1. Background
Changes in the lung function following open heart surgery have been well documented by researchers (1-5). Unfortunately, its incidence remains unacceptably high (6). Researchers believe that, of the many reasons for this event, three factors play a major role: the extracorporeal circulation, the anesthesia and surgical technique which can cause a systemic inflammatory response following the use of cardiopulmonary bypass (CPB), entrapment of neutrophils in the pulmonary capillaries due to endotoxins, and the release of several pro-inflammatory agents (7). Its clinical manifestations range from transient hypoxemia to severe pulmonary injuries (ALI) and acute respiratory distress syndrome (8).
Chest physiotherapy treatment is routinely applied to the patients after open heart surgery, at the intensive care unit (ICU), during the first few days post-surgery. The goals of the physiotherapy are to decrease pain (9), reduce the accumulation of pulmonary secretions, pneumonia, and atelectasis, maintain pulmonary volume, correcting the ratio of ventilation and perfusion, reduce airway resistance, improve respiratory and peripheral muscle strength, minimize postoperative complications, shorten the length of hospitalization, and consequently reduce the patient morbidity and mortality (10).
Various techniques of chest physiotherapy and breathing exercise with or without mechanical devices are routinely recommended for open heart surgery patients to prevent or reduce the incidence of impaired lung function. They include early mobilization, positioning (11), incentive spirometry (IS), expiratory positive airway pressure (12, 13), deep breathing exercises (14), respiratory muscle training (15), coughing support (16), and active cycle of breathing techniques (ACBT) (17).
The common cycle of ACBT involves breathing control, expansion training, breathing control, and huffing technique. The number and frequency of each ACBT component can be changed, but all the components of the cycle must be applied and vary with the control of respiration (17). An overview of existing literature reveals inconsistent results regarding the effect of airway cleaning techniques such as ACBT in patients with a wide range of lung diseases. Some of these studies have reported no effect of this type of intervention on the lung function such as in patients with bronchiectasis (18), COPD (19), and heart failure (20). On the other hand, some other studies have proven its therapeutic effects, such as in post-operative lung cancer patients (21, 22).
2. Objectives
Nevertheless, there are limited reports available on preferred chest physiotherapy methods in patients with CABG surgery (16). The aim of this study was to compare the effect of ACBT and routine chest physiotherapy on pain and respiratory parameters in patients undergoing CABG surgery.
3. Methods
This randomized controlled trial was conducted from July to November 2018 in Shafa Hospital in Kerman, Iran. Seventhly eligible patients, after CABG surgery in the open-heart ICU in Shafa Hospital affiliated to Kerman University of Medical Sciences were enrolled in the study.
The inclusion criteria were: age within 18 - 60 years, undergoing non-emergency CABG surgery, having cognitive, speaking and hearing ability, not being addicted, no history of open heart surgery, no sever pulmonary disease, no renal dysfunction, no mechanical ventilation longer than 24 h after surgery, and no known psychological illness.
On the other hand, the exclusion criteria included: unwillingness to stay in the study, initiation of early complications after surgery (such as: cardiac shock, sever hypotension, bleeding, cardiac tamponade, kidney dysfunction), dangerous dysrhythmia (such as: atrial fibrillation and ventricular tachycardia), loss of consciousness, cerebral difficulties, renal and pulmonary complications, congestive heart failure, deep vein thrombosis, bleeding, myocardial infarction, being connected to the ventilator for more than 48 hours.
The sampling was performed based on the inclusion criteria. For all subjects in two groups, after complete consciousness, stability of the vital signs within 6 and 7 h after the surgery, and removal of the tracheal tubing in the evening shift, initially the arterial blood gas analysis as the main outcome was performed. Then, the pain severity, heart rate, and respiratory rate were measured as the secondary outcomes. Note that all patients in this department have an arterial line and before removal of the tracheal tubing, the arterial blood gas analysis is performed every 2 - 4 hours, but after removal of the tracheal tubing, this test is performed as needed.
In the ACBT group, the patient was placed in a fowler position. The ACBT was performed in three stages. The first stage was the breathing control. In this stage, breathing was carried out slowly through the nose. If breathing through the nose was not possible, it was done through the mouth. This should be performed with the "lips of the bud". During this step, the patient is encouraged to maintain calm by closing their eyes and away from any tension. Then he/she places one hand on his/her abdomen and exhales as if the shoulders move downwards and feel burning in the abdominal area. The second stage is the practice of extending the chest wall to provide airflow in small airways. At this stage, the air flows deeply, slowly and continuously through the nose into the lungs, so that the chest wall is expanded. The air is held for 2 - 3 seconds, and then it deflates out slowly and through the mouth. This step was repeated 3 times. The final was the huff stage and the integral part of this technique. In this stage, coughing was done through open mouth and throat. This will move the discharge from small airways to the larger airways and eventually discharges it. For this purpose, at first, the patient performed an intermediate respiration. Next, with opened mouth and with the help of respiratory muscles, he/she took a deep tail and then coughed. The ACBT intervention was performed on the two consecutive days after operation, each day one session, each session 3 courses and each course for 10 minutes with 15 minutes of rest between them.
For the routine physiotherapy group, chest wall vibrations and manual percussions were done. For this purpose, a vibrating device with a constant frequency of 50 Hz per second was used for 1.5 minutes, which was performed by placing the device on the patient's anterior and posterior chest wall. Then, the hand percussion was carried out on the anterior and posterior chest wall of the patient, using a hand palm which came in the form of a cup and from the wrist area, at a height of 10 cm. The vibration and precaution were done on a bed sheet. Manual percussion was performed 25 times in 10 seconds for 2 minutes. Then, the patient was encouraged to do effective coughs.
All patients received the basic post-operative care such as early mobilization, changes in positioning, and active exercises of the upper limbs.
Immediately after the completion of the routine physiotherapy and the ACBT in both groups, again the arterial blood gas levels were measured. Also, for both groups, the pain severity, heart rate, and respiratory rate were measured post intervention.
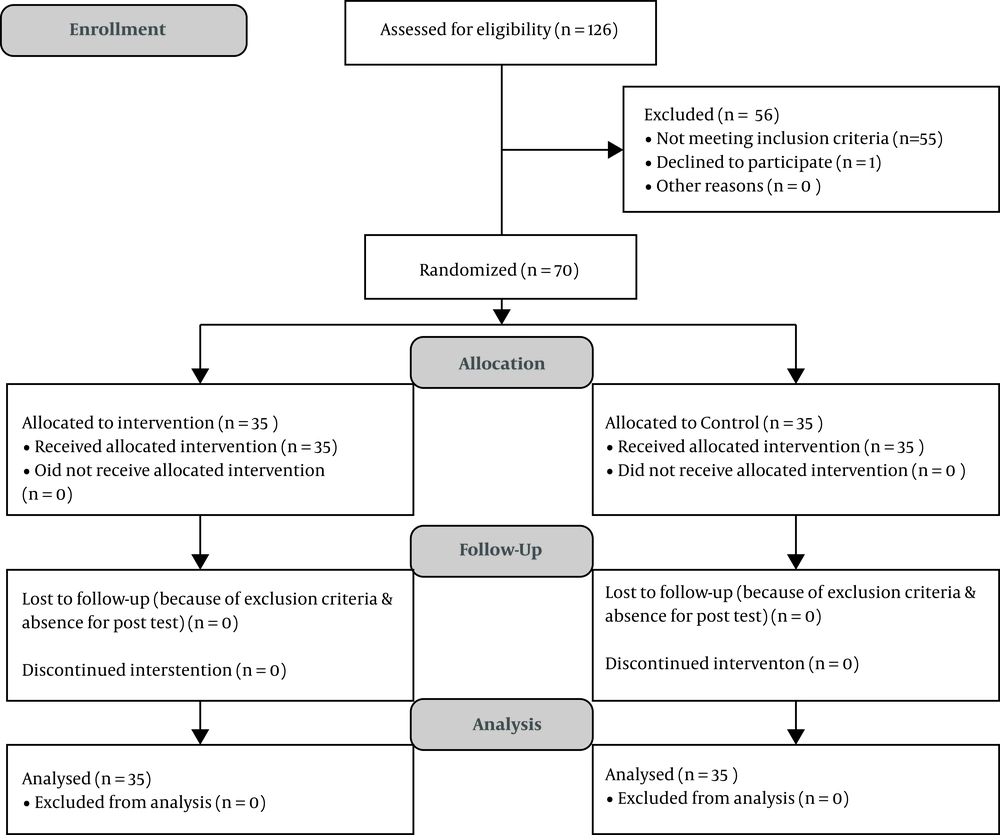
The sample size was considered to be approximately 70 (35 for each group) according to the following formula with a standard deviation of 11 at the significance level of 0.05 and power of 90%, along with the effect size of 9 in terms of minimum significant changes in average partial pressure oxygen (23).
Overall, 70 patients were assigned into ACBT and routine chest physiotherapy groups equally based on sex classes via minimization method (24). The samples were randomly placed in the classes, where eventually the total number in each class would be equal. Sampling continued until reaching the sample size.
Data collection was done by face-to-face interviews. The data collection tool included a demographic questionnaire (age, sex, smoking history), and the 10-degree visual analog scale (VAS) for pain intensity evaluation. This tool was standard and its validity and reliability were confirmed (24). For evaluation of respiratory parameters, the arterial blood gas was analyzed which contained: partial pressure oxygen (PaO2), arterial oxygen saturation (SaO2), partial pressure carbon dioxide (PaCo2), arterial PH, and bicarbonate level (HCO3). The pulse and respiration rate were also recorded. Arterial blood gas analysis was conducted by the GEM Premier 3000, USA (25), which was calibrated at the patient's temperature during sampling using 300-bit cartridge made by GEM Premier USA.
The study was approved by the Research Council and Ethics Committee of Rafsanjan University of Medical Sciences (with ethical code number: IR.RUMS.REC.1397.010). This trial was also registered at the Iranian Clinical Trial Registry (with the IRCT identification code: IRCT20180304038935N1). All participants were informed of the study objectives and explained that their company is voluntary and may leave the study whenever they wished. Prior to entering the study, all participants signed a written informed consent form and were assured that their presence or absence in the study did not influence their routine care in the hospital.
Data analysis was performed by SPSS software V.22 using Kolmogorov-Smirnov test, chi-square test, paired samples t test, independent two samples t-test, Wilcoxon signed ranks test, and the Mann-Whitney U test, at a significance level of 0.05.
4. Results
In the current study, a total of 126 CABG candidate patients were assessed. Out of them, 55 patients were excluded due to non-compliance with exclusion criteria. One patient declined to participate. Thus, 70 patients were enrolled in the study randomly. Finally, the blood gases, pain, HR, and RR were evaluated for 70 patients in two groups. The sampling details have been explained in a consort flow diagram (Figure 1).
The results showed that the mean and standard deviation of the age of the subjects was 52.69 ± 6.02 with a minimum of 41 and a maximum of 60 years. There was no statistically significant difference between the two groups in terms of age, gender, and smoking history (Table 1).
aChi-square test
bIndepended two samples t-test
The internal Mammary artery grafting was performed for all patients and according to the hospital protocol, all patients were discharged on the fifth to sixth postoperative day.
The results of arterial blood gases analysis showed that all changes in the blood PH lied within the normal range. There were no statistically significant differences in the blood PH level changes in within and between group comparisons (P > 0.05). The reference value was considered 7.35 - 7.45.
The results showed that, in the physiotherapy group, on the first and second days, the PaO2 significantly increased at post intervention phase (P = 0.001). In the ACBT group on the first day, the PaO2 had no significant changes, but on the second day the PaO2 increased significantly at post intervention phase (P = 0.001). However, in between group comparisons, no significant difference was observed. The reference value for PaO2 was considered 75 - 100 mmHg.
The results of atrial oxygen saturation (SaO2) analysis revealed that, in the physiotherapy group on the first and second days, the SaO2 significantly increased at post intervention phase (P = 0.001, P = 0.005 respectively). Also, in ACBT group on the first and second days, the SaO2 increased significantly at post intervention phase (P = 0.001). However, in between group comparisons, no significant difference was observed. The results of other respiratory parameters are reported in Table 2.
| Physiotherapy Group, Mean ± SD | ACBT Group, Mean ± SD | P Valuea | |
|---|---|---|---|
| PH | |||
| The first day | |||
| Before intervention | 0.06 ± 7.40 | 0.06 ± 7.43 | 0.034 |
| After intervention | 0.06 ± 7.40 | 0.06 ± 7.44 | 0.015 |
| P valueb | 0.775 | 0.446 | |
| Mean changes | 0.002 ± 0.041 | 0.006 ± 0.048 | 0.690 |
| The second day | |||
| Before intervention | 7.42 ± 0.07 | 7.44 ± 0.05 | 0.196 |
| After intervention | 7.41 ± 0.05 | 7.44 ± 0.05 | 0.076 |
| P valueb | 0.496 | 0.722 | |
| PaO2 | |||
| The first day | |||
| Before intervention | 12.87 ± 69.54 | 10.97 ± 73.74 | 0.188 |
| After intervention | 13.69 ± 75.62 | 10.74 ± 71.27 | 0.527 |
| P valueb | 0.001 | 0.236 | |
| The second day | |||
| Before intervention | 74.42 ± 12.48 | 71.27 ± 10.74 | 0.261 |
| After intervention | 84.17 ± 13.38 | 80.14 ± 9.32 | 0.149 |
| P valueb | 0.001 | 0.001 | |
| PCO2 | |||
| The first day | |||
| Before intervention | 5.29 ± 38.67 | 5.00 ± 36.88 | 0.151 |
| After intervention | 6.73 ± 37.56 | 4.46 ± 34.93 | 0.058 |
| P valueb | 0.020 | 0.286 | |
| The second day | |||
| Before intervention | 7.40 ± 35.48 | 5.73 ± 36.75 | 0.425 |
| After intervention | 7.77 ± 35.73 | 4.45 ± 36.61 | 0.562 |
| P valueb | 0.834 | 0.083 | |
| SaO2 | |||
| The first day | |||
| Before intervention | 3.60 ± 92.26 | 4.79 ± 91.72 | 0.600 |
| After intervention | 3.51 ± 93.84 | 2.62 ± 94.08 | 0.747 |
| P valueb | 0.005 | 0.001 | |
| The second day | |||
| Before intervention | 2.84 ± 93.89 | 2.47 ± 93.72 | 0.782 |
| After intervention | 2.83 ± 95.50 | 1.58 ± 95.59 | 0.868 |
| P valueb | 0.001 | 0.001 | |
| HCO3 | |||
| The first day | |||
| Before intervention | 3.80 ± 23.71 | 2.79 ± 24.60 | 0.976 |
| After intervention | 3.59 ± 22.92 | 4.58 ± 22.69 | 0.293 |
| P valueb | 0.263 | 0.021 | |
| The second day | |||
| Before intervention | 3.59 ± 22.92 | 4.05 ± 24.66 | 0.060 |
| After intervention | 4.42 ± 22.48 | 3.43 ± 24.55 | 0.032 |
| P valueb | 0.490 | 0.863 |
aIndependent sample t-test
bPaired sample t-test
The results of vital sign analysis revealed that, in both groups on the first and second days, the HR significantly increased at post intervention phase (P = 0.001). However, in between group comparisons, no significant difference was found (P > 0.05). Based on the results, the median and IQR of respiratory rate (RR) in both groups, on the first and second days, significantly increased at post intervention phase (P = 0.001). On the other hand, in the between group comparisons, only on the second day, at post-intervention, the RR was significantly higher in the physiotherapy group than in ACBT group (P = 0.001, effect size = 0.724).
Finally, the results of the pain severity comparison showed that, in both groups on the first and second days, the pain significantly increased at post intervention phase (P = 0.001). However, no significant difference was observed in between group comparisons (Table 3).
| Physiotherapy Group, Median ± IQR | ACBT Group, Median ± IQR | P Valuea | |
|---|---|---|---|
| RR | |||
| The first day | |||
| Before intervention | 17 ± 5 | 17 ± 5 | 0.957 |
| After intervention | 21 ± 7 | 21 ± 9 | 0.403 |
| P valueb | 0.001 | 0.001 | |
| The second day | |||
| Before intervention | 17 ± 5 | 14 ± 5 | 0.114 |
| After intervention | 25 ± 5 | 21 ± 6 | 0.011 |
| P valueb | 0.001 | 0.001 | |
| HR | |||
| The first day | |||
| Before intervention | 77.55 ± 16.72 | 75.51 ± 15.43 | 0.595 |
| After intervention | 89.82 ± 16.08 | 87.25 ± 11.63 | 0.446 |
| P valueb | 0.001 | 0.001 | |
| The second day | |||
| Before intervention | 73.40 ± 12.02 | 72.08 ± 9.79 | 0.618 |
| After intervention | 87.51 ± 13.54 | 83.60 ± 9.90 | 0.172 |
| P valueb | 0.001 | 0.001 | |
| Pain | |||
| The first day | |||
| Before intervention | 0 ± 1 | 0 ± 1 | 0.480 |
| After intervention | 3 ± 1 | 3 ± 1 | 0.990 |
| P valueb | 0.001 | 0.001 | |
| The second day | |||
| Before intervention | 0 ± 0 | 0 ± 1 | 0.489 |
| After intervention | 2 ± 1 | 3 ± 1 | 0.695 |
| P valueb | 0.001 | 0.001 |
aMann-whitney U test
bWilcoxon signed ranks test
5. Discussion
Our study indicated that ACBT and routine chest physiotherapy with early mobilization had the same effects on most arterial blood gases following CABG. In reviewing the existing literature, limited studies have compared the effects of ACBT and routine physiotherapy on respiratory outcomes in patients undergoing CABG surgery. Further, the ACBT has shown a controversial effect on the lung function and respiratory parameters in various situations. Similar to our results, Savci et al. have shown that the ACBT and incentive spirometry had similar effects on respiratory parameters, lung function, and rate of atelectasis in patients undergoing CABG surgery (17). Meanwhile, Grammatopoulou et al. found that the ACBT method and respiratory physiotherapy did not differ in the reduction of pulmonary complications in patients with rib fractures (26). It seems that ACBT has a more positive effect on patients undergoing abdominal surgery than on CABG patients, and on blood oxygenation than on pulmonary function. In a study, Wange et al. found that the ACBT had a better performance in improving pulmonary function in patients undergoing abdominal surgery compared to incentive spirometry (27). Also, Syropoulos et al. observed that ACBT from the third post-operative day led to a significant increase in the SPO2. However, in comparison with routine physiotherapy, there was no effect on the prevention of pulmonary complications in patients undergoing major surgery in the upper abdomen (28).
In this study, we found that the respiratory and heart rate on two consecutive days, in both groups, had a significant increase after intervention; on the second day, the respiratory rate in the routine physiotherapy group was significantly higher than in the ACBT group. Similar to the results of this study, Savci et al. found that in patients undergoing CABG surgery, there were no significant differences in the heart rate in ACBT group compared to spirometry, though, in both groups after the intervention, the heart rate increased significantly (17). Çırak et al. noted that the heart rate increased in patients undergoing CABG surgery following physiotherapy. Note that high risk patients showed a significant increase in the heart rate as compared to low risk patients (29). Since the implementation of these two methods is considered a physical activity, therefore, increase in heart rate and respiration is expected. Nevertheless, this increase should occur in the normal range.
Contrary to the opinion of physiotherapists who believe that patients undergoing CABG experience a great deal of pain on the first day after surgery (30), in the present study, we found that the mean change in pain score during ACBT and routine physiotherapy was similar. In addition, we observed a similar mild pain perception during the first two days after the operation. These results indicated that postoperative pain was well managed. Similar to this study, Savci et al. observed that there was no significant difference in perceived pain between patients undergoing CABG surgery in the ACBT group and spirometry (17). In this regard, Grammatopoulou et al. examined the effectiveness of chest physiotherapy and the active cycle of breathing techniques for pain management in patients with rib fractures. In contrast to our results, they concluded that the ACBT method was more effective in pain reduction when compared to the control group (26). Also in another study, ACBT was associated with pain relief at rest and during coughing from the 5th postoperative day in upper abdominal surgery patients (28).
Despite the great strengths of this study, such as controlling the confounding factors, this study had its own limitations. First, the effect of two types of intervention on pulmonary function was not considered due to separation of patients from the ventilator device. Further, some elderly patients were not familiar with the VAS scale.
Overall, it can be said that the results of this study are the starting point for research in this field and provide significant assistance in selecting the preferred intervention to improve arterial blood gases following CABG surgery.
5.1. Conclusions
In summary, the results suggested that ACBT and routine physiotherapy could be used safely during two consecutive days after CABG surgery. Note that the physiotherapy intervention on the second day increased the RR to an abnormal level. Both methods increased the pain perception to a mild level and HR in the normal range. Further studies are recommended to determine which methods are appropriate for which patients.