1. Background
Globally, family planning is an important task for reproductive-aged couples. The numbers of contraceptive methods have expanded in need of reproductive health care. These methods typically focus on women, and there are limited options for men. Studies have demonstrated that stable, reliable, reversible, accessible, and cost-effective methods are desirable for this purpose (1-4).
However, in this context, condoms, withdrawal, and vasectomy are limited methods of male contraception (1). Vasectomy is often considered as the most common contraceptive method, due to the highly effective reversal success rate. The chance for pregnancy rate after successful vasectomy reversal is 40% - 60% and also, in 70% - 90% of cases, sperms return to the ejaculate (5). It is important because approximately 6% of couples will request reversal within 5 years after sterilization, while men have a 2% - 6% of this portion (5). This is most likely because of remarriage or accidental loss of child/children.
With advances in urological procedures, various surgical approaches have been described to reverse vasectomy. Microscopic vasovasostomy is one of the most common techniques that was introduced in the 1970s (6, 7). Since then, many studies have been developed to consider different surgical and anesthetic methods, which aimed to determine the modified microsurgical vasovasostomy as a method of choice to attain the best results (8, 9).
2. Objectives
With the excellent patency and pregnancy rates, the microsurgical procedure has been recognized as a more common method for vasectomy reversal. Here, we present our experience of Modified Double-Layer Microsurgical technique (MDLT) compared with Three-Layer technique (TLT) for 3 years.
3. Methods
After receiving our Research Committees’ approval (code no.: 86/93/457), we reviewed and analyzed the records of the selected microsurgical vasovasostomy procedure performed on patients for 3 years.
Only records, in which vasectomy reversals were requested for the first time with a proven fertility history, were included in the present study. Also, records that had registered any post-vasectomy complications, including infection and bleeding, or history of pelvic/inguinal surgery, were excluded. The patients’ age, periods of obstruction and their wife’s age, and fertility status data were extracted.
Thirty individuals in the Modified Double-Layer Microsurgical technique (MDLT) and twenty-four in Three-Layer technique (TLT) methods were randomly enrolled in this study.
3.1. Vasovasostomy Techniques
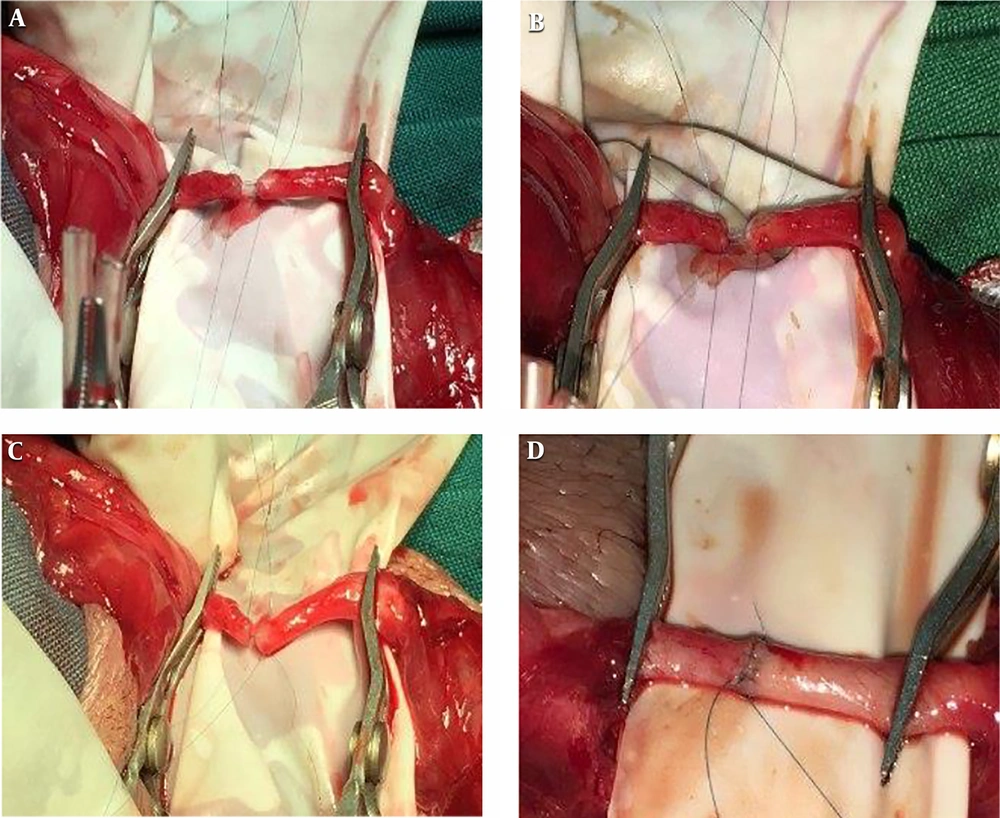
The end-to-end vasovasostomy (VV) was performed when the clear or pasty liquid from the epididymal end of vas deferens was seen. All patients underwent bilateral end-to-end VV under general or spinal anesthesia. Here we analyzed only records that were carried out by a single microsurgeon and the decision to allocate the Modified Double-Layer Microsurgical technique (MDLT) or Three-Layer technique (TLT) microsurgical vasovasostomy procedure was made based on his decision. (Figure 1).
For the Modified Double-Layer technique (MDLT) briefly, 4 sutures with a 9 - 0 or 10 - 0 nylon were placed at 3, 6, 9, and 12 o’clock positions in the mucosa. The anastomosis was completed using an 8 - 0 non-absorbable continuous seromuscular suture. Then the testis was returned to the normal anatomic position within the scrotum.
For the Three-Layer technique (TLT), the interior mucosal layer was stitched together by four 10 - 0 non-absorbable sutures, without any tensile strength. At the second layer, muscle walls of both vasal stumps were sutured by using 8 - 0 non-absorbable threads. It involved 6 stitches. Six 8 - 0 non-absorbable sutures were placed in the adventitial connective tissue surrounding the duct position. All the surgeries were performed by one surgeon.
The patients were prohibited from heavy exercise and ejaculation until after about 1 month. Also, they were followed until pregnancy was achieved, or the patient was lost to follow-up visit.
3.2. Semen Analysis
Semen analysis was performed for all patients after a 4-day sexual abstinence by masturbation. The complete semen analyses were performed according to WHO guidelines of 2010 (10).
3.3. Data Analysis
All patients were divided into 2 subgroups according to microsurgery technique. For calculation of the pregnancy rate, only patients with natural pregnancy that was confirmed by fetal heartbeats were included. Also, the presence of any sperm in the ejaculate was defined as patency. Then statistical analyses of unpaired student’s t-test or χ2 were carried out using SPSS (V. 15.0) and a value of P < 0.05 was considered significant.
4. Results
In this report, twenty-four men underwent TLT-VV (group 1) and thirty men MDLT-VV (group 2). These 54 participants showed no significant difference in the age of men (P value = 0.319), and the age of their wives (P value = 0.345). Also, there was no significant difference in the causes of vasectomy reversal between the two groups (P value = 0.392) (Table 1). There was no significant difference between study groups in the fertility history (P value = 0.561), the presence of a sperm granuloma (P value = 0.21), and underlying diseases (P value = 0.345).
| TLT-VV (N = 24) | MDLT-VV (N = 30) | |
|---|---|---|
| Age, y | 42.9 ± 1.4 | 41.4 ± 0.9 |
| Wife’s age, y | 33.3 ± 0.5 | 33.1 ± 0.8 |
| Causes of vasovasostomy | ||
| Loss of wife | 12 (50) | 12 (40) |
| Accidental loss of child | 7 (29) | 9 (30) |
| Remarriage | 5 (21) | 9 (30) |
| Patency rate | ||
| Age of men, y | ||
| < 35 | 2 (100) | 2 (100) |
| 35 - 50 | 18 (94.7) | 26 (96.3) |
| > 50 | 2 (66.7) | 1 (100) |
| Vasectomy interval, y | ||
| < 5 | 6 (85.7) | 9 (90) |
| 5 - 10 | 13 (92.9) | 18 (100) |
| > 10 | 3 (100) | 2 (100) |
| Total | 22 (91) | 29 (96) |
| Pregnancy rate | ||
| Age of men, y | ||
| < 35 | 2 (100) | 1 (50) |
| 35 - 50 | 8 (42.1) | 11 (40.7) |
| > 50 | 0 | 0 |
| Vasectomy interval, y | ||
| < 5 | 4 (57.1) | 7 (70) |
| 5 - 10 | 4 (28.6) | 5 (27.8) |
| > 10 | 2 (66.7) | 0 |
| Total | 10 (41) | 12 (40) |
Outcomes of Microsurgical Techniquesa
Here, we observed 21.1 ± 3.9 × 106/mL and 20.8 ± 2.3 × 106/mL in semen, respectively in group 1 and group 2. No significant difference between groups was found in patency rates (P value = 0.95). The mean intervals in vasectomy of group1 were 7.2 ± 0.7 years, and this did not differ significantly in group 2 (6.0 ± 0.5 y) (P value = 0.168). The patency rate was shown to be only faintly correlated with age (r = 0.364, P value = 0.01). Also, no correlation was found between patency rates and vasectomy interval (r = -0.05, P value = 0.717).
All participants in both groups were subdivided based on their age less than 35 y, 35 - 50 y, and more than 50 y. Afterward, fertility rate and patency were compared between two groups, and significant differences were not seen (P value > 0.05) (Table 1).
All participants in both groups were categorized based on vasectomy interval: 5 > y, 5 - 10 y, and 10 < y. The same comparison was made between vasectomy with patency and fertility. Also, a comparison of sperm granuloma with patency in both groups showed no significant differences (Table 1).
5. Discussion
Since 1975, introducing microscopic vasectomy reversal operation has brought advantages to family planning and sexual health. High throughput return of fertility, without any need for Assisted Reproductive technique (ART), placed this technique in the first step of fertility for those who underwent a vasectomy in the past.
Alongside microsurgical tools and procedures, ongoing advances, the outcomes of this technique have been improved. Comparing outcomes of VV in end-to-end and side-to-end types of three-layer VV technique showed 31% to 85% outcomes, with a 35% mean of the fertility rate. The same pattern can be seen in the Jee and Hong study (11), which reported 72 % patency rate and 28 % pregnancy rate in monolayer microsurgery while these rates increased in microsurgical technique (96% and 40% respectively). Using Microsurgery, we observed a 94% patency rate (51/54) that was in agreement with Hsieh et al. and Lee et al. (12) results (96% and 93 %, respectively) (12, 13). Also, this result was higher than the Safarinejad et al. (7) report (82.3%). Similar to Safarinejad et al. (7), we observed no significant difference in pregnancy rate. Although Safarinejad et al. (7) concluded that this is related to parameters such as partner features (age, fertility status), but we have matched groups. The homology in our results may be a reflection of our limited records that make a definitive conclusion hard.
Sperm leakage, mainly in a monolayer subtype of VV, is one of the most important complications of the VV technique that gets the surgeons’ attention (11). One of the advantages of the 2-layer anastomosis is the control and prevention of this problem. In our study, the MDLT-VV technique, by providing a perfect seal of the internal layer and facilitated layer connection, prevents any leakage. Also, Safarinejad et al. (7) pointed out the negative effect of non-absorbable suture material on the long-term patency after VV, while in approximately 5 years of follow up, we have no similar report.
Although significant differences were not observed between the 2 techniques in the present study, patients satisfactory associated with shorter operation time, made MTLV-VV interested.
5.1. Conclusions
It seems that Modified Double-Layer technique may be placed on the first step of Microscopic end-to-end vasovasostomy. It’s safe, high throughput and reversible traits made it a remarkable surgical approach to vasectomy reversal and family planning.