1. Introduction
Soft tissue sarcomas are rare among adult malignant tumors (0.7%) (1). Liposarcoma, which was first introduced by Virchow in 1857 (2, 3), is a tumor due to malignant transformation of adipose tissue (4). It is the most common soft tissue sarcoma (5); 30% of liposarcomas have a myxoid pathologic feature (6). This tumor often occurs in the retroperitoneum and extremities (7) and adults aged 40-60 years, with slightly more prevalent in males (8). It is relatively rare in the head and neck regions (5%-9%) (9, 10). The metastatic cases reported in the head and neck region are even rarer in comparison to primary tumors. Here is reported a case of suspected metastatic liposarcoma tumor in the inferior alveolar nerve canal.
2. Case Presentation
A 40-year-old female patient was referred to the Oral and Maxillofacial Medicine Department of Tehran University of Medical Sciences. Her chief complaint was numbness of the chin and the lower lip, started one month ago from the right side and gradually extended to the left side. However, the main dysesthesia still focused on the right side. On history, she had painful swelling in the right thigh, surgically removed two years ago. The lesion was myxoid liposarcoma without lymphatic or vascular invasion.
After surgery, she underwent radiotherapy. After one year, a tumor was excised from her thorax, which was myxoid/round cell liposarcoma, based on histopathology findings.
Upon examination, bilateral dysesthesia of the skin of the lower lip and chin was observed. The mandibular incisors of both sides were vital. Based on these data, panoramic radiography was ordered, in which an irregularity was observed in the alveolar nerve canal on the right side.
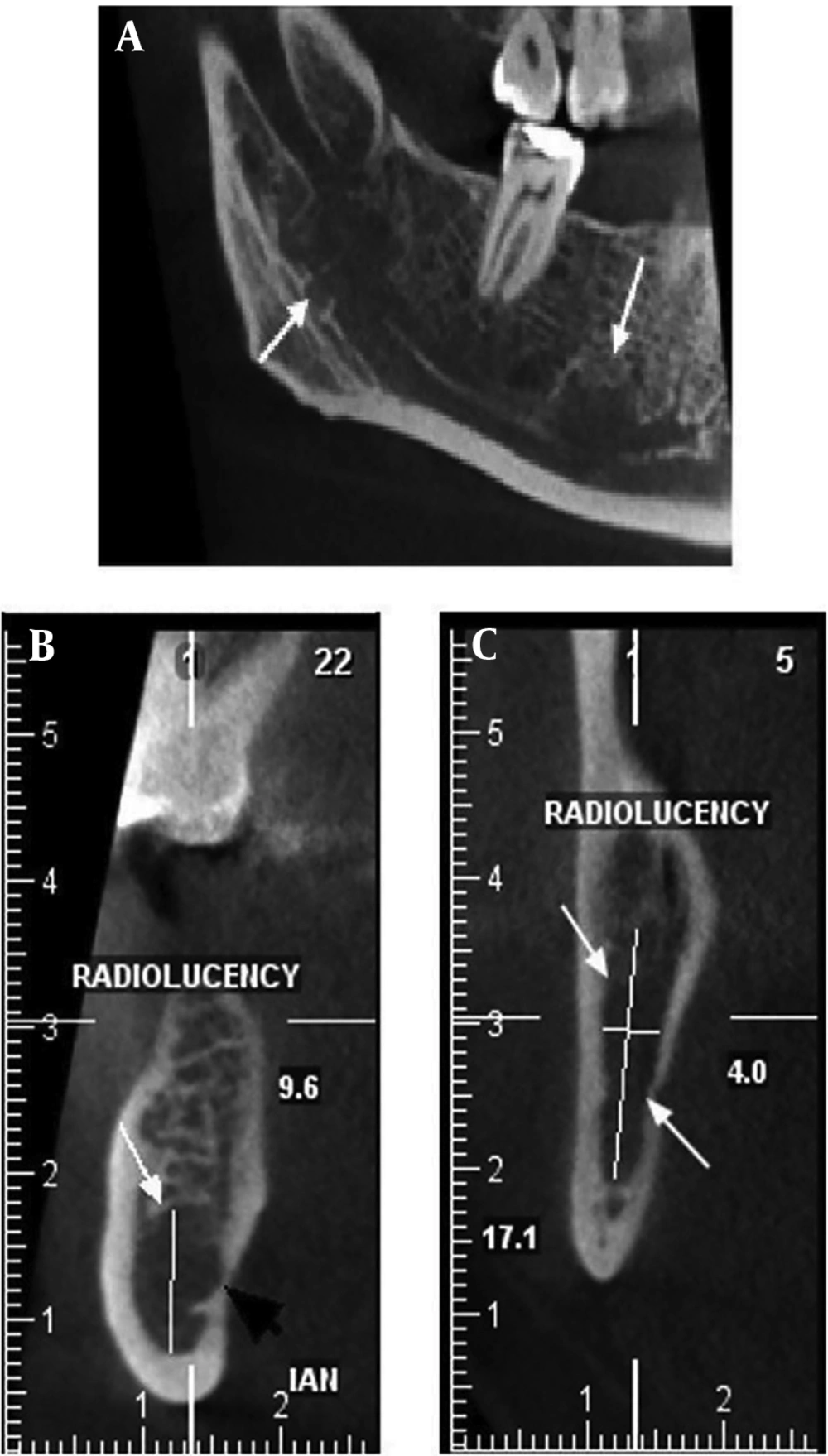
For further examination, a cone beam computerized tomography (CBCT) was performed on her mandible, showing two radiolucent areas (6.4 × 9.6 and 17.1 × 4 mm) with ill-defined borders on the right side. The lesions were close to the inferior alveolar canal, and the cortical border of the canal was not detectable in the proximity of the lesion. No cortical expansion or thinning was observed in buccal and lingual plates (Figure 1).
The patient was referred to her oncologist to investigate possible metastasis of liposarcoma to the mandible.
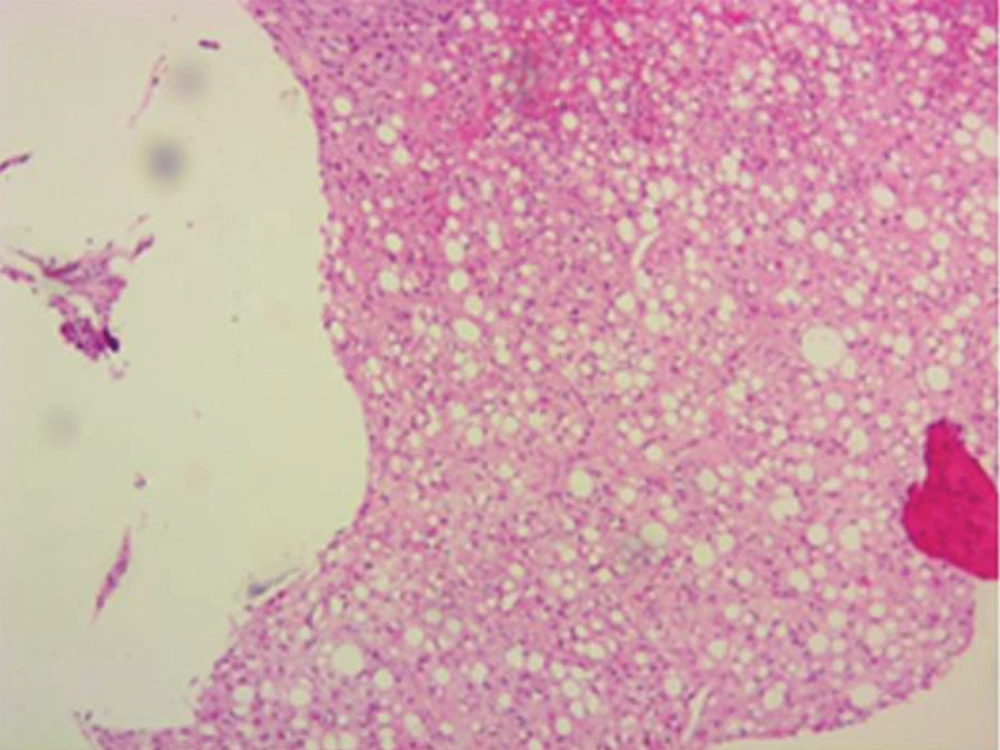
The oncologist preferred to order a total body FDG-PET/CT (fluorodeoxyglucose-positron emission tomography/computed tomography) scan. Its report indicated soft tissue densities in the posterior trunk, especially on the left side. Then, a core needle biopsy of the bone marrow was performed. Microscopic examination of bone marrow revealed sarcoma with a myxoid background containing fat cells and rare lipoblasts. The stroma had arborizing, thin-walled vessels replacing normal hematopoietic elements. The pathology report was compatible with metastatic liposarcoma (Figure 2).
According to the extent of the disease, the oncologist decided to use the palliative chemotherapy regime of AIM (Adriamycin, Ifosfamide, Mesna).
Surgery is the standard treatment of liposarcoma. If surgical treatment is not sufficient or the tumor progresses, chemotherapy and radiography are employed, which were applied to the reported patient. Unfortunately, the patient was lost to follow-up.
3. Discussion
Liposarcoma is the malignant tumor of lipoid cells. The reported cases of head and neck liposarcoma are few, mostly occur in the neck, face, larynx, dura, orbit, oral cavity, ears, mandible, and parotid, respectively (11). The metastatic cases to the head and neck region are extremely rare. Studies on metastatic liposarcoma in the head and neck region, using the keywords "Metastatic Liposarcoma" and "Head" and "Neck", were searched in the English language database of PubMed and the search engine of Google Scholar, and finally, a total of 25 cases were found (Table 1).
| Author | Patient's Age | Patient's Gender | Primary Area | Metastatic Area |
|---|---|---|---|---|
| Trabelsi (12) | 42 | M | Thigh | Parotid |
| Daly (13) | 46 | M | Lower extremities | Larynx |
| Zagzoog (14) | 43 | F | Lower extremities | Skull base |
| Haft (14) | 52 | M | Thigh | Brain |
| Paraf (14) | 27 | M | Heart | Brain |
| Arepally (14) | 56 | M | Thigh | Brain |
| Fitzpatrick (14) | 74 | F | Thigh | Brain |
| Kumar (14) | 73 | F | Thigh | Brain |
| Joshua (15) | 68 | M | Left shoulder | Right gingival mucosa |
| Tysome (15) | 51 | M | Thigh | Thyroid |
| Fabi (15) | 53 | M | Retroperitoneum | Bilateral orbits |
| Ohashi (15) | 38 | M | Left tibia | Submandibular region |
| Ohashi (15) | 41 | M | Left knee | Anterior neck |
| Brandwein-Gensler (15) | 86 | F | Thigh | Thyroid |
| Azar (15) | 30 | F | Thigh | Thyroid |
| Bashir (15) | 55 | F | Buttock | Thyroid |
| Bailey (15) | 54 | F | Sublingual | Parafalcine dura mater |
| Utsunomiya (15) | 44 | M | Thigh | Dura mater and skull base |
| Fezza and Sinard (15) | 75 | F | Abdomen | Orbit |
| Cheng (15) | Not specified | Not specified | Buttock | Dura mater |
| Tijl (15) | 52 | F | Not specified | Orbit |
| Nasr (15) | 57 | F | Retroperitoneum | Orbit |
| Peison (15) | 50 | M | Retroperitoneum | Scalp |
| Abdalla (15) | 43 | M | Thigh | Orbit |
| Tatsis (16) | 78 | M | Scrotal | Tongue |
According to the current review report, there was no metastatic case of liposarcoma to the mandibular nerve canal, and the reported case might be the first one with mental numbness as the first sign of metastasis. Although clinical signs, panoramic radiographic view, and CBCT confirmed the presence of the lesion in the mandibular canal, PET-FDG CT scan was negative for any lesion in the site. The false-negative result of the PET-FDG CT scan can be related to the low activity of the tumor, while the method is based on the metabolic activity of the lesion (17). The small tumor size (18, 19) and the spatial resolution limitations related to PET-FDG CT scan (17) were the other reasons for the false-negative results.
Although the mandibular lesion was not detected by PET-FDG CT scan, it led to finding other metastatic lesions.
3.1. Conclusion
Signs and symptoms of patients with a history of cancer should be considered more cautiously since they could be the first trace of cancer metastases or recurrence.