1. Background
Perioperative inadvertent hypothermia (PIH) is defined as a 2°C decrease in core body temperature, resulting in a temperature of 36°C, which commonly occurs after major surgical procedures under local or general anesthesia due to bleeding and hypotension (1). It is a critical issue, especially in the elderly and high-risk patients, as it negatively affects multiple organs, induces shivering, hypoperfusion, and peripheral vasoconstriction, weakens tissue oxygenation, increases the risk of organ failure, impairs neutrophil function, and has many other negative effects (2, 3). Moreover, PIH is associated with adverse postoperative outcomes, including wound infection, prolonged hospitalization period, increased surgical bleeding, increased risk of morbid cardiac events, and postoperative ventricular tachycardia (4-6).
Various factors have been proposed to associate with predict hypothermia, such as higher age, female gender, ASA physical status of the patient, type of surgery, and the anesthetic technique (7, 8). Accordingly, fentanyl, but not morphine or bupivacaine, was associated with postoperative hypothermia in neonates, which is hypothesized to be due to metabolic heat production block (9).
Despite the significance of PIH, the European survey shows that preoperative warming of patients is not a standard care and no guideline has been provided in this regard (10). Various techniques have been used for warming of patients undergoing surgery; some studies have investigated the effect of skin warming (11) while others have evaluated the ambient warming during or before surgery (12, 13) and some have used a combination of both methods (14).
As there is no guideline regarding the most appropriate temperature of the warmer, duration of warming patients, and other details, the present study aimed to compare the physical and laboratory outcomes in patients undergoing total intravenous anesthesia in posterior spinal fusion surgery, warmed intra-operatively at two different temperatures.
2. Methods
2.1. Subjects and Procedure
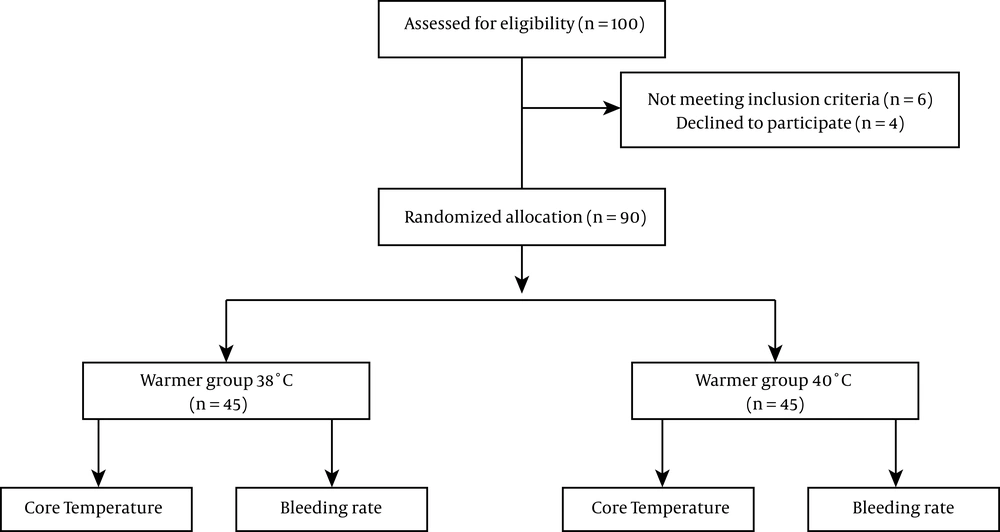
This randomized controlled trial was carried out at the Tehran Pars Hospital, Iran (a single center study) from July 2015 to May 2016. The trial was approved by the Ethics Committee of Iran University of Medical Sciences (Number: IRCT20141225020434N2). The participants signed the informed consent form after being explained about the study objectives. The present study investigated 90 patients undergoing total intravenous anesthesia in posterior spinal fusion surgery (PSF) (Figure 1) who were recruited in the study by a convenient sampling method. The inclusion criteria were to include patients referring to Pars hospital from July 2015 to May 2016 and aged between 30 and 60 years, patients without underlying diseases, including endocrine, cardiovascular, respiratory, hepatorenal, and hematologic diseases, non-smokers, and non-addict patients with a risk of surgery grade 1 or 2. Any patient with hypothermia or fever was excluded from the study. The patients who met the inclusion/exclusion criteria were randomly divided into two groups of 45 patients, based on the codes on concealed packets. The warmer (WarmTouchTM, CovidienTM, USA) was set at 38°C for group “A” during surgery and at 40°C for group “B.” The anesthesia protocol for both groups consisted of premedication with 0.05 mg/kg midazolam and induction by 5 mg/kg thiopental sodium, 0.3 mg/kg atracurium, and 100% oxygen that was maintained by 100 µg/kg protocol and 0.1 µg/kg remifentanil with two oxygenations. Respiratory oxygen was kept at 50% during surgery and breathing was controlled by the respiratory system with a tidal volume of 8 mL/kg and a respiratory rate of 12 per minute. Mean blood pressure was kept at 65 - 70 mmHg during surgery. If more than 2 points of shivering occurred, 25 mg of meperidine would be administered intravenously. Core temperature (Tc) was measured indirectly with the tympanic measurement of temperature (by used WarmTouch). Hypothermia was defined as the temperature below 36°C based on the National Institute for Clinical Excellence.
The number of bloody gauze during operation and the levels of hemoglobin and hematocrit during the operation were evaluated and compared with the preoperative values.
2.2. Study Outcomes
The primary outcome measured was Tc. Other outcomes of interest included oxygen saturation, CO2 level, electrocardiographic changes, systolic BP, mean Tc (recorded every 30 minutes), and serum levels of platelet counts (PLT), hemoglobin (Hb), and hematocrit (Hct), arterial blood gas (ABG) parameters, heart rate, and respiratory rate. Patient’s characteristics, including age, sex, weight, and body mass index (BMI), were also recorded. All tests and examinations were recorded in three phases: during induction, during operation, and before discharge from the recovery room. Normal ranges of all the variables measured are defined in Table 1.
| Variable | Normal Range | Total Patientsa | Group Aa | Group Ba | P Value |
|---|---|---|---|---|---|
| Hemoglobin, mg/dL | Male: 13.5 to 17.5, female: 12.0 to 15.5 | 13.80 ± 1.62 | 12.48 ± 2.09 | 11.87 ± 1.61 | 0.005 |
| Hematocrit, % | Male: 42 to 54, female: 38 to 46 | 41.34 ± 4.80 | 37.79 ± 6.26 | 35.88 ± 4.93 | 0.004 |
| Fasting blood sugar, mg/dL | < 100 | 100.15 ± 20.16 | 116.76 ± 35.39 | 118.81 ±32.75 | 0.0001 |
| Creatinine, mg/dL | 0.6 - 1.2 | 1.04 ± 1.02 | 1.15 ± 1.00 | 1.19 ± 0.95 | 0.251 |
| Sodium, mEq/L | 135 - 145 | 148.03 ± 92.96 | 137.67 ± 13.94 | 140.58 ± 2.41 | 0.150 |
| Potassium, mEq/L | 3.5 - 5.0 | 6.44 ± 2.71 | 3.76 ± 0.44 | 4.11 ± 3.57 | 0.124 |
| BUN, mg/dL | 7 - 20 | 14.02 ± 3.73 | 16.25 ± 4.02 | 16.55 ± 4.52 | 0.524 |
| Heart rate, /min | 60 - 100 | 78.25 ± 9.96 | 75.97 ± 12.23 | 73.11 ± 12.07 | 0.009 |
| Systolic blood pressure, mmHg | 80 - 120 | 103.96 ± 17.14 | 79.82 ± 9.82 | 81.96 ± 9.83 | 0.104 |
| Body temperature, °C | > 36 | 35.99 ± 0.70 | 36.31 ± 0.46 | 36.39 ± 0.17 | 0.212 |
| Operating theater temperature, °C | 23 - 25 | 24.40 ± 18.97 | 23.45 ± 1.48 | 23.66 ± 1.59 | 0.340 |
| Respiratory rate, /min | 12 - 20 | 12.29 ± 0.71 | 12.24 ± 0.69 | 12.34 ± 0.79 | 0.390 |
| Arterial Oxygen, % | 80 - 100 | 94.93 ± 1.01 | 98.76 ± 6.63 | 99.51 ± 1.13 | 0.067 |
| Arterial carbon dioxide, mmHg | 35 - 45 | 28.50 ± 0.70 | 30.28 ± 2.89 | 28.94 ± 4.52 | 0.354 |
| Arterial lactate, mmol/L | 0.5 - 1 | 0.75 ± 0.21 | 1.26 ± 0.71 | 1.20 ± 0.56 | 0.354 |
aValues are expressed as mean ± SD.
2.3. Statistical Analysis
Statistical analysis was performed using SPSS version 19 software (SPSS Inc., Chicago, IL, USA). Baseline characteristics between the two groups were compared using the Student’s-test or the Mann-Whitney test whenever the data did not appear to have a normal distribution or when the assumption of equal variances was violated across the study groups. The data are presented as numbers (percentages) for categorical variables or means ± standard deviation (SD) for quantitative variables. P values of less than 0.05 were considered statistically significant.
3. Results
The mean age of the patients was 50.14 ± 13.38 years, which was significantly higher in group “B” (the group with 40°C warmer) (55.40 ± 11.45 years) than group “A” (the group with 38°C warmer) (47.76 ± 14.58 years) (P = 0.042). The mean height and weight of the two groups were not significantly different (P = 0.397 and 0.987, respectively). The patients’ characteristics are compared between the two groups in Table 1. The mean time of operation was 6.34 ± 2.26 hours and the amount of intraoperative bleeding was estimated to be 1788 ± 123 mL.
The comparison of the two groups before intervention (Table 1) showed significantly higher serum hemoglobin and hematocrit levels, as well as lower fasting blood sugar, in group A than in group B, while the rest of the variables did not differ significantly between the two groups before intervention. As shown in Table 2, no difference was found in any study hemodynamic and biochemical parameters between the two groups during operation; however, postoperatively, group B had a lower serum hemoglobin level and higher sodium level with no difference in other indices. In addition, base excess was significantly different between the groups during operation and recovery. We found no significant change in body temperature, as well as clinical and biochemical parameters, among the three time points of during anesthesia induction, during operation, and during recovery (Table 3).
| Variable | During Induction | During Operation | During Recovery | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Group A | Group B | P Value | Group A | Group B | P Value | Group A | Group B | P Value | |
| Hemoglobin, mg/dL | 12.84 ± 2.21 | 12.08 ± 1.73 | 0.042 | 11.64 ± 1.97 | 11.15 ± 1.71 | 0.160 | 12.77 ± 1.67 | 12.06 ± 1.20 | 0.047 |
| Hematocrit, % | 39.18 ± 6.30 | 36.74 ± 5.06 | 0.025 | 36.31 ± 6.49 | 33.92 ± 5.44 | 0.144 | 38.33 ± 5.32 | 36.28 ± 3.74 | 0.127 |
| Fasting blood sugar, mg/dL | 95.89 ± 35.02 | 100.54 ± 21.29 | 0.558 | 116.28 ± 29.67 | 118.52 ± 28.58 | 0.775 | 139.27 ± 29.02 | 141.39 ± 35.43 | 0.828 |
| Sodium, mEq/L | 134.34 ± 23.23 | 140.31 ± 2.01 | 0.343 | 139.41 ± 2.50 | 140.33 ± 2.21 | 0.857 | 139.68 ± 2.62 | 141.14 ± 2.98 | 0.031 |
| Potassium, mEq/L | 3.48 ± 0.34 | 4.55 ± 6.01 | 0.056 | 3.80 ± 0.35 | 3.83 ± 0.64 | 0.216 | 4.100 ± 0.48 | 3.93 ± 2.95 | 0.326 |
| Heart rate, /min | 74.51 ± 11.42 | 70.71 ± 9.57 | 0.337 | 76.20 ± 11.13 | 73.58 ± 11.47 | 0.165 | 80.83 ± 12.57 | 77.21 ± 11.17 | 0.297 |
| Systolic blood pressure, mmHg | 12.08 ± 1.54 | 16.79 ± 2.26 | 0.897 | 76.23 ± 6.73 | 77.96 ± 7.24 | 0.050 | 87.88 ± 11.55 | 89.72 ± 8.95 | 0.053 |
| Body temperature, °C | 36.23 ± 0.37 | 36.25 ± 0.12 | 0.752 | 36.33 ± 0.57 | 36.45 ± 0.24 | 0.211 | 36.45 ± 0.14 | 36.51 ± 0.07 | 0.357 |
| Operating theater temperature, °C | 22.27 ± 0.19 | 22.65 ± 0.53 | 0.545 | 22.97 ± 0.59 | 22.95 ± 0.53 | 0.999 | 25.54 ± 1.20 | 25.84 ± 0.92 | 0.788 |
| Respiratory rate, /min | 11.85 ± 0.33 | 12.00 ± 0.43 | 0.221 | 11.95 ± 0.23 | 12.00 ± 0.00 | 0.489 | 12.82 ± 1.00 | 12.90 ± 1.09 | 0.243 |
| Oxygen, % | 0.41 ± 0.07 | 0.90 ± 0.27 | 0.011 | 99.78 ± 0.57 | 100.00 ± 0.00 | 0.440 | 96.13 ± 12.01 | 98.92 ± 1.16 | 0.368 |
| CO2, % | 2.97 ± 0.38 | 2.96 ± 0.40 | 0.152 | 29.50 ± 3.49 | 28.45 ± 5.13 | 0.625 | 32.17 ± 2.71 | 30.67 ± 3.24 | 0.480 |
| Lactate, mg/dL | 0.41 ± 0.07 | 0.37 ± 0.07 | 0.897 | 1.09 ± 0.41 | 1.09 ± 0.48 | 0.967 | 1.74 ± 0.99 | 1.57 ± 0.68 | 0.280 |
| pH | 0.05 ± 0.007 | 0.05 ± 0.006 | 0.0001 | 7.39 ± 0.06 | 7.41 ± 0.06 | 0.524 | 7.38 ± 0.07 | 7.37 ± 0.06 | 0.969 |
| PaCO2, mmHg | 5.18 ± 0.66 | 4.13 ± 0.55 | 0.135 | 31.21 ± 5.53 | 29.84 ± 7.49 | 0.103 | 34.88 ± 4.90 | 42.28 ± 32.82 | 0.936 |
| PaO2, mmHg | 67.70 ± 8.74 | 72.57 ± 9.78 | 0.316 | 274.74 ± 77.74 | 259.20 ± 95.94 | 0.883 | 224.76 ± 63.34 | 225.50 ± 73.20 | 0.291 |
| HCO2, mEq/L | 3.43 ± 0.44 | 3.44 ± 0.46 | 0.011 | 19.58 ± 2.28 | 19.60 ± 2.10 | 0.658 | 19.50 ± 1.95 | 19.61 ± 6.08 | 0.152 |
| Base excess | 19.13 ± 3.61 | 2.67 ± 0.52 | 0.729 | -4.45 ± 2.39 | -4.01 ± 2.67 | 0.025 | -4.84 ± 2.08 | -0.25 ± 0.99 | 0.042 |
| Oxygen saturation, % | 0.25 ± 0.04 | 1.37 ± 0.27 | 0.343 | 99.83 ± 0.53 | 100.00 ± 0.00 | 0.783 | 99.08 ± 1.15 | 91.42 ± 26.27 | 0.476 |
| Lactate, mg/dL | 0.43 ± 0.08 | 0.34 ± 0.06 | 0.387 | 1.08 ± 0.40 | 1.10 ± 0.48 | 0.524 | 1.71 ± 0.95 | 34.84 ± 2.94 | 0.619 |
| Urine output, mL | 115.84 ± 25.24 | 325.70 ± 69.44 | 0.364 | 881.25 ± 503.21 | 816.20 ± 519.03 | 0.976 | 1692.50 ± 567.60 | 1275.00 ± 613.73 | 0.751 |
| Variable | During Induction | During Operation | During Recovery | P Value |
|---|---|---|---|---|
| Body temperature, °C | ||||
| Group A | 36.23 ± 0.37 | 36.33 ± 0.57 | 36.45 ± 0.14 | 0.059 |
| Group B | 36.25 ± 0.12 | 36.45 ± 0.24 | 36.51 ± 0.07 | 0.181 |
| Hemoglobin, mg/dL | ||||
| Group A | 12.84 ± 2.21 | 11.64 ± 1.97 | 12.77 ± 1.67 | 0.245 |
| Group B | 12.08 ± 1.73 | 11.15 ± 1.71 | 12.06 ± 1.20 | 0.584 |
| Hematocrit, % | ||||
| Group A | 39.18 ± 6.30 | 36.31 ± 6.49 | 38.33 ± 5.32 | 0.054 |
| Group B | 36.74 ± 5.06 | 33.92 ± 5.44 | 36.28 ± 3.74 | 0.368 |
| Fasting blood sugar, mg/dL | ||||
| Group A | 95.89 ± 35.02 | 116.28 ± 29.67 | 139.27 ± 29.02 | 0.159 |
| Group B | 100.54 ± 21.29 | 118.52 ± 28.58 | 141.39 ± 35.43 | 0.897 |
| Sodium, mEq/L | ||||
| Group A | 134.34 ± 23.23 | 139.41 ± 2.50 | 139.68 ± 2.62 | 0.589 |
| Group B | 140.31 ± 2.01 | 140.33 ± 2.21 | 141.14 ± 2.98 | 0.525 |
| Potassium, mEq/L | ||||
| Group A | 3.48 ± 0.34 | 3.80 ± 0.35 | 4.100 ± 0.48 | 0.250 |
| Group B | 4.55 ± 6.01 | 3.83 ± 0.64 | 3.93 ± 2.95 | 0.987 |
| Heart rate, /min | ||||
| Group A | 74.51 ± 11.42 | 76.20 ± 11.13 | 80.83 ± 12.57 | 0.123 |
| Group B | 70.71 ± 9.57 | 73.58 ± 11.47 | 77.21 ± 11.17 | 0.589 |
| Operating theater temperature, °C | ||||
| Group A | 22.27 ± 0.19 | 22.97 ± 0.59 | 25.54 ± 1.20 | 0.879 |
| Group B | 22.65 ± 0.53 | 22.95 ± 0.53 | 25.84 ± 0.92 | 0.650 |
| Respiratory rate, /min | ||||
| Group A | 11.85 ± 0.33 | 11.95 ± 0.23 | 12.82 ± 1.00 | 0.361 |
| Group B | 12.00 ± 0.43 | 12.00 ± 0.00 | 12.90 ± 1.09 | 0.054 |
| CO2, % | ||||
| Group A | 2.97 ± 0.38 | 29.50 ± 3.49 | 32.17 ± 2.71 | 0.945 |
| Group B | 2.96 ± 0.40 | 28.45 ± 5.13 | 30.67 ± 3.24 | 0.251 |
| Lactate, mg/dL | ||||
| Group A | 0.41 ± 0.07 | 1.09 ± 0.41 | 1.74 ± 0.99 | 0.361 |
| Group B | 0.37 ± 0.07 | 1.09 ± 0.48 | 1.57 ± 0.68 | 0.213 |
| PaCO2, mmHg | ||||
| Group A | 5.18 ± 0.66 | 31.21 ± 5.53 | 34.88 ± 4.90 | 0.547 |
| Group B | 4.13 ± 0.55 | 29.84 ± 7.49 | 42.28 ± 32.82 | 0.586 |
| PaO2, mmHg | ||||
| Group A | 67.70 ± 8.74 | 274.74 ± 77.74 | 224.76 ± 63.34 | 0.874 |
| Group B | 72.57 ± 9.78 | 259.20 ± 95.94 | 225.50 ± 73.20 | 0.251 |
| HCO3, mEq/L | ||||
| Group A | 3.43 ± 0.44 | 19.58 ± 2.28 | 19.50 ± 1.95 | 0.158 |
| Group B | 3.44 ± 0.46 | 19.60 ± 2.10 | 19.61 ± 6.08 | 0.259 |
| Base excess | ||||
| Group A | 3.13 ± 3.61 | -4.45 ± 2.39 | -4.84 ± 2.08 | 0.035 |
| Group B | 2.67 ± 0.52 | -4.01 ± 2.67 | -0.25 ± 0.99 | 0.015 |
| Urine output, mL | ||||
| Group A | 115.84 ± 25.24 | 881.25 ± 503.21 | 1692.50 ± 567.60 | 0.875 |
| Group B | 325.70 ± 69.44 | 816.20 ± 519.03 | 1275.00 ± 613.73 | 0.695 |
According to the Pearson’s correlation test, the patients’ heart rate was positively associated with the temperature change in both groups (r = 0.22 and P < 0.05). The temperature change was negatively associated with serum hemoglobin and hematocrit levels in group “A” (r = -0.21 and P < 0.05) while it was directly associated with fasting blood sugar (r = 0.388, P < 0.01) and arterial lactate (r = 0.25, P < 0.05) in group B.
4. Discussion
According to the results of the present study, there was no significant difference between the Tc of patients warmed intra-operatively at 38°C or 40°C; however, the prevalence of hypothermic patients decreased in group B receiving the 40°C warmer (P < 0.001). At the end of the recovery, 51% in group A and 49% in group B were hypothermic.
Several studies have investigated the efficacy of warming in patients undergoing different surgical procedures by using different warming methods. Murat and colleagues warmed 26 children undergoing spine surgery with forced-air warmers during the operation and measured the rectal temperature at the end of the surgery; they reported significantly increased Tc in the warmed group, compared to the control group (15). Andrzejowski and colleagues evaluated 68 patients undergoing spinal surgery under general anesthesia and reported a smaller intra-operative decrease in mean Tc and lower prevalence of PIH in 31 patients prewarmed at 38°C for 60 minutes, compared to 37 controls; they declared 60 minutes prewarming at 38°C is effective for preventing PIH (13). Kurz and colleagues randomized patients undergoing the colorectal surgery into the control and warmed groups (using 37°C air-forced warmer), reporting a significant difference in Tc at the end of surgery until 5 hours after the surgery (6). However, the results of the present study indicated no significant increase in Tc after warming patients, either at 38°C or at 40°C, although the mean values did not drop below 36°C. The authors stand the point that these results can be justified as follows: the above-mentioned studies, which found a significant increase in Tc in the warmed group, measured Tc at the end of the surgery and the study by Andrzejowski et al. reported that the changes in Tc were not statistically significant after 80 minutes, which could justify the insignificant increase in Tc in the present study, as long as patients undergoing posterior spinal fusion surgery usually stay in the recovery room for more than one hour and we measured the final Tc at the end of their recovery room stay. In addition, as demonstrated in previous studies (6, 15), there is a minor decrease in Tc during surgery, even in the warmed group, which could justify the insignificant change in Tc during operation in the present study. Moreover, as posited, various factors can affect Tc, including the amount of fluid and blood replacement, duration of anesthesia and surgery, and the ambient operating room temperature (8), which could have variations among participants in the present study and might have affected the results.
Among studies that evaluated prewarming the patients, the optimal duration of warming patients was found to be 30 - 60 minutes (13, 16) while we warmed the patients throughout the posterior spinal fusion surgery that usually lasted for 2 - 3 hours and might induce some metabolic changes, such as increased base excess that was statistically significant in the current study. In addition, as studies have hypothesized, increased skin temperature and sweating interfere with the efficiency of warming (16) that might have also caused insignificant results in the present study.
Although the results of the present study determined no significant changes in other variables, the mean values were mostly within the normal ranges, clarifying the clinical significance of warming in patients undergoing surgical procedures. This means that hypothermia, cardiac arrhythmia, excessive bleeding, electrolyte imbalance, etc., reported by previous studies (due to hypothermia) (4-6), were not common findings in the present study and the warming intervention could correct such complications although considering the non-warmed control group in the present study could strengthen such conclusion. Besides, some of the variables, investigated in the present study, have established to be similar in warmed and control groups in other studies; Murat et al. found no difference in blood loss between warmed and control groups (15); Kurz et al. reported a similar oxygen consumption, fluid balance, and hemodynamic responses in the warmed and control groups (6). Overall, the results of the present study, consistent with previous studies, indicated the maintenance of normothermia during operation is of great importance and could prevent hypothermia-related perioperative complications. It seems that using newly designed fluid warming kits can turn the warming devices as safer. As shown by Jung et al. (17), a new kit named Mega Acer Kit was more effective in preventing excessive hypothermia and warming compared to the Standard Ranger. In addition, Yang et al. (18) applied two warming methods, namely warm cotton blankets and a radiant warmer, to hypothermia patients in a post-anesthetic care unit (PACU) after spinal surgery and showed that the radiant warmer was a more efficient device to reach a specified temperature.
The present study faced some strength and some limitations. One of the strengths of the present study was the comparison of warmers at two temperatures with a random allocation of patients, which has scarcely been conducted before. In addition, a wide range of variables was investigated in the current study to examine the effect of intra-operative warming on various parameters. Nevertheless, the lack of a non-warmed control group limited the clinical conclusions. In addition, several factors, which were not controlled in the present study, could act as confounding factors, including the amount of fluid and blood replacement and duration of anesthesia and surgery. Therefore, it is suggested that future studies consider the effect of different warmer temperatures in a multicentric study with a larger sample size and compare the results with the outcomes of a control group to minimize the effect of confounders.
4.1. Conclusion
Since the mean values of the variables in the present study were within the normal ranges, it could be said that warming the patients during operation caused normothermia in both groups, showing that there is no significant difference in warming the patients during operation at 38 or 40°C to prevent hypothermia-induced complications during induction, operation, and recovery.