1. Background
Benign prostatic hyperplasia (BPH) is a pathologic process that is one but not the only cause of lower urinary tract symptoms (LUTS) in aging men (1, 2). Standard surgical treatment for symptomatic benign prostatic enlargement in prostates with volumes between 30 and 80 milliliters is monopolar transurethral resection of the prostate (TURP) (3). However, TURP can lead to significant hematuria and blood loss postoperatively (4, 5). Aspirin is essential for the prevention of cardiovascular events. It is estimated that 25% of elderly patients should receive aspirin, and in some cases, life-long treatment is needed (6-8). Thus, prescribing aspirin is a serious difficulty for urologists. A study by Devereaux et al. concluded that prescribing aspirin before surgery and during initial periods after surgery has no significant effect on mortality and non-lethal myocardial infection rate but increases the risk of major hemorrhage (9). Oscarsson et al. reported that treatment with aspirin led to a 7.2% reduction in major cardiac complications after surgery, and no significant difference was seen in surgical complications between the two study groups (10).
2. Objectives
Despite the large bulk of studies on the continuation/discontinuation of aspirin in perioperative periods in various surgeries, it seems that there is no consensus regarding the timing of aspirin administration before and after urologic operations. Given these conflicting results, we aimed to investigate the probable effects of aspirin on hemorrhage and postoperative cardiac complications after TURP, hoping to find more definite conclusions on the rate of surgical complications with the prescription of aspirin.
3. Methods
This case-control study was conducted in Sina hospital, an affiliated hospital of Tehran University of Medical Sciences, in 2018. The inclusion criteria were as follows: A clinical diagnosis of BPH and LUTS (International Prostate Symptom Score > 8), unresponsiveness to oral medications, undergoing treatment with aspirin, prostate size of 30 to 50 cc on transabdominal ultrasonography examination, and low-risk for cardiovascular events according to Goldman’s cardiac risk index. Also, cases with elevated prostate-specific antigen (PSA) or abnormal digital rectal examination (DRE) were assessed with trans-rectal ultrasound-guided prostate biopsies for ruling out prostate cancer. The exclusion criteria included end-stage renal disease, receiving anticoagulant medications, and cirrhosis. Eligible candidates were enrolled in the study and randomly assigned to two groups. In the first group, aspirin was discontinued one week before the surgery (monopolar TURP) and resumed upon discharge from the hospital (off-aspirin). In the second group, the surgery was performed without discontinuation of aspirin (on-aspirin). All surgeries were conducted under general or spinal anesthesia by surgeons who had passed their learning curve in TURP. A 22- or 24-F Foley catheter was inserted at the end of the procedure for all patients. The length of hospital stay, hemoglobin loss rate, need for blood transfusion, duration of Foley catheter fixation, the incidence of cardiovascular complications (Troponin I rise and chest pain), and secondary hemorrhage up to one month were recorded for each patient. Secondary hemorrhage was defined as bleeding between 72 hours and 30 days postoperatively. Blood transfusion was used for patients with Hb < 10 (24 h after the operation). The Foley catheter was removed after hematuria was resolved. Cardiac complications were defined as chest pain and raised Troponin I confirmed by a cardiologist. Data analysis was conducted via IBM SPSS for Windows, version 22 (IBM Corp., Armonk, N.Y., USA). Statistical significance was considered as P value < 0.05. Descriptive analysis was presented as frequency, percentage, mean, and standard deviation. The normality of data was evaluated with the Shapiro-Wilk test. To compare the two groups in terms of quantitative variables, Student’s t-test and ANOVA were used. The comparison of qualitative variables was made by the chi-square test.
4. Results
The study evaluated 132 patients, with a mean age of 64.11 ± 5.27 and 63.88 ± 4.41 years in the off-aspirin and on-aspirin groups, respectively. The mean prostate volume was 41.63 ± 5.81 ml in the first group, while it was 44.37 ± 5.42 ml in the second group (Table 1).
| Variable | Off-Aspirin | On-Aspirin |
|---|---|---|
| Age (y) | 64.11 ± 5.27 | 63.88 ± 4.41 |
| PSA (ng/dL) | 2.06 ± 1.39 | 2.17 ± 1.14 |
| Prostate Volume (cc) | 41.63 ± 5.81 | 44.37 ± 5.42 |
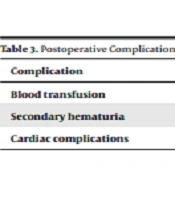
The Hb decline rate, hospital stay length, and Foley catheter fixation duration are summarized in Table 2. The analysis showed a significantly lower rate of Hb decline, duration of hospitalization, and Foley catheter fixation duration in the first group (off-aspirin) than in the second one (on-aspirin) (P < 0.001). No patient needed a blood transfusion in the first group, while it was necessary for two patients (3%) in the second group (Table 3). Nevertheless, the difference was not significant (P = 0.150). Six (9.1%) patients experienced secondary hematuria in the first group, while only one (1.5%) patient was involved with this complication in the second group. Although there was a trend toward the first group regarding the occurrence of secondary hematuria, this trend did not reach statistical significance (P = 0.052). Cardiac complications were not observed in any patient in the second group, while two (3%) patients in the first group suffered from these problems. These results revealed no significant difference between the two groups regarding cardiac complications (P = 0.154) (Table 3).
| Variable | Off-Aspirin | On-Aspirin | P Value |
|---|---|---|---|
| Hb decline | 1.68 ± 0.40 | 2.46 ± 0.60 | < 0.001 |
| Duration of hospitalization | 1.15 ± 0.36 | 1.69 ± 0.60 | < 0.001 |
| Duration of Foley catheter fixation | 1.63 ± 0.64 | 2.10 ± 0.78 | < 0.001 |
| Complication | Off-Aspirin | On-Aspirin | P Value |
|---|---|---|---|
| Blood transfusion | 0 (0%) | 2 (3%) | 0.150 |
| Secondary hematuria | 6 (9.1%) | 1 (1.5%) | 0.052 |
| Cardiac complications | 2 (3%) | 0 (0%) | 0.154 |
5. Discussion
Our study was conducted to assess the impact of aspirin continuation or discontinuation on TURP outcomes. Our results showed that the discontinuation of aspirin can significantly lower blood loss, hospital stay, and Foley fixation duration. The postoperative complications did not differ between the two groups.
The majority of patients with BPH are elderly, and due to the high rates of cardiac diseases in old ages, they are usually on aspirin treatment. Three decades ago, two reports of death following prostatectomy in aspirin users raised concerns regarding the clinical benefits and safety of aspirin in the perioperative period. Researchers tried to figure out whether it is a good choice to continue aspirin when the patient is a candidate for TURP or not. The studies revealed conflicting results on this issue, and the controversy is still going on. The consensus of UK urologists is that antiplatelet therapy increases the amount of blood loss, and thus, for a large number of patients, antiplatelet therapy must stop before surgery (11, 12).
A study on 136 patients undergoing TURP showed that the risk of hemorrhage in patients receiving aspirin was 50% versus 14.2% in patients not receiving aspirin. Two deaths also occurred in the aspirin group (4). Wierad et al. also reported significantly higher risks of bleeding with aspirin in the post-TURP period. In that study, 99 patients receiving aspirin required 42 units of blood, while 358 patients without aspirin treatment received 68 units of blood in total (13). In another case-control study, operative blood loss was the same in both ASA and placebo groups, but postoperative blood loss was significantly higher in the ASA group. Hospital stay duration after TURP was not significantly different between the ASA and control groups (14). For a more precise conclusion of studies, a systematic review on 49,590 patients undergoing non-cardiac surgeries revealed that aspirin in TURP was associated with a significantly higher risk of needing transfusion up to 2.7 folds compared to non-aspirin receivers (15).
On the other hand, Ehrlich et al. conducted a randomized clinical trial on the initiation of aspirin after TURP. Two groups of early (24 hours after operation) and late (three weeks after surgery) initiation of aspirin were evaluated. Postoperative bleeding, time to catheter removal, and hematuria duration were the same in both groups. Three cases of cardiovascular complications all occurred in the early group. This study concluded that the early initiation of aspirin did not negatively affect operative outcomes (16). Another study by Ala-Opas et al. on 40 patients on aspirin treatment and 42 controls showed that operative blood loss was the same, and post-TURP blood loss was not correlated with aspirin use (17). Another study by Haghro et al. assessed 105 TURP patients in two groups of aspirin receivers and controls. No significant difference was observed between the groups in intraoperative blood loss, hemoglobin level drop, hematocrit drop, and blood transfusion (18).
The current study found that although aspirin is a risk factor for blood loss after TURP, it does not have any effect on the blood transfusion rate. The study also showed that the continuation of aspirin might prolong hospital stay and catheter fixation duration, but it does not decrease cardiovascular complications. We also concluded that although secondary hematuria was more common in the aspirin group, no statistically significant association was observed.
There were some limitations to this study. The most important limitations were the relatively small sample size and inclusion of patients with low risk of cardiovascular diseases. To get more valid results, we suggest that future studies be conducted with a larger sample size and patients with high cardiovascular risks.
5.1. Conclusions
According to our results, discontinuation of aspirin does not increase cardiovascular disease in low-risk patients. Thus, aspirin could stop preoperatively. Due to our study limitations, the decision about higher-risk groups should be made based on more comprehensive studies.