1. Background
Propofol is one of the most commonly used drugs for the induction and maintenance of anesthesia. Quick wakening up and short context-sensitive half-life after prolonged intravenous infusion are among the advantages of this drug, which in turn increase the tendency for using this drug for the maintenance of anesthesia in outpatient operations, emergencies and intensive care units (1, 2). However, cardiovascular complications caused by the administration of this drug including reduced cardiac contractility, decreased heart rate, reduced peripheral vascular resistance, suppression of baroreceptor reflex and sudden decrease in blood pressure, especially in elderly patients and those with an underlying cardiac disease, and shocks have limited the use of this drug (3-5).
The existing evidence suggests that the use of low doses and titers of ketamine can be effective in reducing the cardiovascular effects of propofol; nevertheless, this administration method can increase the chance of waking up during anesthesia. Some studies have reported the effect of anesthesia induction using a single propofol dose and low ketamine doses on the hemodynamic stability of patients in short-term outpatient operations in emergency departments. On the other hand, no report has been published so far regarding hemodynamic changes due to propofol infusion in more prolonged operations.
2. Objectives
Herein, we aimed to evaluate the intra and post-operative hemodynamic effects of ketofol infusion in comparison with propofol infusion.
3. Methods
After obtaining the approval the Ethics Committee of Birjand University of Medical Sciences and registering the study at the Iranian Center for Clinical Trials (code: IRCT2015062222867N1), this double-blind clinical trial was conducted on patients aged 15 to 45 years old who were candidates for leg fracture surgery of class I and II of the American Society of Anesthesia for physical risk stratification in Imam Reza Hospital affiliated to Birjand University of Medical Sciences. The flow diagram of the study is presented in Figure 1.
The inclusion criteria were all patients aged 15 to 45 years old who were candidates for elective leg fracture surgery with general anesthesia. The exclusion criteria included patients with a previous history of upper respiratory tract infections, allergies to propofol-ketamine, eggs or soy, psychosis, epilepsy, cardiac diseases, drug and alcohol abuse, diabetes, hypertension, opium addiction and history of postoperative nausea and vomiting. According to the study performed by Akin et al. (6), the sample size was determined as 27 patients in each of the two independent groups based on the ratio comparison formula with the confidence level of 95% and test power of 80%.
Written consent was obtained from all the patients, and then they were randomly assigned to one of the two groups using a computer-based method and permuted-block randomization. After insertion of venous catheter number 18, anesthesia was induced in both groups using propofol 2 mg/kg (Cordenpharma, Italy), fentanyl 2 µg/kg (Darou Pakhsh, Iran) and atracurium 0.5 mg/kg (Aburaihan pharmaceutical, Iran). To maintain the anesthesia in the Propofol and Ketofol groups, propofol infusion 100 µg/kg/min and ketofol infusion (propofol 50 µg/kg/min + ketamine 25 µg/kg/min [Sterop, Belgium]) were used, respectively. The drugs used to maintain anesthesia were prepared in the same syringes by an anesthesia technician who was not involved in the study. The drugs were prescribed to maintain anesthesia according to the study grouping.
Heart rate and systolic, diastolic and mean blood pressure were measured prior to the induction of anesthesia, immediately after the induction of anesthesia, after laryngoscopy and at 10-minute intervals until the end of the surgery. They were also recorded by an independent researcher who was blinded to the study grouping. The severity of pain and nausea and vomiting frequency were recorded in both groups immediately after the operation and each 2 hours until 6 h. Pain severity was evaluated immediately to 6 hours after the surgery at 2-h intervals based on the visual analog scale (VAS). If VAS > 4, intravenous ketorolac (15 mg) was prescribed. The severity of nausea was also evaluated based on VAS, where the absence and highest severity of nausea were indicated by scores 0 and 10, respectively. If VAS > 4, intravenous ondansetron (4 mg) was prescribed.
Data were entered into SPSS version 18. The two groups were compared in terms of heart rate, systolic, diastolic and mean blood pressure, severity of pain and nausea, vomiting frequency and the doses of analgesics and antiemetic drugs used. Data analysis was conducted by t-test and Mann-Whitney U-test after evaluating the homogeneity of the data by the Kolmogorov-Smirnov test. P value less than 0.05 was considered statistically significant.
4. Results
Overall, 45 (83.3%) of the patients were male (23 [85.2%] in the ketofol and 22 [81.5%] in the propofol group [P = 0.17]), and the mean age of the patients was 30.48 ± 7.46 years in the ketofol and 29.14 ± 7.61 years in the propofol groups (P = 0.51). There was no statistical difference between the two groups regarding age and sex distribution.
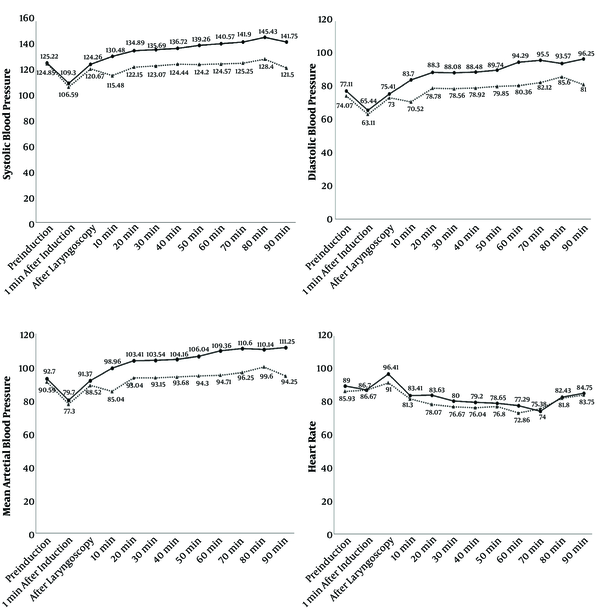
Figure 2 presents the trends of heart rate and systolic, diastolic and mean arterial blood pressure both groups. As the figure clearly shows, there was no difference between the two groups regarding systolic, diastolic and mean arterial blood pressure before induction, 1 minute after induction and after laryngoscopy. However, they were significantly higher in the ketofol group compared to the propofol group at 10 to 60 min after induction. On the other hand, heart rate showed the same trend in both groups (Figure 2).
trend and mean of systolic, diastolic, mean arterial blood pressure and heart rate measured before induction of anesthesia (baseline), 1 minute after induction, after laryngoscopy and then in 10 minutes intervals to the discharge from recovery in ketofol (solid line) and propofol (dotted line) groups.
The severity of pain and nausea has been compared in Table 1. None of the participants in the ketofol group had nausea immediately and 6 hours after the surgery. However, 1 hour and 4 hours after the surgery, the intensity of nausea was not significantly different between the two groups.
| Postoperative Nausea | Postoperative Pain | |||||
|---|---|---|---|---|---|---|
| Group K | Group P | P Value | Group K | Group P | P Value | |
| After surgery, h | ||||||
| Immediately | - | - | - | 2.22 ± 3.555 | 1.37 3.053 | 0.34 |
| 2 | 0.56 ± 1.601 | 0.04 ± 0.192 | 0.10 | 2.52 ± 3.55 | 1.41 3.01 | 0.22 |
| 4 | 0.41 ± 1.474 | 0.37 ± 1.334 | 0.92 | 0.93 ± 2.28 | 1.93 3.07 | 0.18 |
| 6 | - | - | - | 0.67 ± 1.92 | 1.11 | 0.46 |
| Total drug dose | 1.85 ± 3.958 | 0.74 ± 2.669 | 0.23 | 13.89 ± 11.71 | 12.78 ± 10.77 | 0.71 |
Severity of Pain and Nausea Reported Immediately After Surgery and in 2 hours Intervals to 6 Hours After Surgery in Ketofol (k) and Propofol (p) Groupsa
The frequency of nausea, vomiting and pain medicine prescription in both groups are presented in Table 2. At 2 hours after surgery, the frequency of nausea in the ketofol group was higher than in the propofol group (3 [11%] in the ketofol group vs. 1 [3.7%] in the propofol group; P = 0.29). Nausea severity and drug dosage were not significantly different between the groups. Also, with the exception of two patients in the propofol group, 6 hours after surgery, none of the participants had vomiting during the follow-up (Table 2). However, compared to the propofol group, the ketofol group reported more pain at the outset of follow up, which improved by the end of follow-up. Also, postoperative pain severity and drug dosage were not significantly different between the two study groups (Table 1).
| Groups | Group P | Group K | P Value |
|---|---|---|---|
| Nausea | |||
| 2 hours after surgery | 1 (3.7) | 3 (11.1) | 0.29 |
| 4 hours after surgery | 2 (7.4) | 2 (7.4) | 1 |
| Vomiting | |||
| 6 hours after surgery | 2 (7.4) | 0 (0) | 0.15 |
| Prescription pain medicine | 18 (66.7) | 18 (66.7) | 1 |
Comparison of Postoperative Complications in Two Groupsa
5. Discussion
Rapid onset of action and short duration of action have made propofol a desirable drug for the induction and maintenance of anesthesia (7). However, the cardiovascular effects of this drug have limited its use, especially in patients with cardiac diseases and hemorrhagic emergency. Based on the available studies, the use of drugs such as ketamine as an anesthetic induction agent can reduce the suppressing hemodynamic effects of propofol, in addition to reducing the need for high propofol doses (8). To the best of our knowledge, most studies have investigated the use of a single ketamine dose in the induction of anesthesia, while the use of this drug in infusion has not been examined except in cases of local anesthetic procedures requiring sedation. In the present study, we compared he hemodynamic effects of ketamine + propofol infusion in relation to propofol infusion alone for the maintenance of anesthesia in 54 patients undergoing leg surgery.
In this study, systolic, diastolic and mean blood pressure were comparable in the two groups before and after anesthesia induction as well as immediately after intubation. On the other hand, the values of these variables were significantly higher in the ketofol group than in the propofol group at 10-minute intervals until the end of the operation.
Tang et al. (9) compared the effects of addition of low dose ketamine to propofol-fentanyl and propofol-fentanyl alone for sedation in 80 patients who were candidates for gynecologic diagnostic laparoscopy. They observed that mean blood pressure was consistently higher in the Ketamine group, as sympathomimetic effects of ketamine might have overcome the cardiovascular effects of propofol, thereby maintaining hemodynamic stability in these patients compared to the propofol-treated patients. In contrast with our findings, a study performed by Singh et al. (10, 11) comparing the cardiovascular effects of propofol alone and in combination with ketamine or fentanyl for sedation in patients undergoing endoscopic ultrasonography showed no significant differences in the mean blood pressure or heart rate at any time point among the groups. These conflicting results are probably related to the type of the procedures, as tubal ligation is a surgical operation, while endoscopy is a minimal invasive procedure (9).
Although there was a higher incidence of nausea in the Ketofol group, there was no significant difference between the two groups in terms of the incidence and severity of nausea and vomiting in the present study. Inconsistent with this finding, another study comparing the administration of a bolus dose of ketofol, compared to fetofol (fentanyl + propofol) showed significantly higher severity of nausea in the ketofol group than in the Fetofol group (11).
Based on the available literature, nausea and vomiting are the known complications of ketamine (12, 13). In contrast, propofol has anti-nausea and vomiting effects; therefore, considering the longer recovery time in the ketamine-treated group than in the propofol group, the higher incidence of nausea and vomiting in patients receiving the combined bolus regimen of propofol and ketamine seems logical after administering a single dose. On the other hand, since propofol + ketamine combination was used in our study for intraoperative infusion, it probably increases the metabolism of context-dependent propofol, resulting in its elevated plasma levels and recovery time in comparison with its single dose. On the other hand, this can overlap the recovery time of ketamine and propofol, thereby reducing the nausea-inducing effects of ketamine. Also, the infusion of a low dose of ketamine probably has less pre-emetic effects (14). In our study, the severity of postoperative pain at the outset of follow-up (immediately after surgery and 2 hours later) was higher in the ketofol group than in the propofol group, which decreased in the ketofol group compared to the propofol group in the next follow-ups (4 and 6 hours postoperatively). However, none of these changes were significant in the two groups. The results of another relevant study revealed that the ketamine + propofol combination led to better analgesia compared to propofol alone (15-17).
It can be concluded that the infusion of a mixture of ketamine and propofol improves hemodynamic stability in addition to better analgesia compared to the infusion of propofol alone. Nevertheless, it led to heightened risk of nausea and vomiting. We did not investigate the effect of ketofol infusion on opiate doses and the recovery time. Therefore, future studies are recommended to address these issues. In addition, further studies are warranted to investigate the use of sub-hypnotic doses of ketamine + ketofol combination for infusion in surgical procedures.
5.1. Limitations
The difference between the patients’ definition of pain intensity, the difference between the patients’ definition of nausea intensity, exaggeration in describing their pain for affecting others, and the patients’ unawareness of their condition after surgery were the research constraints.