1. Background
Chest injuries are the cause of admission in 8 to 15% and of mortality in 25% of traumatic patients (1). Blunt trauma includes about 73% of total cases of chest injuries (2). The rib fracture is a most common injury associated with blunt chest trauma, involving approximately 10% of trauma patients that is an indication of the severity of chest damage. With the increased number of fractured ribs, mortality and morbidity increase (3). In previous studies, the prevalence of rib fracture in admitted traumatic patients was 4 to 10%, which was associated with 3 to 13% mortality and 16 to 60% pulmonary complications. Chest damage, especially multiple fractures, are associated with severe pain and restricted patient’s ability for a cough and deep breath that can lead to the accumulation of pulmonary secretions, atelectasis, pulmonary infections, and finally respiratory insufficiency (4). The mainstay of treatment of rib fracture includes pain control, chest physiotherapy, and respiratory care (1). Pain control has an important role in the prevention of pulmonary complications (2, 3). Pain is controlled by various approaches such as medical analgesics (e.g. anti-inflammatory drugs, IV narcotics (e.g. opioids), and regional techniques (e.g. intercostal block, intrapleural block, paravertebral block, and epidural block) (5). Retrospective studies showed that epidural analgesia was more efficient than other approaches. Although the epidural method is preferred in current guidelines, it is accompanied by adverse effects such as increased sympathetic block and numbness depending on increasing the dose of administration due to high pain score. They are uncommon but very serious (6). Bupivacaine and dexmedetomidine are used as analgesics.
We aimed to assess continuous thoracic epidural infusion by bupivacaine alone and a combination of bupivacaine and dexmedetomidine to decrease the local anesthetic dose. It has additive analgesic and sedative effects and lower side effects such hypotension compared to clonidine. In our centers, fentanyl is routinely administered as an adjuvant drug. However, here we used dexmedetomidine in combination with LA for evaluating its pharmacodynamics, hemodynamics, and pulmonary complications profile.
2. Methods
This clinical trial (IRCT No. 201701299948N2, ethical No. 94.3-12.8) was conducted in 64 traumatic patients with rib fractures who admitted to surgery and ICU wards. Sample size was selected by α1 = 0.05 0, power = 80, and effect size = 0.7. Inclusion criteria were as follows: traumatic patients with multiple fractures, age > 18 years old, the presence of rib fracture inducing respiratory symptoms, and GCS ≥ 14. Traumatic patients with brain and spine injuries, patients who refused to use epidural catheter, patients with coagulopathies, with allergy to local anesthetics, with systemic and block site (infection), patients under mechanical ventilation, patients with abdominal trauma, bilateral rib fracture, a history of psychological disease and chronic analgesic consumption, patients with anemia, liver function, hospital stay, and with intubated or no intubated state were excluded from the study. After obtaining informed consent from patients and ethical committee confirmation of Tabriz University of Medical Sciences, the patients were randomly assigned to two groups. The first group received thoracic epidural by continuous infusion of bupivacaine and the second group received thoracic epidural by continuous infusion of bupivacaine plus dexmedetomidine, by a catheter (two levels below the last fracture rib), before induction of anesthesia. The two analgesic approaches were performed for 4 days after intervention. Isobaric bupivacaine 0.125% (of bupivacaine 0.5%; MYLAN i.e., we solved 100 mg vial in 100 water and administered it at a rate of 1 to 2 mL/hour, it was equal to 5 mg/hour) and 200 μ/mL dexmedetomidine (Hospira, Inc.) were used. The patients were monitored before and after block and vital signs were recorded. Five minutes before epidural analgesia, the acid-base gas analysis was performed under the same circumstances. ABG was performed in the first 4 days without consideration of prolonged stay in ICU or the ward.
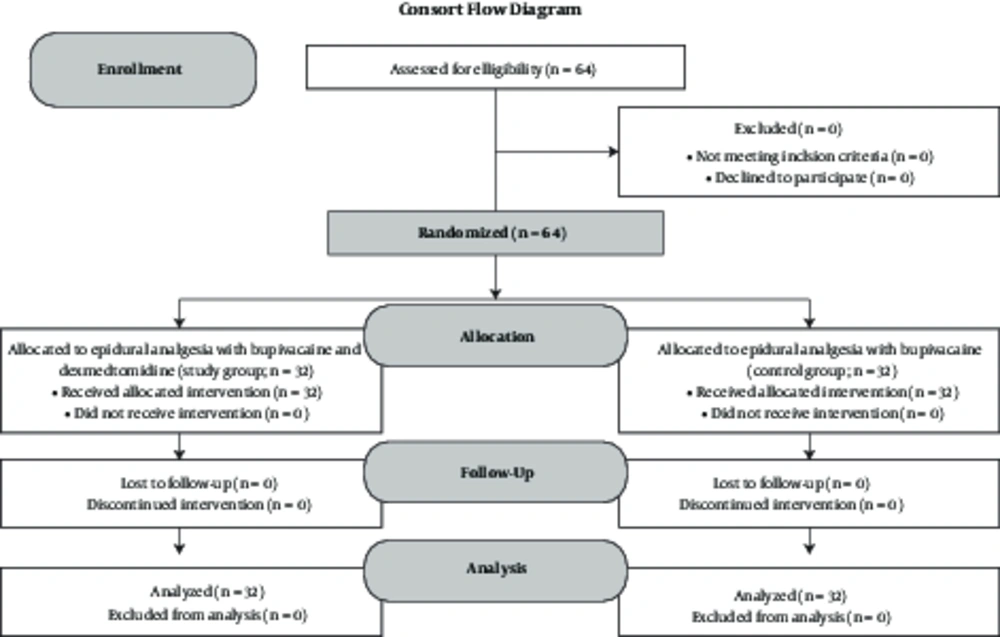
Our questionnaire included demographic data (age, sex, and coexist diseases), trauma-related injuries, the number of fractured ribs, laterality, the location of the fracture, chest tube, prognostic data, and hospital course (e.g., ICU stay and complications such as hypotension, pneumonia, hypoxia, and delayed intubation). Based on the visual analogue scale (VAS), degree and severity of pain were recorded before and after daily block over 4 days. The optimal site for insertion of the thoracic epidural catheter was determined in the patient positioned sitting or lateral (depending on patient tolerance). The tip of the catheter was inserted in the middle fractured level of the rib from two levels below the last fractured rib by an 18-gauge needle and loss-of-resistance and the correct position was confirmed by test does. Accordingly, the primary bolus dose (1.5 mL per segment) of bupivacaine 0.125% was injected. After injecting the test dose, the catheter was inserted and bupivacaine 0.125% and 1 mL/kg/hr plus dexmedetomidine (200 μ/mL) were infused for 3 days. Another group received bupivacaine 0.125% alone using the same technique in the same duration. The catheter was withdrawn after 3 days. We obtained arterial blood sample every day up to 4 days and oxygenation and ventilation parameters including pH, BE, PCo2, SaO2, and PaO2 were recorded along with the pain score. The data were analyzed by SPSS17 and descriptive statistical methods were used. The Chi-square test was used for comparison of qualitative results and One-way ANOVA and non-parametric tests were employed for comparison of quantitative results. In addition, the repeated measure method was used for assessing VAS (visual analog scale) changes. P value < 0.05 was considered significant. The flowchart of the patients is shown in Figure 1.
3. Results
In the present study, 64 cases were studied. 32 cases (15 females and 17 males) received epidural analgesia with bupivacaine (group 1) and 32 cases (16 males and 16 females) received epidural analgesia with combined bupivacaine and dexmedetomidine (group 2). Demographic data are shown in Table 1.
| Variable | Age, y | Time of Hospitalization, day | Duration of the Catheter, day |
|---|---|---|---|
| Group 1 | 55.75 ± 9.51 | 93.0 ± 65.4 | 3 |
| Group 2 | 56.15 ± 7.97 | 99.0 ± 31.4 | 3 |
aValues are expressed as mean ± SD.
The site of the catheter, chief complaint of patients, coexist diseases, associated traumatic injuries and their location, and the number of fractured ribs are listed in Table 2. There was no statistically significant association between the two groups (P value = 0.05).
| Variables | Bupivacaine | Bupivacaine + Dexmedetomidine | P Value |
|---|---|---|---|
| Location of catheter | 0.94 | ||
| T5 - T6 | 10 (31.3) | 10 (31.3) | |
| T6 | 9 (28.1) | 11 (34.4) | |
| T6 - T7 | 9 (28.1) | 8 (25) | |
| T7 - T8 | 4 (12.5) | 3 (9.4) | |
| Chief compliant | 0.44 | ||
| Chest Pain | 14 (43.8) | 11 (34.4) | |
| Chest Pain and distress | 18 (56.3) | 21 (65.6) | |
| Comorbid disease | 0.59 | ||
| HTN | 9 (28.1) | 3 (9.4) | |
| DM | 11 (34.4) | 2 (6.3) | |
| Associated trauma | 0.14 | ||
| Limb fracture | 4 (12.5) | 10 (31.3) | |
| Clavicle fracture | 3 (9.4) | 4 (12.5) | |
| Insertion of chest tube | 0.61 | ||
| Right | 9 (28.1) | 11 (34.4) | |
| Left | 7 (21.9) | 6 (18.88) | |
| No insertion | 16 (50) | 15 (46.9) | |
| Number of fractured rib | 0.22 | ||
| 3 ribs | 15 (46.9) | 9 (28.1) | |
| 4 ribs | 9 (28.1) | 15 (46.9) | |
| 5 ribs | 8 (25) | 8 (25) |
aValues are expressed as No. of cases (%).
The results of ABG after insertion of the epidural catheter are shown in Table 3. Although there were significant differences in pH, PacCo2, and BE values, they were not clinically significant. The authors believed that we need larger trials with more match participants. According to the alteration of values in the normal range, we could not rely on them for the more definite conclusion. Any complications such as bleeding, hematoma, neurologic problems, and infection were not seen.
| ABG | The First Day | The Second Day | The Third Day | The Forth Day | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Bupivacaine | Bupivacaine + Dexmedetomidine | P Value | Bupivacaine | Bupivacaine + Dexmedetomidine | P Value | Bupivacaine | Bupivacaine + Dexmedetomidine | P Value | Bupivacaine | Bupivacaine+Dexmedetomidine | P Value | |
| pH | 7.39 ± 0.07 | 7.38 ± 0.08 | 0.66 | 7.36 ± 0.04 | 7.41 ± 0.03 | 0.025 | 7.39 ± 0.01 | 7.41 ± 0.52 | 0.00 | 7.4 ± 0.01 | 7.41 ± 0.03 | 0.001 |
| BE | 1.02 ± 0.5 | 0.51 ± 0.45 | 0.9 | 1.27 ± 0.48 | 1.34 ± 0.64 | 0.001 | 0.93 ± 0.22 | 1.22 ± 0.57 | 0.00 | 1.76 ± 0.37 | 1.02 ± 0.06 | 0.005 |
| PCo2 | 38.85 ± 3.53 | 39.96 ± 7.43 | 0.002 | 38.88 ± 1.3 | 37.66 ± 0.58 | 0.00 | 38.5 ± 1.52 | 36.28 ± 5.24 | 0.00 | 39.38 ± 2.31 | 36.22 ± 1.8 | 0.7 |
| SaO2 | 81.93% ± 23.18 | 88.76% ± 0.11 | 0.00 | 93.12% ± 2.18 | 93.5% ± 1.2 | 0.003 | 93.71% ± 1.27 | 94.84 ± 1.16 | 0.002 | 93.96% ± 1.53 | 98.31% ± 0.96 | 0.02 |
| PAO2 | 56.34 ± 5.95 | 67.34 ± 5.75 | 0.46 | 71.56 ± 10.64 | 78.01 ± 6.1 | 0.002 | 74.28 ± 18.89 | 84.62 ± 5.24 | 0.023 | 80.87 ± 3.91 | 86.37 ± 8.81 | 0.001 |
In the first group, 8 cases (25%) and in the second group, 3 cases (9.4%) required supplemental oxygen (3 lit/min). There was no statistically significant association between the groups (P value = 0.09). There were significant differences in O2 saturation and PaO2 between the two groups. In the first group, 7 cases (21.9%) to the ICU and 25 cases (78.1%) to the ward were admitted and in the second group, there were 6 cases (18.8%) in ICU and 26 cases (81.2%) in the ward. There was no significant correlation (P value = 0.7).
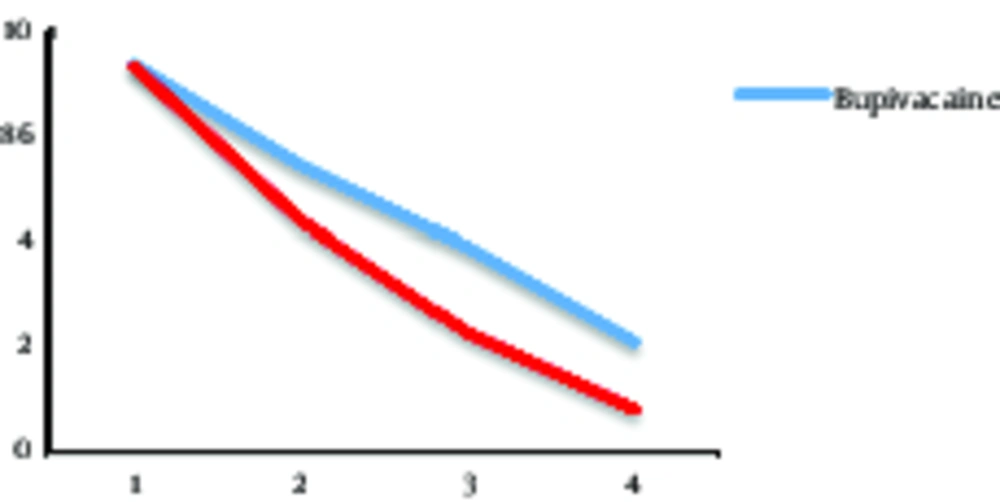
The comparison of visual analog scale (VAS) is shown in Figure 2.
The results suggested that VAS improved in the two groups (P value = 0.002); but in patients who received bupivacaine and dexmedetomidine analgesia, the relief of pain was better than the other group (P value = 0.000). We summarized pain scores in Table 4. There was a significant difference between the two groups and VAS was lower in the group receiving a combination of dexmedetomidine and bupivacaine.
| Bupivacaine | Bupivacaine + Dexmedetomidine | P Value | |
|---|---|---|---|
| 1 | 9.28 ± 7.34 | 9.19 ± 8.53 | 0.510 |
| 2 | 6.85 ± 3.54 | 5.55 ± 2.45 | < 0.001 |
| 3 | 4.90 ± 1.44 | 2.89 ± 0.99 | < 0.001 |
| 4 | 2.67 ± 0.67 | 1.05 ± 0.78 | < 0.001 |
4. Discussion
The results of the present study showed that PaO2 and SaO2 were significantly higher in the epidural group with bupivacaine and dexmedetomidine but PaCO2 was not significantly lower in this group. These variables suggest that the oxygenation and ventilation were better in the epidural group with dexmedetomidine and bupivacaine. VAS was also significantly lower in the epidural group with dexmedetomidine and bupivacaine (P value = 0.000). VAS (visual analog scale) is a scale that presents 0 as “no pain” and 10 as “more severe pain”. In VAS ≥ 4, the second dose of LA is required. The sedation score (1 = wide awake, 2 = dozing, 3 = asleep, and 4 = unrousable) is another test used in this study (6).
The chest may have various ranges from abrasions and bruising to a rib fracture, hemothorax, and pneumothorax which may be associated with rib fracture-induced chest organ injuries (7). Patients who survive of chest trauma suffer from rib fractures by an incidence of 10% of traumatic patients (8). Rib fractures usually did not need special treatments and the patients are recovered over several weeks. In severe cases with multiple fractures, the treatment of pulmonary complications secondary to fracture such as pain is an important aspect (9). The control and management of pain are of prime importance in the case of severe pain, elderly patients, and coexist respiratory failure. In various studies, the efficacy of invasive treatments such as thoracic epidural analgesia was surveyed (10). The approaches of modern anesthesiology have been extended to the perioperative period. The treatment of postoperative pain is a most significant part of appropriate post-surgical care. The untreated pain after surgery can change pathophysiologic neural process. These processes are not limited to peripheral mechanisms and may convert into chronic pain syndromes (11). Thoracic epidural analgesia could reduce mortality and morbidity rates as 6% in elder patients with rib fracture (9). The fractured ribs are main complications that can induce pain and change pulmonary functions (4). The fractured rib can result in pain induced impairment ventilation (12). Analgesia could be induced by several methods such as intravenous analgesia, topical analgesia (e.g. gel), and nerve blocks. Among analgesia approaches (i.e. nerve block), intercostal and intrapleural blocks are the most common approaches. Epidural and spinal anesthesia is used for nerve block (13). Epidural analgesia is considered as a good method for relieving pain. Epidural analgesia with local anesthetic and opioids can result in episodic hypotension (14). Dexmedetomidine is an α2 - agonist that acts as an adjuvant to local anesthetics and prolongs sensory and motor block. Kanazi et al. demonstrated that a low dose dexmedetomidine (3 µg) in combination with intrathecal bupivacaine did not induce hemodynamics change, but can cause early onset of motor block (15). Another study concluded that caudal epidural analgesia with low-dose dexmedetomidine (2 µg) in combination with intrathecal bupivacaine 0.25% in children undergoing abdominal surgery promoted analgesia and anesthesia without increasing side effects (16).
Fouad Selim et al. obtained better results with dexmedetomidine plus local anesthetic regarding patient satisfaction and fewer side effects such as hypotension (6). Mahmoud et al. concluded that epidural analgesia plays an important role in traumatic rib fractures in comparison with parenteral analgesia (17). Bajwa et al. suggested that epidural analgesia with bupivacaine and morphine evaluated by VAS, ABG, and clinical assessments had similar results, increased patient comfort, and accompanied by the absence of pulmonary complications. Bjwa et al. showed dexmedetomidine is a good alternative to fentanyl in epidural analgesia for patients undergoing orthopedic surgery due to early onset, prolonged motor and sensory block, lack of hemodynamics variability, and sustained postoperative analgesia. They tested and compared a combination of ropivacaine and dexmedetomidine versus ropivacaine alone (18). The administration of epidural steroid had historical roots due to various indications; thus, currently, it is performed under the fluoroscopic guide. Several approaches have been applied over years for such injections (19). These results showed that tramadol is not considered as neurotoxic when administered around the nerve sheet. Imani et al. found that addition of tramadol to 2% lidocaine in epidural anesthesia for cesarean sections can increase sensory and motor blockade effects without any attenuation of side effects and therefore, we know it as a proper drug (20).
Another study et al. showed no significant difference between bupivacaine, bupivacaine and morphine, and bupivacaine and dexmedetomidine regarding pain improvement based on postoperative VAS. However, bupivacaine and dexmedetomidine are alternatively used for pain control (21). Elhakim et al. demonstrated that bupivacaine and dexmedetomidine had significantly better results than bupivacaine alone (22). Accordingly, the assessment of ABG results showed that bupivacaine and dexmedetomidine in relation to bupivacaine had better results in the second to fourth days. Bupivacaine and dexmedetomidine could improve PaO2 compared to bupivacaine (22). Among various drugs used for epidural anesthesia, in the present study, we used bupivacaine and bupivacaine plus dexmedetomidine. Our results showed that bupivacaine can only relieve pain but bupivacaine plus dexmedetomidine could significantly reduce VAS scores in patients with a rib fracture. Chatrath et al. suggested bupivacaine and dexmedetomidine could result in prolonged rapid sensory and motor block and patients had a longer duration of the painless period, in line with other studies (23).
We demonstrated a good profile for dexmedetomidine combined with LA in traumatic patients and we can suggest it as an alternative drug for opioids. In future, other clinical trials should be conducted for obtaining definite profiles.
4.1. Conclusion
The present study suggested epidural infusion of bupivacaine and dexmedetomidine can excellently control the pain of fractured rib in traumatic patients without remarkable hemodynamics or pulmonary side effects, and it is a good alternative for bupivacaine in these patients.