated ST-segment analysis to detect ischemia, pulse oximetry, invasive arterial blood pressure, central venous pressure, nasopharyngeal thermometer, Bispectral index; BIS (BIS Quatro Sensor. Spacelabs (Medical) Ultraview SD), End tidal Co2 (Etco2), urine output (UOP) and Noninvasive Blood Pressure (NIBP) with a 3-minute interval. Anesthesia was induced by 0.05 mg/kg midazolam (5 mg/1 mL, midazolam as Hcl, manufactured by Aburaihan Pharmaceutical Co. Tehran-Iran) and 2 µg/kg sufentanil (Sufentanil citrate 0.0075 mg, eq. 0.005 mg sufentanil, sodium chloride solution, Janssen-Cilag). As previous studies have demonstrated, low doses of intra venous anesthetics were used to suppress anesthesia-related adverse effects. Accordingly, propofol (10 mg/mL, B.Braun Melsungen AG.Melsungen, Germany) was administrated to suppress cough caused by opioid (22, 23). After achieving neuromuscular blockade with 0.2 mg/kg cisatracurum (20 mg/10 mL, contains cisatracurium as besylate, Aburaihan Pharmaceutical Co., Tehran, Iran) tracheal was intubated. Anesthesia was maintained with 1% - 1.5% isoflurane in group I and continuous infusion of propofol 50 - 150 mg/kg/min in group P. Both groups received sufantanil 0.1 - 0.3 µg/kg/h and cisatracurium 0.6 mg/kg/h.
A BIS value between 40 and 60 was maintained for an appropriate depth of anesthesia during the surgery. Patients were ventilated with 100% oxygen to an Etco2 concentration of 35 - 40 mmHg. The patients underwent median sternotomy and a standard technique was used to establish heart-lung pump (standard membrane oxygenator Medtronic). To achieve a target activated clotting time, heparin was given at a dose of 300 IU/kg. For myocardial protection, intermittent cold-blood cardioplegia was used during aortic cross- clamping. The patients received protamine fully reverse of the heparin at the end of the surgery. Completing the vascular graft in stable vital signs status, the patients were disconnected from the heart-lung pump, transferred to the CCU (coronary care unit), and after 6 - 8 hours, were disconnected from ventilator and extubated. If the patient complained of pain, morphine 0.1 mg/kg was administrated.
All the statistical analyses were performed using the SPSS statistical software version 16 (SPSS Inc, Chicago, and II). Unpaired T-test and Chi-square test were used to compare the categorical variables between two groups. The data were expressed as mean ± standard deviation. P value < 0.05 was considered as statistically significant.
4. Results
The present study was conducted on 72 patients, underwent elective CABG surgery in CPB form, meeting inclusion criteria. The patients were randomly assigned into two groups of 36 persons, received either isoflurane or propofol, both supplemented with sufentanil (Figure 1). The results revealed no significant difference between the two groups concerning baseline characteristics and preoperative data (Tables 1 and 2). Noticing that the duration of surgery influences the release of neuro-endocrine hormones, although the surgeries were performed by different surgeons, the mean duration of surgery did not differ statistically between two groups. In both groups, plasma cortisol level initially declined after surgery using CPB with no significant difference (P > 0.05), and then slightly increased to maximum of baseline at 24 hours postoperatively (Figure 2). Although both groups showed an increase in plasma cortisol level 24 hours after the surgery, but it was noticeable that group I had significantly less increase in plasma cortisol level (P < 0.05) (Table 3).
| Parameter | Group 1 | Group 2 | P Value |
|---|---|---|---|
| Age (yrs.) | 58.2 ± 5.8 | 55.8 ± 6.1 | 0.093 |
| Sex (M/F) | 25/11 | 27/9 | 0.599 |
| BMI (kg/m2) | 26.8 ± 4.2 | 27.1 ± 3.07 | 0.72 |
| Parameter | Group 1 | Group 2 | P Value |
|---|---|---|---|
| MAP | |||
| Pre-operative (T0) | 89.9 ± 19.4 | 85.4 ± 14.7 | 0.17 |
| End of CPB (T1) | 63.1 ± 12.4 | 67.1 ± 9.3 | |
| 24 hours (T2) | 78.8 ± 11.6 | 80.4 ± 12.2 | |
| CPB time (min) | 58.2 ± 17.9 | 53.8 ± 15.2 | 0.26 |
| Aortic cross-clamp time (min) | 33.6 ± 9.1 | 35.1 ± 14.4 | 0.6 |
| Duration of surgery (hrs) | 2.7 ± 0.4 | 2.8 ± 0.5 | 0.33 |
Abbreviation: MAP = mean arterial pressure.
aMean ± SD, P ≥ 0.05.
5. Discussion
The application of CPB using a heart- lung machine to open heart surgery is associated with preoperative and postoperative stress responses, which triggers a high risk of postoperative organ dysfunction. There has been increasing evidence that CPB may be the reason of some morbidity associated with CABG (21). Stress hormones, adrenocorticotropic hormone (ACTH), cortisol, epinephrine and norepinephrine can be measured to evaluate stress response in surgery, but plasma cortisol concentration is the most frequently used marker for stress induced reactions (3, 24). Plasma cortisol concentration increases from two-to ten folds after induction of anesthesia, during surgery and in the post-operative period, while it returns to normal levels within 24 hours postoperatively; however, depending on the its severity, the surgical trauma may remain elevated for 72 hours (12). Clinical evidence has shown that the choice of the main anesthetic agent and technique influences the stress response by modulating the pathophysiologic pathways, which induce neurohormonal and immunologic alternations, and might reduce the release of stress hormones (25). No single anesthetic drug or combination of anesthetic agents is suitable for anesthesia in every patient undergoing CABG surgery; however the goal is to choose an anesthetic method to prevent wide swings in hemodynamics. Propofol and isoflurane are two anesthetics used in CABG (26, 27). The inhibitory effects of propofol on the sympathoadrenal system are documented in cardiac surgery and volatile anesthetics such as isoflurane have cardio protective effects (25, 26). It has been shown that intravenous and volatile agents in normal doses have minor influences on the endocrine and metabolic pathways. However, opioid supplements might interfere with stress response. It was noticeable that the difference between volatile and intravenous anesthesia on stress response control was reported to be non-significant after addition of opioids, indicating that this class of drug abolishes the stress response. For example, sufentanil mitigates the increase in plasma levels of catecholamine, cortisol, glucose, and free fatty acids during open heart surgery (5, 28). In this study, we observed that serum cortisol levels decreased during the surgery with no significant difference between two groups. The day after surgery, serum cortisol levels increased in both groups. However, group I significantly showed a less increase compared to the group P. Decreasing trend in the cortisol level while pumping is due to the effect of blood dilution in the initial liquid of bypass machine and adrenocortical axis suppression. The results of Taylors’ (2) study support our findings. However, Adams and Mujagic (4, 20) studies claimed that propofol might have advantages over anesthesia with isoflurane, based on measuring cortisol and catecholamine levels as markers for stress response in non-cardiac surgeries. Additionally, Cock et al. (5) performed a study comparing the effect of propofol and isoflurane both combined with remifentanil on stress response in craniotomy surgery and found no significant difference between two groups. It is noticeable that their style of surgery was different, craniotomy versus open heart surgery while craniotomy induces less stress; and the other difference was our use of sufentanil instead of remifentanil. However, the suppressive effect of total intravenous anesthesia on stress response is controversial (27, 29-31). In Fu hai et al. (11) study, patients underwent laparoscopic cholecystectomy received either propofol or sevoflurane, they found that plasma cortisol level was lower in propofol group the day after surgery. In Velissaris et al. (32) study, where changes in plasma cortisol levels were investigated in CABG using CPB versus off pump CABG, a similar increase pattern was observed in both groups over a period of 24 hours after surgery. These data were in contrast to Rashid et al. (21) study, reported that, after an initial decline during the surgery, cortisol levels rose early in both groups, but in CPB group the maximum in cortisol levels was lower and occurred at 4 hours postoperatively. In both groups, it fell gradually within 18 - 24 hours.
Although this clinical trial study was well performed to provide a theoretical basis for optimizing the anesthesia method, our finding sometimes does not agree with the other similar studies. It maybe stem from the difference between the patients’ populations that can explain at least a part of the observed discrepancies. In fact, comparison and interpretation of endocrine response to surgery and anesthesia are difficult, because it is not possible to study the isolated effects of each type of response in the clinical setting. Therefore, still, we do not know what predominant factor is exactly responsible for the initiation of systemic stress response in cardiac surgeries (i.e. cardiopulmonary bypass, the surgical trauma. etc.).
5.1. Limitations
Some of the limitations of the study should be noted as following: sample size was small, the measurement time points of plasma cortisol levels were restricted, and we only observed cortisol level changes till 24 hours after surgery. To evaluate the stress response, we only measured cortisol levels, but growth hormone, glucagon catecholamine and some other markers which also represent the stress response to anesthesia and surgery were not measured.
5.2. Conclusion
Our findings indicate that in CABG surgery with CPB, both isoflurane and propofol in combination with sufentanil have a suppressive effect on post -operative stress response but isoflurane-sufentanil has a superior effectiveness. Yet, further researches with larger sample size and shorter intervals of measurement, in different styles of surgery and anesthetic agents by evaluating more stress markers, are required to choose an anesthetic drug and technique, which can effectively ease or relive stress response leading to benefit patients and show better outcome.