1. Background
Chronic plantar heel pain (CPHP) is one of the common orthopedic diseases in elderly and adults. The prevalence of CPHP has been reported 24% in over 18 year-old adults and 42% in people over 65. CPHP could result in decrease of activity, walking disorders and disrupting daily tasks, as well as cause a sort of morbidity (1, 2). Chronic plantar heel pain is a general term and is defined as a deep pain beneath the heel and medial foot during walking and weight bearing, which would be intensified during the rest. Plantar fasciitis is one the main reasons of CPHP, however, the main reason of the pain is not clear in many of the cases and its ethology is still unknown (3). As one of the most common CPHP pains, plantar fasciitis is the reason for 11% -15% of CPHP in patients referring to orthopedic clinics, which dual distribution is among sportsmen and elderly and adults.
Degenerative changes in fascia can be seen, especially in non-inflammatory chronic cases (3). Etiology of plantar fasciitis has not been discovered yet and is probable multifactorial. Primary treatments for plantar fasciitis are conservative and include rest, non-steroidal anti-inflammatory drugs (NSAIDs), Achill tendon stretching of the plantar fascia, physical therapy, Plantar foot padding, and orthotic devices, which can be used to suit patient needs (4, 5). In the absence of therapeutic response with conservative treatment, other options for plantar fasciitis treatment include local steroid injections, platelet rich plasma, and intra lesion botulinum toxin A (5-7), which is one of the most popular treatments for corticosteroid injections (8).
Limited data from case-control studies emphasized the relationship between obesity and CPHP (9). The aim of this study is to investigate the relationship between anthropometric findings with results of chronic plantar heel pain treatment with corticosteroid local injection based on the BMI and anthropometric findings of the patients.
2. Methods
All the patients who were older than 18, who referred to orthopedic clinic with CPHP complaints from Aug 2014 to May 2016, and whose number amounted to 85 non-athletes patients were entered into a prospective cohort study. Patients of both genders, older than 18 years of age, referred to our orthopedic clinic, with definitive diagnosed, with chronic plantar heel pain (CPHP), who failed to respond to conservative treatments, including physical therapy, NSAIDs, Achilles stretching, plantar fascia exercise, and heel cushion for more than 2 months were included. Those meeting the inclusion criteria were invited to participate and provided informed consent.
Inclusion criteria were having chronic plantar heel pain for more than 2 month, no systemic disease (diabetes or any other metabolic or rheumatoid arthritis, gout, lupus), no congenital deformity in foot bone or history of fracture or surgery in ankle and foot, and no pregnancy in women.
A definitive diagnosis for CPHP is given with used criteria including: 1. tenderness to pressure at the origin of the plantar fascia on the medial tubercle of the calcaneus, 2. complaint of heel pain in the morning or after sitting for a long time, and 3. increasing foot pain with extended walking or standing for more than 15 minutes with pain intensity greater than or equal to 3 on a 1 - 10 visual analog scale (VAS) (10). Patients with posterior heel pain due to Achilles tendon bursitis, or active S1 radiculopathy were excluded. Also, patients who had a history of local or systemic corticosteroid injections or physiotherapy in the last 3 months were excluded from the study.
The mentioned patients were treated by anti-inflammatory drugs (celecoxibe 200 mg), Achilles stretching, and foot padding for 2 months. If they did not improve, they received local corticosteroid injection. Their demographic information was recorded and then their BMI was determined. After signing a written consent by the patients, their height, weight, and waist circumference were clinically examined. Their height by a wall tape measure with accuracy of 0.1 cm and weight by a SECA weighing machine [SECA Medical, Massachusetts, USA] with accuracy of 0.5 kg. Then their BMI was calculated in kg/m2. The extent of their morning and daily pain was recorded before the treatment. After 2 months of treatment, the results were also investigated among the patients. All the patients were treated with a 2-week oral medication including NSAIDs and stretching of the plantar fascia. After 2 months, if they did not improve or their pain did not decrease, they were considered as a candid of corticosteroid local injection. All the studied patients at least received 1 corticosteroid injection. For this purpose, 40 mg of Methylprednisolone plus and 1 - 1.5 cc of Lidocaine1% were used. For injection, a small needle (gauge 22) was entered in plantar region of the heel from the medial region and after touching the calcaneus bone. The injection carried in maximum tenderness in fascia region (9). Finally, the patients were followed up for 12 months. During the study, 5 patients were excluded due to lack of reference or follow-up. Lateral foot radiography was done to evaluate heel spur.
To investigate the pain severity, visual analog scale was used, in which the patients scored their pain from 1 to 10. To examine the performance of the patients, and evaluate the response to the treatment, The foot function index (FFI) is a self-report, foot-specific instrument, measuring pain and disability, and has been widely used to measure foot health. Foot Function index (FFI) questionnaire was used, which included 17 items concerning the level of pain and function and convenience in walking. The questions were asked by a doctor and the questionnaire was filled up at the end of 2 months after corticosteroid injection (9). The recurrence of symptoms was evaluated in 12 months of the follow up period. Finally the patients were classified according to their BMI in the following order (1):
Underweight BMI ≤ 18.5 kg/m2
Ideal weight: 18.5 - 24.9 kg/m2
Overweight: 24 - 29.9 kg/m2
Obese ≥ 30 kg/m2
Among the investigated 80 patients, 1 case was underweight, 18 cases were in ideal weight range, 25 patients were over weight, and 36 cases were obese. As the patients were analyzed based on their BMI, 1 underweight case was merged with the ideal weight group and the investigations were carried out on 3 groups of patients including ideal weight, over weight, and obese.
2.1. Statistical Analysis
Statistical analysis was done using the statistical package SPSS 16 (IBM, New York, USA). The data is shown as Mean ± SD with 95% confidence interval. Normality of the distribution was checked for each variable (1 sample Kolmogorov-Smirnov test). To compare the qualitative data among the 3 groups of patients, Chi-square or Fisher’s exact tests were employed. For comparing the quantitative data among the 3 groups based on the patients’ BMI, ANOVA and Scheffe Post Hoc were applied. Pearson correlation test was used to investigate the relationship between BMI and the pain and functional score of the patients. The significance level was P < 0.05.
3. Results
In this study, 80 CPHP patients, including 16 men (20%) and 64 women (80%), were studied. The patients’ average age was 46.3 ± 11.4 years old. The patients were classified into e groups based on their BMI.
Demographic findings of the patients can be seen in Table 1. Clearly there were significant differences in weight and waist circumference between the 3 groups (P < 0.001). The average age of the obese patients was significantly higher (P = 0.005).
| Variable | Ideal Weight | Over Weight | Obese | P Value |
|---|---|---|---|---|
| Men | 7 (36.8) | 6 (24%) | 3 (8.3%) | 0.3 |
| Women | 12 (63.2%) | 19 (76%) | 33 (91.7%) | |
| Age (year) | 40.3 ± 12.2 | 44.9 ± 10.9 | 50.3 ± 9.8 | 0.005a |
| Height (cm) | 165.4 ± 8.9 | 164.3 ± 9.1 | 153.5 ± 7.8 | 0.2 |
| Weight (kg) | 62.05 ± 9.1 | 74.8 ± 9.4 | 87.1 ± 10.9 | < 0.001a |
| BMI | 22.5 ± 2.1 | 27.5 ± 1.4 | 33.2 ± 12.6 | < 0.001a |
| Waist circumference | 71.3 ± 7.3 | 83.6 ± 13.4 | 99.3 ± 10.7 | < 0.001a |
| Heel spur in foot profile graph | 13 (68.4%) | 9 (36%) | 24 (66.7%) | 0.03a |
| Bilateral | 7 (36.8%) | 14 (56%) | 21 (58.3%) | 0.02a |
| Unilateral | 12 (63.2%) | 11 (44%) | 15 (41.7%) |
aSignificant difference.
Severity of the pain and the average score of the morning pain are compared in term of patients’ BMI in Table 2. Also, the functional score of the patients after corticosteroid injection can be seen in this table. The decrease in average pain of the patients was not significantly different among the 3 groups, in spite of higher pain severity in obese patients. However, the average of morning pain severity in obese patients was significantly different with the other groups (P = 0.005). Functional scores of the patients, according to the questionnaires, were not significantly different in the 3 groups. The number of injections was higher in obese patients and they needed more than 1 injection in most of the cases (P = 0.001).
| Variable | Ideal Weight Patient (N = 19) | Over Weight Patients (N = 25) | Obese Patients (N = 36) | P Value |
|---|---|---|---|---|
| VAS score before | 9.3 ± 0.6 | 9.2 ± 0.7 | 9.3 ±0.6 | 0.1 |
| VAS score after | 5.3 ±1.1 | 5.1 ±1.2 | 5,8 ±1.5 | 0.4 |
| Morning VAS before | 8.6 ±0.8 | 8,6 ±0.8 | 9.02 ±0.7 | 0.1 |
| Morning VAS after | 5.6 ±1.7 | 5.9 ±1.6 | 6.6 ±1.2 | 0.005a |
| FFI score | 58.1 ±12.6 | 61.3 ±8.9 | 60.6 ±9.7 | 0.5 |
| Number of injections | 1.1 ±0.2 | 1.2 ±0.2 | 1.6 ±0.4 | 0.001a |
Abbreviations: FFI, foot functional index; VAS, visual analog scale.
aSignificant difference.
In the long-term follow-up the patients for at least 12 months, the recurring cases were determined. In 1 case (5.3%) in the ideal weight group, recurrence happened. Also, in overweight patients, 3 of them (12%) experienced recurrence after the last injection, while this record was 21 cases (58.3%) in the obese patients’ group, who were generally resistance against corticosteroid. There was significant difference between the 3 groups in the recurrence rate in obese patients (P < 0.001). According to the regression model, obesity can be a relative risk factor (OR = 7.52, 95% CI = 4.28 to 16.53, P < 0.001) in CPHP recurrence.
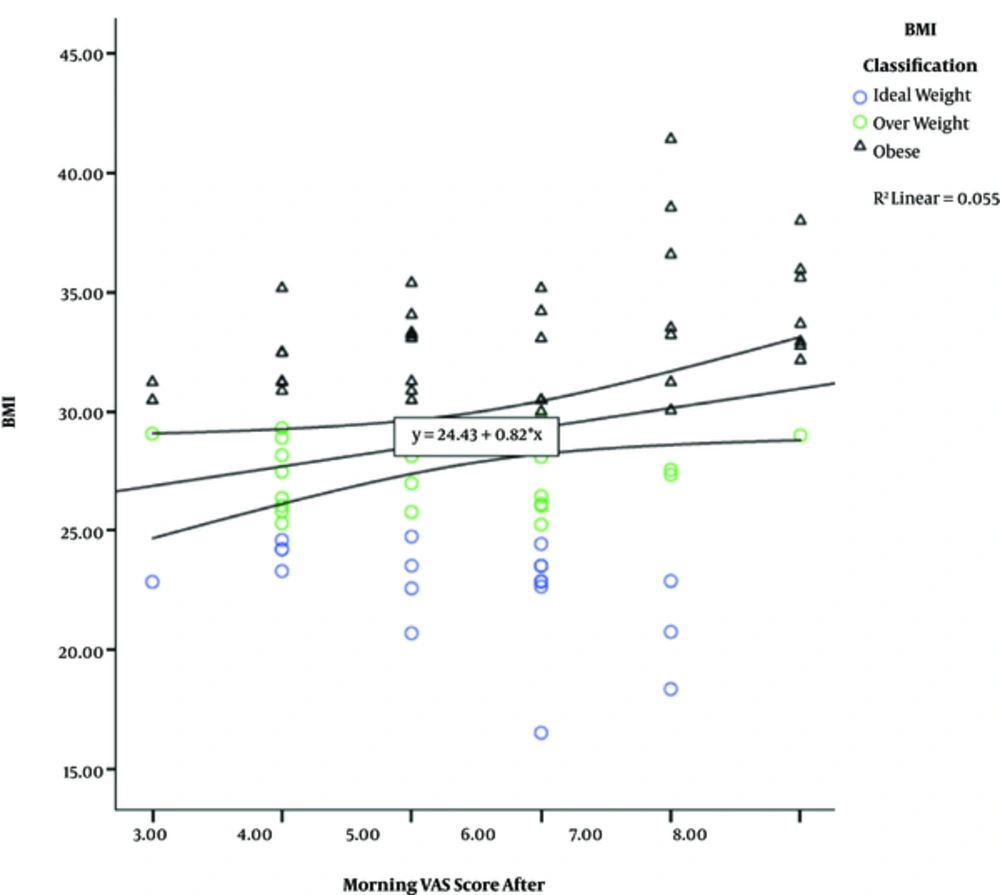
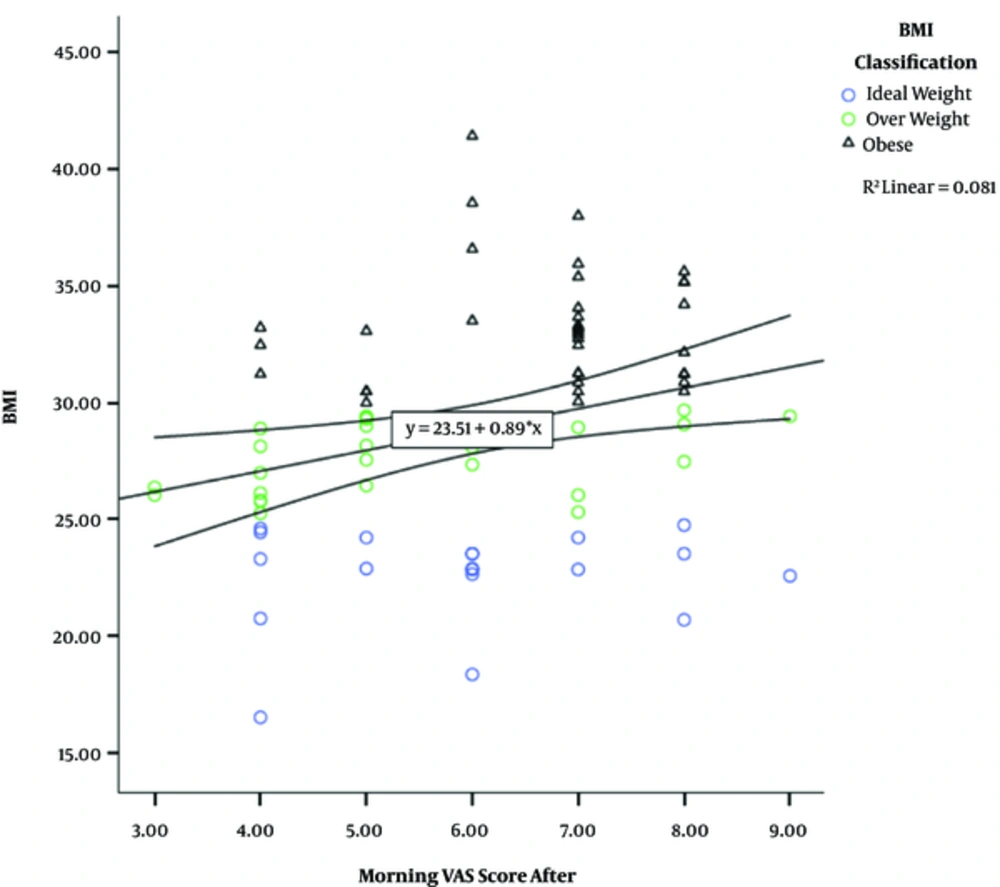
According to Pearson correlation test, there was a positive statistical relationship between the BMI and average pain of the patients after injection as well as the average of morning pain with r = 0.1, P = 0.03 and r = 0.2 and P = 0.005, respectively (Figures 1 and 2).
4. Discussion
The aim of this study is to investigate the relationship between the people’s BMI and their response to CPHP treatment. The etiology of Plantar Fasciitis has not been discovered yet and it is probably multifactorial (11). Limited data of case-control studies have mentioned risk factors such as obesity, jobs requiring long time standing (pes planus), ankle dorsiflexion, and inferior calcaneal exostosis (9, 11). As this disease is common in runners, it is also believed that plantar fasciitis can be mainly due to micro-trauma. Proposed risk factors include too much running (or sudden increase in running distance), improper shoes for running, running on rough surfaces, or having foots with high arch, and short Achilles tendon; however, the evidence for most of these factors is limited or unavailable. Long-term follow-up in large series, which mainly include the patients referring to orthopedic clinics showed that the clinical trend is acceptable in most of Plantar fasciitis patients and the symptoms would be improved in more than 80% of patients during 12 months (10, 11). While, according to the data of our study, obese patients are more exposed to symptom recurrence and majority of these patients had bilateral involvement.
The relationship between the increase of BMI and Chronic plantar heel pain has been mentioned in various resources and the studies on ordinary, non-sportsmen population indicated strong correlation between increase of BMI and CPHP (12, 13). However, there is no study addressing the relationship between the obesity and response to the treatment. According to the findings of our study, there was no significant difference in the patients’ response to treatment in different groups. Although obese patients had more severe morning pain, their FFI was not significantly different. One of the interesting points of our study was the presence of significant difference in the age of the patients in 3 groups. Obese patients were older than patients with ideal weight, which could be due to the extent of their activity. The chronic pain of the people with ideal weight could be due to their higher activity, however, the CPHP in obese people with higher age and lower activity could be attributed to their weight. Old women with high weight are more prone to CPHP, in a way that in the cohort study of Gay et al., high BMI in old women was considered as a strong risk factor for chronic pain of the ankle (14). As mentioned before, various etiologies have been introduced, however, all the patients had a common complaint, the chronic plantar heel pain with the same treatment, which is one of the characteristics of our study. The study of Irving et al., was conducted in 2007 in Australia and addressed the relationship between BMI and CPHP (1) in patients with chronic heel pain, BMI was significantly higher. Based on logistic multi-variant analysis, high BMI was the most important factor in CPHP and was mentioned as a strong risk factor (1). Study of Chattereton was carried out in England in 2005 and was an epidemiological investigation of CPHP in society. In this study, 9334 people older than 50 were examined (2). The findings of this study showed that BMI with the relative risk of 1.5 was the most important factor in chronic pain, in bilateral cases, there was a strong correlation between BMI and chronic pain, and in the mentioned cases, the relative risk was reported 5.7 (2). Diabetes is the 2nd factor in CPHP and had a relative risk of 1.9. High physical activity had negative relationship with creation of chronic plantar heel pain. Moreover, BMI > 35 had a relative risk of 7.1, which reflects the impact of BMI in increase of CPHP prevalence (2). In our study, bilateral involvement was more frequent in obese patients, however, their response to the treatment was the same as patients with ideal weight, and the severity of morning pain was higher in obese patients. Recurrence is also more in obese patients. These people are more prone to recurrence and in more than 50% of the cases, recurrence happened during the follow-up period. Also, the number of corticosteroid injection was more in these people. It seems that the response of obese people to the treatment is the same among all groups; however, after anti-inflammatory effects of corticosteroid, recurrence happened in obese patients. In a study by Mc Milan et al., increase of plantar fascia to more than 2.1 mm has a strong relationship with CPHP and observance of spur in radiography was more frequent in CPHP patients (15). This increase of thickness had a significant relationship with BMI in a way that thicknesses over 4 mm were reported for BMI > 30. According to this study, increase of fascia was the result of weight increase (15). Therefore, one of the reasons of recurrence in obese people could be due to etiology of plantar fascia thickness increase, which by fading of corticosteroid, effects resulted in recurrence of the symptoms. In our study, only conservative treatments with corticosteroid injection were investigated. Other therapeutic methods of CPHP such as chock therapy should be considered as well.
4.1. Conclusion
High BMI is a strong risk factor in recurrence of chronic plantar heel pain. Obese patients require more frequent corticosteroid injections and there is a strong relationship between patients’ BMI and the severity of morning pains.