1. Background
Toxoplasma gondii is an intracellular protozoan that causes toxoplasmosis disease, which is a worldwide infection and has approximately infected one-third of the world’s population (1, 2). In humans, infection with this parasite is known as a risk factor for the development of schizophrenia and depression (3-6). The prevalence of toxoplasmosis is varied from 8.2% to 63.2% and 11.0% to 80% in Europe and American, respectively (7).
The prevalence of infection in different regions of Iran is varied based on weather conditions. Environmental conditions, such as the changes in humidity and temperature have a direct effect in maintaining sporulation of oocysts excreted by the final host cat (1). Studies in different regions in Iran show that the seroprevalence of T. gondii infection was at 39.3% among the general population (8).
The number of parasites, parasite virulence, genetic background, sex, and immunological status of individuals seem to affect the progression of the infection. Toxoplasmosis has two acute and chronic forms (9). The chronic form is seen in people who seem to be healthy (1). Typically, in people with an effective immune system, toxoplasmosis is a benign infection and does not cause a specific problem (2). The parasite develops cysts in various organs, including different anatomical places of the brain and various types of neurons. Consequently, the infection can cause various hormonal and mental disorders and probably some personality and behavioral changes (1, 6, 10) like obsessive-compulsive disorder, suicide, Alzheimer’s, Parkinson’s disease, epilepsy, migraine headaches, mental retardation, and behavioral and neurological disorders (3-6).
Previous studies have shown the relationship between toxoplasmosis and the phenomenon of anxiety and depression (5, 6).
2. Objectives
One of the most important pillars of human health is mental health, which is an aspect of the general concept of health. Since the study of the most common psychiatric disorders in soldiers with chronic toxoplasmosis has not been done yet, the aim of this study was to investigate the most common mental disorders in soldiers with chronic toxoplasmosis.
3. Methods
3.1. Study Design
In a cross-sectional study, a total of 239 blood samples were taken from the voluntary soldiers in one of the garrison in Tehran, Iran. Then, the MMPI-short form 71 questionnaires were filled by them.
3.2. Laboratory Tests
The blood samples were centrifuged (2000× g, 10 min) and the serum was separated and stored at -70ºC. Then, the serums were analyzed for anti-Toxoplasma gondii IgG antibodies using ELISA (Capitia TM. T.gondii (Toxo) IgG Capita TM) kits). IgG antibodies against T. gondii levels of > 1/1 UL/mL were considered to be seropositive. A positive IgG test was interpreted as chronic toxoplasmosis.
3.3. MMPI Tests
Then, seropositive and seronegative groups were defined and these two groups were compared for mental health using MMPI-short form 71 test. Depression, anxiety, and six other mental disorders were evaluated by this general mental health test.
3.4. Validity and Reliability of the Questionnaire
The validity and reliability of the MMPI questionnaire were measured in the different studies in Iran and around the world (11). In the current study, the alpha Cronbach’s coefficient of the hypochondria, depression, hysteria, psychopathic deviation, paranoia, psychasteria, schizophrenia, and mania were: 0.80,0.70, 0.85, 0.77, 0.87, 0.79, 0.82, and 0.71, respectively, and 0.78 totally.
3.5. Statistical Analysis
Kolmogorov-Smirnov test was used to check the normality of the data. Regarding the non-normalization of the data, the Mann-Whitney test was used for comparison the mean of score in mental disorders, and the chi-square test was used for analyzing the pattern of diet between groups. The significance level was considered to be P < 0.05. Analyses were performed using SPSS software version 16 (SPSS Inc., Chicago, IL, USA).
4. Results
A total of 69 (28.87%) out of 239 samples were seropositive. The seropositive was significantly higher in the ones who consumed unpasteurized milk, undercooked meat (juicy), and contacted with soil (Table 1) (using chi-square test, P < 0.05).
| Serum | IWOHOCS | IWHOCS | Cooked Meat | Undercooked Meat | Unpasteurized Milk | Pasteurized Milk |
|---|---|---|---|---|---|---|
| Seropositive 69 (28.87%) | 90.8 | 9.2 | 41.8 | 58.2 | 53.1 | 46.9 |
| Seronegative 170 (71.13%) | 99.4 | 0.6 | 60.0 | 40.0 | 38.4 | 61.6 |
Abbreviations: IWHOCS, individuals with a history of occupational contact with the soil; IWOHOCS, individuals without a history of occupational contact with the soil
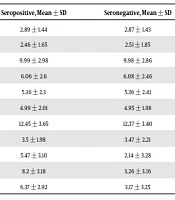
The MMPI-short form 71 test revealed that the mental disorders were not significantly different between the seropositive and seronegative groups (Table 2).
| Groups, Indicator | Seropositive, Mean ± SD | Seronegative, Mean ± SD | P Value |
|---|---|---|---|
| Perfectionism and lying | 2.89 ± 1.44 | 2.87 ± 1.43 | 0.66 |
| Mental disturbance and sense of cooperation | 2.46 ± 1.65 | 2.51 ± 1.85 | 0.26 |
| Defense mechanism and security feeling | 9.99 ± 2.98 | 9.98 ± 2.86 | 0.83 |
| Psychopathic deviation | 6.06 ± 2.6 | 6.08 ± 2.46 | 0.77 |
| Hypochondria | 5.36 ± 2.3 | 5.36 ± 2.41 | 0.96 |
| Paranoia | 4.99 ± 2.01 | 4.95 ± 1.98 | 0.72 |
| Hysteria | 12.45 ± 3.65 | 12.37 ± 3.40 | 0.61 |
| Mania | 3.5 ± 1.98 | 3.47 ± 2.21 | 0.96 |
| Psychasthenia | 5.47 ± 3.10 | 2.14 ± 3.28 | 0.68 |
| Depression | 8.2 ± 3.18 | 3.26 ± 3.16 | 0.3 |
| Schizophrenia | 6.37 ± 2.92 | 3.17 ± 3.25 | 0.82 |
5. Discussion
Toxoplasmosis have been hypothesized to be the etiology of some mental disorders. The effect of the toxoplasmosis on human personality, physiology, and morphology were assessed using the personality questionnaire and there was a significant difference between personality traumatized men and women (12); it is not consistent with the outcome of this study. As the questionnaire, the age, and sex of subjects are different in the current study, perhaps, these factors affected to obtain the different outcome.
The relationship between toxoplasmosis and schizophrenia, the proposed mechanisms of the pathogenesis of schizophrenia, the simultaneous participation of genetic, and infectious and environmental factors that cause brain growth and differentiation were assessed and recorded, which is capable of affecting some of the metabolic and coagulation pathways led to the development of the disease disorder (13). This result is not consistent with the present study and maybe, the involvement of other organs in seropositive cases (apart from brain) happened in the current study (10). According to the other studies, the involvement of the nervous system or brain in chronic toxoplasmosis occurred in the upper and middle ages more, consequently, neurological symptoms will appear more in older individuals. In the other words, as age increases, the likelihood of behavioral disorders increases (14, 15). Since the age of the soldiers in the current study were between 18 to 25 years old, it is supposed that the immune system could still suppress and control the parasite, and the neuritis has not taken place yet, or due to the gradual progression, symptoms has not been observed yet (14-16).
Another study recorded that chronic toxoplasmosis was significantly higher in patients with schizophrenia than in healthy ones; it disagreed on the result of the current study. It seems that the different outcome between two studies might be due to the different subjects of them. The study tried to detect the chronic toxoplasmosis in schizophrenic patients as a subject, however, in the present study, on the contrary, mental disorders were looked for in ones with chronic toxoplasmosis as subjects (6).
In the present study, 69 (28.8%) soldiers were seropositive, which was confirmed by some studies (17). According to the results of this study, how the meat and milk were consumed, and lack of hygiene in contact with the soil were the important ways to transmit the toxoplasmosis and should be of more concern.
5.1. Conclusions
Overall, the soldiers with chronic toxoplasmosis, as a young community, showed no significant mental disorders and similar research in older groups or females is suggested. There were chronic toxoplasmosis in soldiers and the prevalence of toxoplasmosis, especially chronic form was high. Therefore, the infection of toxoplasmosis should be considered. The strength of this study was the group that was considered (soldiers). In terms of their behavior, the results help us know which parts they should be employed in during their military service. The limitation of this study was “the lack of knowledge about the locality of tissue cysts in the body of ones with chronic toxoplasmosis”. If the brain was involved, the mental disorders would be followed better.