1. Background
Cleft lip and palate (CLP) is one of the common congenital malformations worldwide. In the UK, its incidence is between 1:500 and 1:700, approximately 1000 babies every year presenting with cleft lip and/or palate. Children with CLP usually present for correction in infancy. Waiting until 3 months of age gives time to detect other congenital abnormalities and allows anatomical and physiological maturation. Upper respiratory tract infections (URTIs) are common at this age and carry an increased risk of airway complications and impaired wound healing (1).
Inhalant anesthesia has been the mainstay of pediatric anesthesia. However, with the advances in the understanding of pharmacology and the availability of new fast-acting drugs and the modern infusion pumps, total intravenous anesthesia (TIVA) has become an attractive option in the administration of general anesthesia in children. The TIVA usage compared with volatile anesthesia are still a matter of debate (1).
However, propofol TIVA became an attractive option in children (2). It allows a smoother recovery with less distress behavior, (3) reduced airway reactivity and improved postoperative ciliary function (4), and reduced nausea and vomiting (5).
2. Objectives
We aimed to compare propofol- vs. sevoflurane-based anesthesia for pediatrics undergoing cleft palate repair in emergence characteristics and respiratory adverse effects.
3. Methods
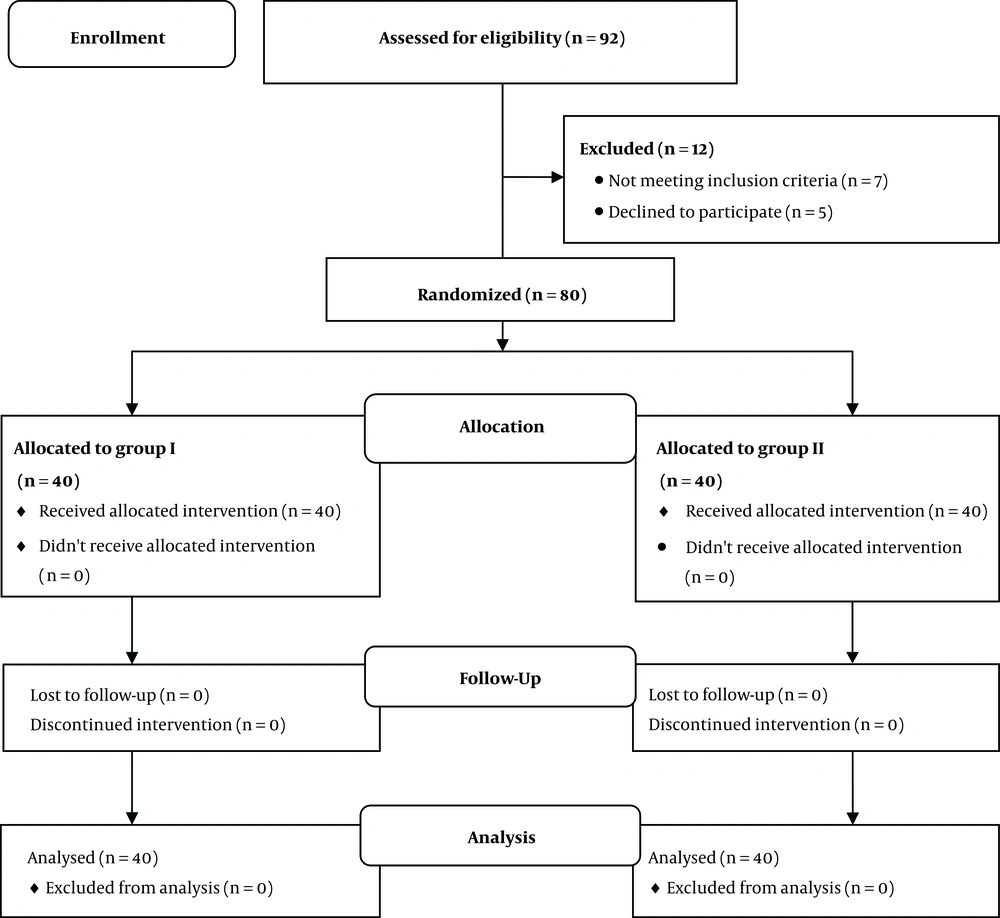
After obtaining approval and informed consent from each parent, 80 children, based on the American Society of Anesthesiologists physical status class (I and II), age six months to one year, from both genders scheduled to undergo cleft palate repair surgery, were selected and included in this prospective randomized study that was done at our pediatric hospital (Tanta University Hospital, Egypt) from June 2017 to April 2018. The trial was approved by Tanta Faculty of Medicine Research Ethics Committee with approval code of 31531/05/17 and registered at the Pan African Trial registry (identification number; PACTR201710002426237 at 2017/07/14).
The exclusion criteria were: children with the known severe cardiovascular disease, cerebral, hepatic illness, children with lower or upper respiratory tract infection; having purulent nasal discharge, fever, or with a cough, and those with renal dysfunction or neuromuscular diseases. Preanesthetic checkup and routine investigations were done for all children. The patients were kept nil by mouth for 4 hours for breast milk, 6 hours for milk formula, and 8 hours for solid food and 2 hours for clear fluid. Thirty minutes before the induction of anesthesia, all patients were pre-medicated with 0.5 mg/kg of oral midazolam.
Upon admitting to the operating room, peripheral venous access was obtained using a 22 G catheter and the pediment solution 10 mL/kg was infused with cefazolin 50 mg/kg for antibiotic prophylaxis. Non-invasive monitors, such as electrocardiogram, non-invasive blood pressure, oxygen saturation, and bispectral index (BIS) were attached for recording baseline parameters such as heart rate, mean arterial pressure, peripheral oxygen saturation, and the depth of anesthesia. The study was single-blind and the participants were randomly allocated to two groups: 40 patients each at 1:1 allocation ratio, using an on-line randomization program (www.randon.org).
Group I (40 patients): In this group, general anesthesia was induced with fentanyl one µg/kg, propofol 2.5 mg/kg, and after the loss of consciousness, the muscle was relaxed with cisatracurium 0.15 mg/kg intravenous. To prevent propofol injection pain, 0.1 mg/kg of lidocaine was added. The children were intubated with tracheal tubes. Maintenance of anesthesia was started immediately after the loading dose by a continuous infusion of propofol 9 mg/kg/hr and cisatracurium 3 µg/kg/hr by two syringe drivers. Group II (40 patients): In this group, general anesthesia was induced with O2/sevo (FiO2 = 1/sevoflurane, 8% MAC), fentanyl one µg/kg and after loss of consciousness, the muscle was relaxed with cisatracurium 0.15 mg/kg immediately. Then the maintenance of anesthesia was carried out by O2/air (FiO2 = 0.4), sevoflurane 2% MAC, and cisatracurium 3 µg/kg/hr.
In both groups, cisatracurium was given immediately when BIS value became between 40 - 60, lungs were mechanically ventilated in pressure-controlled mode. The pressure and frequency were adjusted to deliver adequate tidal volume and to maintain normocapnia (EtCO2 30 ± four mmHg). All children were received dexamethasone 0.1 mg/kg intraoperatively. The depth of anesthesia was assessed by BIS and hemodynamic parameters such as heart rate, blood pressure, lacrimation, and sweating. Following the skin incision or at any time during the procedure, an increased heart rate, mean blood pressure or BIS value more than 20% above the baseline was defined as the insufficient depth of anesthesia. All children received acetaminophen (40 mg/kg) rectally after the induction to ensure adequate analgesia after discharge.
All cases were operated by the same surgeon and at the end of the surgery, both types of anesthesia were switched off and the neuromuscular blockade was reversed by neostigmine (0.05 mg/kg) and atropine (0.02 mg/kg) slowly intravenously. The children were successfully extubated when the patients met the criteria of extubation (return of gag reflex, facial grimace, and purposeful motor movements) and transferred to the post-anesthesia care unit (PACU). In the PACU, they were observed closely to detect any complications or adverse events and discharged when Aldrete score ≥ 9. The routine analgesic intake started 6 hours after surgery with 30 mg/kg of rectal paracetamol and repeated every 8 hours up to 48 hours postoperatively. The postoperative pain was assessed using the FLACC behavioral pain assessment scale (6), if pain scores ≥ 5 at rest, the patient received paracetamol 10 mg/kg IV.
The primary outcome was the quality of emergence, while the secondary outcome was postoperative laryngeal spasm. The quality of emergence was assessed by modified Hannallah score (7), in which crying, moving, and agitation were assessed separately and scored either (zero or one, or two, and the maximum distress score was six). Postoperative laryngeal spasm (identified by airway obstruction at different severity with paradoxical chest movement, intercostal retraction, and tracheal tug. Also, characteristic crowing sound may be heard in partial laryngospasm but was absent in complete laryngospasm). Laryngospasm was scored as follows: (1 = mild (snoring,), 2 = moderate (stridor), 3 = severe (apnea and cyanosis) (8). The recovery time was the time interval between the cessation of maintenance anesthetics till the eye-opening, and time to extubation was defined as the time from the discontinuation of sevoflurane to the removal of the endotracheal tube within a minute. Postoperative nausea and vomiting (PONV), hypotension and bradycardia were assessed during the first 24 hours.
3.1. Statistics
A pilot study, including 10 children, was performed with the technique used for both groups (five patients per group). The sample size calculation was based on estimating a 30% change in modified Hannallah score. A calculated sample size of 80 patients would be required to attain the power of at least 80% and 5% significance level with a 90% confidence interval. Therefore, we enrolled 40 patients in each group. Statistical analyses were performed using Statistical Package for the Social Sciences (version 15, SPSS Inc., Chicago, IL, USA). Statistical significance of categorical variables between the groups was compared using chi-square test and quantitative variables were compared using unpaired t-test. Quantitative variables were presented as mean ± standard deviation (SD), while ordinal data are presented as the percentage. P ≤ 0.05 was considered statistically significant.
4. Results
Among 92 infants and children were evaluated to be included in the study, 12 patients were excluded; 7 cases of them did not meet the inclusion criteria and 5 children’s parents refused to participate in this study. The remaining 80 patients were randomly allocated to the two studied groups (40 children per group) (Figure 1). Regarding demographic data, the two groups were comparable in the age, gender, duration of surgery, ASA, and body weight (Table 1).
| Demographic Data | Sevoflurane Group, N = (40) | Propofol TIVA Group, N = (40) | Tests | |
|---|---|---|---|---|
| t or χ2 | P Value | |||
| Age, mo | 7.73 ± 1.67 | 8.12 ± 1.23 | 1.189 | 0.238 |
| Sex, M/F ratio | 18/22 | 20/20 | 0.201 | 0.654 |
| BW, kg | 8.74 ± 2.02 | 9.25 ± 1.87 | 1.172 | 0.245 |
| Duration of surgery, min | 90.26 ± 5.48 | 88.67 ± 6.39 | 1.195 | 0.236 |
| ASA (I/II) | 35/5 | 34/6 | 0.105 | 0.745 |
| Dose of propofol infusion, mg/kg/h | 9.53 ± 1.28 | |||
Abbreviations: ASA, American Society of Anesthesiologists; BW, body weight; F/M, female/male; kg, kilogram; mg/kg/hr, milligram/kilogram/hour; N, number; Propofol TIVA, propofol total intravenous anesthesia; SD, standard deviation.
aValues are expressed as mean ± SD.
bP ≤ 0.05 is statistically significant.
The quality of emergence was assessed by modified Hannallah score (Table 2) 5% of the patients in the sevoflurane group had score zero, 40% had score one, and 55% had score two. On the other hand, in the propofol TIVA group, 72.5% of the cases have score zero, and one and two scores constituted 25% and 2.5%, respectively. Comparing the percentage of the patients having score zero between both groups was 60% in patients in the propofol TIVA group and 17.5% in the sevoflurane group, but one and two scores were 27.5% and 2.5%, respectively in the propofol TIVA group and 60% and 2.5%, respectively in the sevoflurane group. In the sevoflurane group 15% of the patients had agitation score zero, 57.5% of them had score one, and 27.5% score two, but in the propofol TIVA group, the percentage was 67.5%, 25%, and 7.5% for zero, one, and two scores, respectively. Altogether, a significant decrease was observed in the number of patients developed agitation after propofol TIVA anesthesia in comparison to sevoflurane anesthesia (P ≤ 0.001).
| Modified Hannallah Score | Sevoflurane Group, N = (40) | Propofol TIVA Group, N = (40) | Chi-Square | |
|---|---|---|---|---|
| χ2 | P Value | |||
| Crying | 44.075 | < 0.001b | ||
| Score 0 | 2 (5) | 29 (72.5) | ||
| Score 1 | 16 (40) | 10 (25) | ||
| Score 2 | 22 (55) | 1 (2.5) | ||
| Movement | 15.294 | < 0.001b | ||
| Score 0 | 7 (17.5) | 24 (60) | ||
| Score 1 | 24 (60) | 11 (27.5) | ||
| Score 2 | 9 (22.5) | 5 (12.5) | ||
| Agitation | 23.056 | < 0.001b | ||
| Score 0 | 6 (15) | 27 (67.5) | ||
| Score 1 | 23 (57.5) | 10 (25) | ||
| Score 2 | 11 (27.5) | 3 (7.5) | ||
Abbreviation: N, number; Propofol TIVA: propofol total intravenous anesthesia.
aValues are expressed as No. (%).
bP ≤ 0.05 is statistically significant.
Perioperative laryngeal spasm was scored as follows: (1 = mild, 2 = moderate, 3 = severe). In this regard, 32.5% and 12.5% of the patients had a postoperative laryngeal spasm in sevoflurane and propofol TIVA groups, respectively; most of the cases with moderate severity were in sevoflurane group (22.5%), but most of the cases with mild severity (7.5%) were in propofol TIVA group. A significant decrease was observed in the number of patients developed laryngeal spasm after propofol TIVA than sevoflurane anesthesia (P = 0.047) (Table 3).
| Score | Postoperative Laryngeal Spasm | |
|---|---|---|
| Sevoflurane Group, N = (40) | Propofol TIVA Group, N = (40) | |
| Mild | 1 (2.5) | 3 (7.5) |
| Moderate | 9 (22.5) | 2 (5.0) |
| Sever | 3 (7.5) | 0 (0.0) |
| Total | 13 (32.5) | 5 (12.5) |
| Chi-square | ||
| χ2 | 6.105 | |
| P value | 0.047b | |
Abbreviations: N, number; Propofol TIVA: propofol total intravenous anesthesia.
aValues are expressed as No. (%).
bP ≤ 0.05 is statistically significant.
The prolonged time of extubation was significantly higher in the propofol TIVA group than another group (14.52 minutes and 9.37 minutes, respectively) (P ≤ 0.001). Moreover, the recovery time was comparable between both groups (P = 0.382). In contrast, PONV was significantly higher in the sevoflurane group than another group (P = 0.047). No patients were developed hypotension or bradycardia during the first 24 hours in both groups (Table 4).
Abbreviations: µg/kg/hr, microgram/kilogram/hour; N, number; Propofol TIVA, propofol total intravenous anesthesia; PONV, postoperative nausea and vomiting; SD, standard deviation.
aValues are expressed as mean ± SD or No. (%).
bP ≤ 0.05 is statistically significant.
5. Discussion
Quicker recovery with less distress behavior (3), reduced airway reactivity, improved post-operative ciliary function (4), and reduced nausea and vomiting (7); are usual advantages of propofol over conventional volatile anesthetic agents. Although these advantages were in mind of the majority of anesthetist, it still wildly used for induction of anesthesia and not as maintenance in pediatric age. Upper respiratory tract infections and continuous nasal discharge without super added infection are particularly common among patients with cleft palate and carry an increased risk of airway complications. After extubation in repair surgeries, all cases must have observed carefully for any signs of airway obstruction, especially in infants with pre-existing airway problems. Airway obstruction may occur at any part of the upper respiratory tract and caused mainly by laryngospasm, upper airway narrowing, lodged blood clot, retained throat pack, and tongue edema from mouth gage. Advantages of propofol and the previously mentioned risks make the propofol ideal anesthetic for cleft palate repair surgery.
Using the parameters of the modified Hannallah score, this conclusion became obvious. Modified Hannallah score has succeeded in determining the three points defining the quality of emergency in pediatrics between 4 months to 18 years. Crying only is not a suitable tool for assessment of the quality of emergence as it can be masked by the sedative effect of opioids. Restlessness and agitation are better for the assessment of the quality of emergence. We reported a highly significant lower number of the patients developed agitation in the propofol TIVA anesthesia group than the Sevoflurane anesthesia group (P ≤ 0.001) with a higher percentage of the patients with a score zero (67.5% in the propofol TIVA group compared with 15% in the sevoflurane group).
Ortiz et al. (9), in a Cochrane Database systematic review in 2014, compared the use of intravenous versus inhalational anesthesia for pediatric outpatient surgery regarding the risk of complications and recovery times. Many studies evaluated postoperative behavioral disturbances. Picard et al. (8), assessed postoperative agitation using a four-point scale; Gurkan et al. (10), and Guard et al. (11), assessed the incidence of agitation in the PACU. All have confirmed the superiority of propofol in such matter, but no one illustrated the emergence in a detailed manner.
Mucociliary clearance is an important protective mechanism within the respiratory tract (3). Retention of secretions is a potential consequence arising from an impaired bronchociliary clearance. Sevoflurane significantly depresses bronchial mucus transport velocity in patients without lung disease compared with TIVA group. Propofol also markedly reduced airway and pharyngeal reflexes. These advantages illustrate the decrease in events of laryngeal spasm in the propofol group in a statistically significant manner in such high-risk patients.
One of the major causes of postoperative discomfort in children and their parents is vomiting as the parents consider postoperative vomiting to be the most relevant outcome. It commonly occurs in children older than 2 or 3 years, while in infants, postoperative vomiting was a minimal problem (12). This is reflected in scores indicating that the age of the patient and the duration of anesthesia was the most relevant risk factors for postoperative nausea and vomiting (13). Despite, propofol is well known for its low incidence of emetic side-effects (14). There is no difference between the two techniques in our study. This can be explained by the mentioned low risk of infants and the use of dexamethasone.
We observed a delay in the time for the decision of extubation in the propofol group. Children required a higher dose of propofol because of increased distribution from plasma to peripheral compartments. Therefore, after the termination of the infusion, the plasma levels decrease slowly, and its half-life increases more in children than adults (15). Thus the rapid awakening was not predominant in TIVA children (16). In adults, propofol context half time after 90 minutes reaches 50 minutes. However, there is no statistical difference in the net result in recovery time. The two groups are similar either in eye-opening or discharge from PACU. Propofol infusion syndrome (PRIS) was not seen in our cases because all patients were infants. The duration of surgery in all cases did not exceed 2 hours (17, 18).
5.1. Conclusions
Overall, the findings of the current study indicated that the propofol anesthesia regimen reduced the incidence of emergence agitation in children with cleft palate repair surgery more than the sevoflurane anesthesia. It is recommended to perform more studies and used methods with a larger sample size to study EA incidence in children who are anesthetized with sevoflurane.