1. Background
Today, trauma is one of the main problems that threaten the health of the community. In the Third World and developing countries, which make up about 15% of the world’s population, 11% of the total disability is caused by traumatic disease (1). Upper extremity fractures are some of the things that can have long-lasting effects on a person's life due to organ failure and disability (2). The upper extremity surgery is performed under the general anesthesia or regional block. Recently, the regional block has been used more often than general anesthesia. Performing this block in patients with difficult airway and underlying comorbid diseases is believed to be beneficial (3). Lower hospital stay, lower financial cost, and avoidance of general anesthesia complications, postoperative analgesia, and reduced opioid use and increased patient satisfaction are remarkable benefits that can be cited in comparison to a general anesthetic for peripheral nerve blocks (4, 5). The peripheral nerve blocks in the upper extremity include the interscalene, supraclavicular, infraclavicular, axillary, etc. nerve plexus. The axillary block is the most common block in this network because it is easy, reliable, and safe. The axillary block indication is forearm and hand surgery but is not suitable for the upper arm and shoulder surgeries (6). There are several techniques to determine the location of the nerve in the axillary block, and the use of sonography for this has found great popularity in anesthesia (7). Using sonography allows direct observation of needles and nerve visualization and surrounding anatomy (6, 8). Therefore, it reduces complications associated with blind techniques, such as intravascular injection, hematoma, and pneumothorax (9). Local anesthetic drugs prevent the directing of electrical impulses in nervous-muscular membranes by blocking sodium channels, causing neural block and loss of sensory and motor perception (5). Lidocaine is a commonly used local anesthetics of the amino amide bunch with a median duration effect which is also used in the epidural and spinal anesthesia (10). Local anesthetics provide good regional anesthesia, but the effect of analgesia is short-acting. Therefore, various adjuvant drugs such as opioids, clonidine, dexmedetomidine, magnesium, dexamethasone, ketamine, etc. are used to provide excellent analgesia in addition to prolonging the duration of the anesthetic effect (9). On the other hand, the time gap between block administration and adequate analgesia is a complaint, especially for surgeons. The use of adjuvants and local anesthetic has been proposed for this shortcoming (3). Opioids are commonly known as analgesics that have their place of action in the central nervous system and the spinal cord, although their analgesic effect can also occur with the activation of peripheral chemoreceptors. Fentanyl is used as a synthetic opioid in the peripheral nerve blocks to increase the length of the block effect and its quality, as well as to produce analgesia without causing central complications (11). Ketamine is an anesthetic drug with N-methyl-D-aspartic acid (NMDA) receptor which its antagonistic effect inhibits or reverses central nervous system (CNS) sensitivity to painful stimuli leading to pain relief after surgery (12). Ketamine is used as premedication, analgesic, sedation, and induction and maintenance in general anesthesia. It is also used as a central, local, and regional analgesia (13).
2. Objectives
The present study aims to comparatively investigate the effects of ketamine-lidocaine and fentanyl-lidocaine on the postoperative analgesic duration in axillary block in the upper extremity fractures.
3. Methods
The present study was a double-blinded clinical trial (IRCT20181220042064N1) performed on 60 patients aged 18 - 75 years who were candidates for the surgery of upper extremity fractures under the axillary block with ASA class I and II in Imam Khomeini and Razi Hospitals in Ahvaz in 2018. After approval by the Ethics Committee of the Ahvaz Jundishapur University of Medical Sciences (code of ethics: IR.AJUMS.REC.1397.023), written informed consent was obtained from all patients after being informed of the method of conducting the study.
The inclusion criteria included male and female patients aged 18 to 75 years. The exclusion criteria were the patient’s dissatisfaction with the study, history of any kind of seizure, allergy to drugs, patients with coagulation disorders, block site infection, traumatic upper extremity neurological damage, neuropathy, and addiction to drugs or opiates. After entering the operating room, initial monitoring, including ECG, pulse oximetry, and BP were performed.
After inserting IV line (Angiocath no. 20), 8 mg/mL normal saline and oxygen with mask 4 L/min were initiated for patients and they received 0.03 mg/kg of midazolam in the form of IV premedication. Group F received 4 mg/kg lidocaine 1% (Aburaihan Co., Iran) and 50 µg fentanyl (Aburaihan Co., Iran), and group K received 4 mg/kg lidocaine 1% and 30 mg ketamine (ROTEXMEDICA Co., Germany) during the axillary block.
The used syringe was impregnated with adrenaline 1:200000. The patients were placed in the supine position and, while the arm abducted, hands were placed behind the head. The axilla area was cleaned using an antiseptic iodine solution and draped. The neural network was identified using an ultrasound machine (EdgeTM Mini-Dock, FUJIFILMSonosite, WA98021), and a sterile needle (90 mm, 22 G) (DR.JapanCo. ltd., Japan) was inserted into the axillary block site under the ultrasound guide and the medication was injected around the neural network.
After the block was performed, the patient was monitored for complications such as hematoma, hypotension, and bradycardia. A pinprick test was performed every 5 minutes to evaluate sensory block for the median, ulnar, radial and musculocutaneous nerves (0 = not blocked, 1 = incomplete block, and 2 = complete sensory block). A three-point scale test was performed for the motor block (0 = normal motion, 1 = paresis, 2 = paralysis).
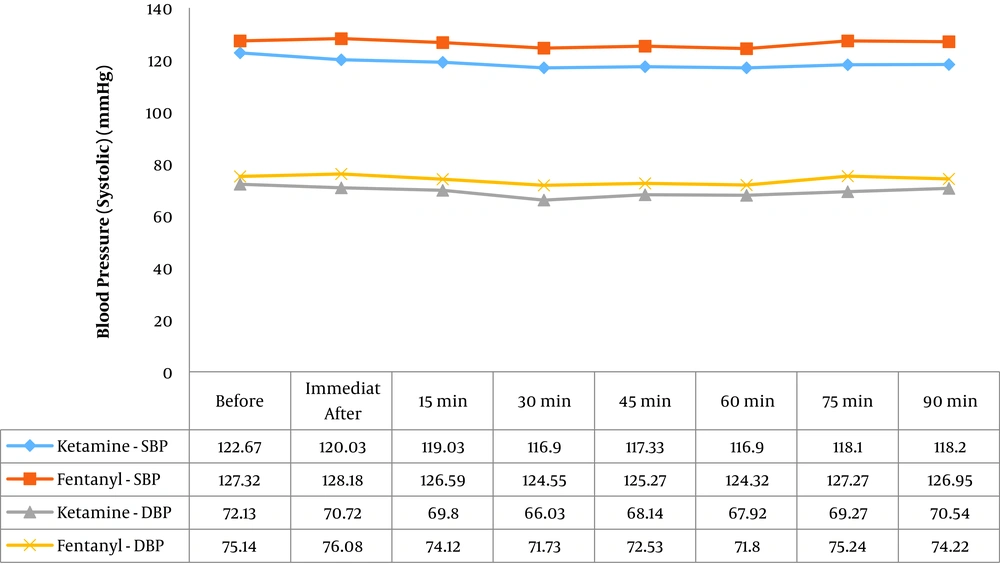
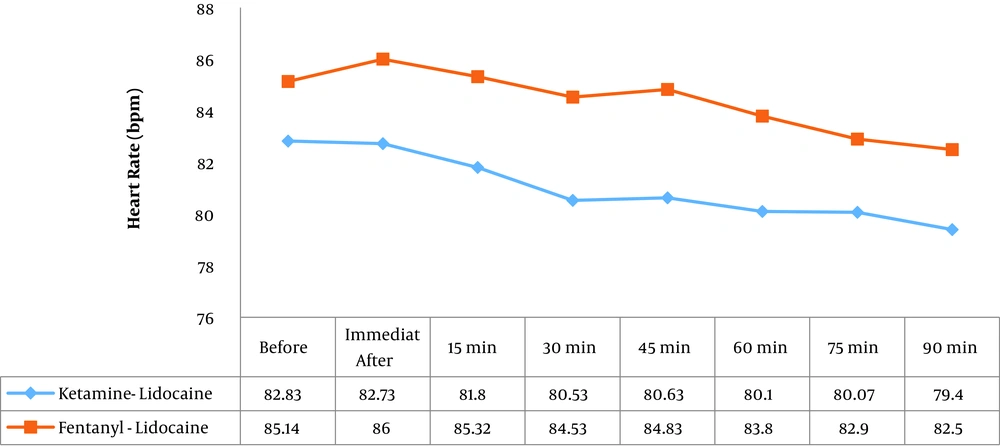
If the block was not successful, the patient was excluded from the study. After complete sensory and motor block, the surgery started. The mean of systolic and diastolic blood pressure and heart rate was measured at 8 different times, including before axillary block, and immediately, 15, 30, 45, 60, 75, 90 minutes after block. Upon completion of the surgery and transferring the patient to the recovery room, the completion of the sensory and motor block was evaluated.
The evaluation of postoperative pain was performed based on visual analogue scale (VAS) at 15, 30 minutes, 1, 2, 3, 4, 5, 6, 9, 12, and 24 hours after the block. When the VAS score exceeds 3, the patient received 0.2 mg/kg of intravenous pethidine and the overall dose of opioid received by the patient was calculated for a 24-hour postoperation period. The duration of analgesia was monitored from the onset of the complete block to the occurrence of pain with an intensity of greater than 3 (VAS > 3).
To blind the study, the patient information was recorded by a person who did not know the type of medicine. In addition, the data were analyzed by a person who was unaware of the patient groups. To describe the data, the mean and standard deviation (SD) were used for quantitative variables and frequency and percentage for qualitative variables. Chi-square, t-test (or Mann-Whitney test) were used to analyze the data. All analyses were performed using SPSS software version 20.
4. Results
The demographic data of the patients in both groups are presented in Table 1.
| Variable | Ketamine-Lidocaine | Fentanyl-Lidocaine | P Value |
|---|---|---|---|
| Age, y | 35.3 ± 13.6 | 40.6 ± 15.2 | 0.16 |
| Gender | 0.08 | ||
| Female | 10 (33.3) | 12 (40) | |
| Male | 20 (66.7) | 18 (60) | |
| Duration of operation, min | 56.3 ± 11.8 | 60.4 ± 9.6 | 0.14 |
aValues are expressed as mean ± SD or No. (%).
bThe statistical test used was t-test for continuous data and chi-square test for qualitative data.
There was no significant difference in mean age, distribution of gender, and duration of operation in the two groups (P > 0.05).
The mean pain intensity at 9, 12, and 24 hours after the surgery was significantly lower in the fentanyl group than in the ketamine group (P < 0.0001), in other times of the measurement, pain intensity did not differ significantly between the two groups (P < 0.05) (Table 2).
| Different Time Points After Surgery | Pain Scores (Measured by VAS) | P Value | |
|---|---|---|---|
| Ketamine | Fentanyl | ||
| 15 min | 0.00 ± 00 | 0.00 ± 00 | - |
| 30 min | 0.00 ± 00 | 0.00 ± 00 | - |
| One hour | 0.1 ± 0.0 | 0.1 ± 0.1 | 0.82 |
| Two hours | 0.1 ± 0.1 | 0.2 ± 0.1 | 0.302 |
| Three hours | 0.1 ± 0.1 | 0.2 ± 0.1 | 0.64 |
| Four hours | 0.5 ± 0.1 | 0.6 ± 0.2 | 0.668 |
| Five hours | 0.9 ± 0.2 | 0.8 ± 0.2 | 0.685 |
| Six hours | 1.4 ± 0.3 | 0.9 ± 0.2 | 0.154 |
| Nine hours | 3.4 ± 0.3 | 1.2 ± 0.3 | < 0.0001b |
| 12 hours | 3.9 ± 0.3 | 1.5 ± 0.3 | < 0.0001b |
| 24 hours | 3.9 ± 0.3 | 1.0 ± 0.2 | < 0.0001b |
aValues are expressed as mean ± SE.
bThe statistical test used was the t-test.
The mean duration of analgesia in the fentanyl group was slightly higher, but there was no significant difference between the two groups (P > 0.05). The time of the first request for a painkiller in the fentanyl group was slightly longer, but there was no significant difference between the two groups (P > 0.05). The mean of the received opioid (pethidine) was significantly lower in the fentanyl group 24 hours after surgery (P < 0.0001). It should be noted that in the ketamine group, all patients received pethidine within 24 hours of surgery, but in the fentanyl group, 8 patients (26.7%) had no pain intensity more than 3 hours after 24 hours and did not receive pethidine.
The mean duration of complete sensory and motor block for the median, ulnar, radial and musculocutaneous nerves was shorter in the fentanyl group, but the difference was not significant between the two groups (P > 0.05). The mean of onset of the sensory and motor block for the median, ulnar, radial and musculocutaneous nerves in the fentanyl group was shorter than the ketamine group, but there was no significant difference between the two groups (P > 0.05) (Table 3).
| Variable | Ketamine | Fentanyl | P Value |
|---|---|---|---|
| Duration of regional analgesia, min | 290.0 ± 20.8 | 356.0 ± 62.9 | 0.32 |
| Time of administration of first dose of pethidine, h | 7.70 ± 2.4 | 8.6 ± 2.8 | 0.25 |
| Total pethidine dose, mg | 66.0 ± 18.5 | 35.5 ± 14.4 | < 0.0001b |
| Duration of sensory block, min | |||
| Median | 226.0 ± 56.1 | 248.0 ± 60.5 | 0.15 |
| Ulnar | 218.0 ± 56.9 | 246.0 ± 57.6 | 0.07 |
| Radial | 226.0 ± 49.1 | 244.0 ± 62.9 | 0.22 |
| Musculocutaneous | 232.0 ± 49.6 | 248.0 ± 66.3 | 0.29 |
| Duration of motor block, min | |||
| Median | 198.0 ± 44.9 | 220.0 ± 9.2 | 0.08 |
| Ulnar | 192.0 ± 48.3 | 216.0 ± 55.9 | 0.08 |
| Radial | 198.0 ± 42.1 | 218.0 ± 48.5 | 0.09 |
| Musculocutaneous | 196.0 ± 44.4 | 222.0 ± 54.9 | 0.06 |
| Onset of sensory block, min | |||
| Median | 8.0 ± 3.4 | 7.7 ± 3.1 | 0.69 |
| Ulnar | 8.3 ± 3.3 | 7.6 ± 3.4 | 0.44 |
| Radial | 9.4 ± 5.3 | 8.5 ± 3.5 | 0.39 |
| Musculocutaneous | 9.5 ± 3.3 | 8.0 ± 3.4 | 0.09 |
| Onset of motor block, min | |||
| Median | 8.2 ± 3.6 | 7.8 ± 3.4 | 0.71 |
| Ulnar | 8.5 ± 3.5 | 8.3 ± 5.3 | 0.87 |
| Radial | 9.8 ± 5.4 | 8.5 ± 3.5 | 0.57 |
| Musculocutaneous | 9.3 ± 3.4 | 7.8 ± 3.1 | 0.08 |
aValues are expressed as mean ± SD.
bThe statistical test used was the t-test.
Changes in hemodynamic parameters, including systolic and diastolic blood pressure and heart rate in both groups were stable during normal surgery (Figures 1 and 2).
Complications during and after surgery, including seizure, nausea, and vomiting, respiratory depression and hallucination were reported in none of the patients in both groups.
5. Discussion
In this study, at 9, 12, and 24 hours after the surgery, the severity of pain (based on VAS) in the fentanyl group was significantly lower than the ketamine group, and the mean received opioid (pethidine) within 24 hours after the surgery in the fentanyl group (35.5 mg) was significantly lower than the ketamine group (66 mg). The mean duration of analgesia in patients receiving fentanyl-lidocaine (356 min) was slightly higher than that in the ketamine-lidocaine group (290 min), but there was no significant difference between the two groups. Moreover, the time of the first request for a painkiller in the group receiving fentanyl-lidocaine (8.5 h) was slightly higher than that in the group receiving ketamine-lidocaine (7.7 h), but there was no significant difference between the two groups. In the study of Mudaraddi and Kumar Kanthi, in which 100 µg fentanyl was used as an adjuvant with 20 cc bupivacaine 0.5% and 10 cc lidocaine 2% in the supraclavicular block, the duration of postoperative analgesia was increased (14). Lashgarinia et al. (15) used 2 mg/kg of ketamine with 5 mg/kg lidocaine1.5% in the supraclavicular block for elbow, forearm and wrist surgery, and in the group that did not receive ketamine, the mean score of VAS was significantly higher. In addition, the time of the first request for a painkiller in the group that did not receive ketamine was significantly lower (15). In our study, the mean sensory and motor length for all four median, ulnar, radial, and musculocutaneous nerves was slightly higher in the fentanyl group, but there was no significant difference between the two groups. The onset of the sensory and motor block was also lower in the fentanyl group, but there was no significant difference.
Senel et al. (16) in a study conducted in Turkey showed that adding 50 mg ketamine to 40 cc of ropivacaine 0.375% for patients undergoing arm and shoulder surgery did not improve the effects of local anesthesia in the brachial network and did not prolong analgesia after surgery. The results of Karakaya et al. (17) showed that adding 100 µg fentanyl to 40 cc bupivacaine 0.25% in the axillary block significantly increased the sensory and motor block and postoperative analgesia compared to the control group. The results of Lee et al. (18) showed that the use of 30 mg ketamine as an additive with 30 cc rupivacaine 0.5% did not have any effect on sensory and motor block and postoperative analgesia. In our study, the mean change in systolic and diastolic blood pressure in both groups was normal and did not change significantly before the anesthesia. Heart rate changes in both groups were decreased in the normal range and did not change significantly before the anesthesia. Overall, hemodynamic status was stable during the surgery in both groups.
5.1. Conclusions
Both drugs are useful for the axillary block, but due to the less pain intensity and less need of analgesics in the fentanyl group, fentanyl may be a better drug for use as an adjuvant in the axillary block in comparison to ketamine. It is recommended that in subsequent studies, higher ketamine dosages should be used for comparison and also studying and comparing other drugs to achieve better drugs as an adjuvant.